“You could fry an egg on it” is how one patient with psoriatic arthritis (PsA) described her skin flare in a 2015 study. Affecting up to one-third of people with the inflammatory skin condition psoriasis, psoriatic arthritis is a double-whammy that has the hallmarks of both psoriasis (skin rashes) and inflammatory arthritis (joint pain). These painful symptoms may increase at certain times, called flares or flare-ups.
Science hasn’t come as far in understanding psoriatic arthritis flares as it has with other types of inflammatory arthritis, such as rheumatoid arthritis.
“Flares are one of the toughest things to pin down because there’s no real set definition a flare, which could mean different things to different people,” says Elaine Husni, MD, MPH, a rheumatologist at Cleveland Clinic. Because of this, it can be hard for patients — especially those recently diagnosed with psoriatic arthritis — to know when it’s happening.
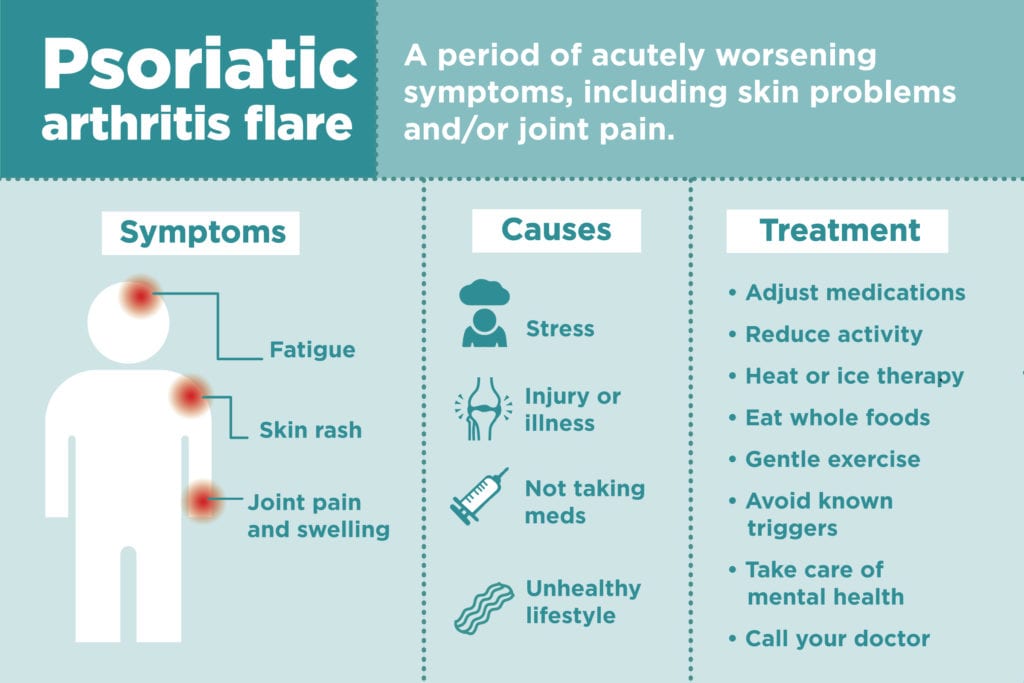
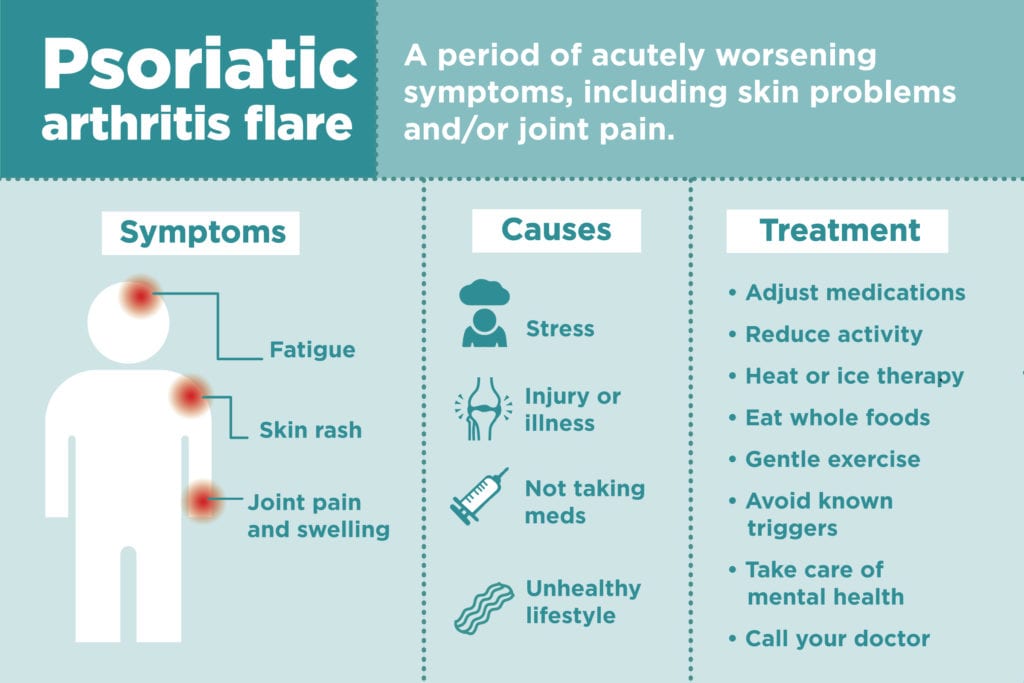
“The line between an official ‘flare-up’ and the normal waxing and waning of symptoms is definitely a difficult and confusing determination for many patients to make,” says occupational therapist Cheryl Crow, MOT, OTR/L, an adjunct faculty member of the Occupational Therapy Assistant program at Lake Washington Institute of Technology and an American Occupational Therapy Association spokesperson. “At the most basic level, a flare-up is a period of acutely worsening symptoms; however, for psoriatic arthritis, the symptoms may differ from patient to patient.”
What actually triggers a PsA flare in the body is also largely unknown. “We wish we knew — if we knew we could stop the flares,” Dr. Husni says. In addition, triggers can vary widely from person to person and even change throughout your life, Crow says. More research on psoriatic arthritis flares is sorely needed, but here’s what we know so far.
Symptoms of a Psoriatic Arthritis Flare
Joint pain and swelling
As with other types of inflammatory arthritis, an increase in joint problems may signal a flare is coming on. “Sometimes the joint swells, it gets more red, it gets more achy,” says Dr. Husni.
Skin rash
Fortunately (or unfortunately), psoriatic arthritis flares sometimes come with a “visual clue,” says Dr. Husni. “A skin flare would be an increase in skin symptoms, so thicker, redder plaques forming in new areas after having a period of being quiet,” she says. “Sometimes it’s helpful to have multiple organ systems affected to give you clues of what might be happening.”
But to make thing more complicated, Dr. Husni says that joint flares and skin flares in psoriatic arthritis are often separate. “They probably do flare at different times — but for some people they do flare at the same times, so it’s really variable, which makes the flare even harder to define,” she says.
Fatigue and mental problems
The 2015 study on PsA flares in the journal Rheumatology also found invisible symptoms such as fatigue and depression. “Some people say in addition to the joint and skin symptoms, you can also feel more tired or it might be more difficult to concentrate, but it’s unlikely that a flare occurs without the skin and the joint symptoms,” Dr. Husni says. “So if you’re all of a sudden feeling really depressed and there are no changes in your joints or your skin, it may be hard to blame it directly on a flare, although it still could be part of the disease process.”
Lasts at least a few days
Dr. Husni also says that a psoriatic arthritis flare usually doesn’t go away after an hour or two. “If you get better right away we don’t really consider that a flare, which usually lasts over a couple of days or a week,” she says. But, if the symptoms are really severe, you should still call your doctor even if it’s only been a short time. “There’s no magic number of days or hours — it’s more of how it affects your activities of daily living,” Dr. Husni says.
Causes of Psoriatic Arthritis Flares
Stress
Stress is one of the most common triggers for flares. (Of course, just having a chronic illness is stressful in itself.) “I have a patient with four kids who gets a flare every time school starts up again,” Dr. Husni says. “So we make sure we have a plan in place a couple of weeks before her kids start school.”
Injury or Illness
Skin infections or injury can cause an eruption of symptoms at the site. Getting sick can also bring on a flare, as can pushing yourself too hard. “Sometimes people have a cold and that triggers it — and then in addition they can’t take their immunosuppressant medicationuntil they get better,” Dr. Husni says. Learn more about how to care for your skin with psoriatic arthritis.
Not taking meds on time
Even if you feel fine, it’s still important to take your medication as prescribed to prevent psoriatic arthritis from flaring up again. “Sometimes people miss some medication doses and they flare,” Dr. Husni says. “Then we look back with the patient to figure out why and they say, ‘Oh, I was a little late taking it.’”
Unhealthy lifestyle
Dr. Husni says smoking, eating fried or sugary foods, and being overweight can cause your psoriatic arthritis symptoms to become worse.
How Psoriatic Arthritis Flares Are Diagnosed
Because PsA flares don’t have a set definition, the diagnosis is made in large part through communication with your doctor. “The first thing we do is we look at the history: what’s been happening before the flare,” Dr. Husni says. “We want to know what the triggers are for your disease and we want patients to see the connection.”
A skin flare is a bit easier to identify, and a diagnosis would be made with a rheumatologist and dermatologist. “We work very closely with the dermatologist — it’s important that they are involved in the treatment decision,” Dr. Husni says.
PsA flare-ups can be so hard to pin down that both professionals we talked to suggested keeping a brief diary of your symptoms to help your doctor diagnose when they are happening, and why.
“I recommend that people keep a symptom diary over time so that they can keep track of the conditions that might have preceded their flares in their lifetime, so that they can respond more proactively in the future,” Crow says. “Unfortunately often it’s most clear in retrospect.” You can use our ArthritisPower app to track your symptoms and disease activity and share your results with your doctor.
How Psoriatic Arthritis Flares Are Treated
Adjust medications
There are two ways to treat flares: pharmacologic and non-pharmacologic, says Dr. Husni. “It depends on the severity of the flare. Sometimes your doctor will add a little medication for you for that flare until you get better and then go back to your normal treatment,” she says. “Or if that’s the third flare in three months, then I might have a talk about changing medications; but I don’t usually do it on the first flare.”
Reduce activity
Non-medical short-term treatments should be put in place as well. “Immediately we usually recommend activity modification: You have to destress and deactivate your life for a couple days,” Dr. Husni says. “It doesn’t mean you become a couch potato, but you look at your schedule and develop strategies — this might not be the time to volunteer for that event.” In addition, she says to immediately start to get enough good sleep, if you’re not already.
Manage pain
You can also use home remedies to ease pain during a flare. “You can use what we call ‘modalities’ for pain management, which include hot or cold packs depending on the advice of your medical team — the general recommendation is to use cold for acutely inflamed joints and heat for stiffness,” Crow says. “Additionally, if you are having a lot of pain in a specific joint or area, you might benefit from a splint or other specific assistive device which can be recommended by an occupational or physical therapist.”
How to Prevent Psoriatic Arthritis Flares
Identify your triggers
As you become more familiar with your disease patterns, you can identify what’s bringing on the flare and take measures to address it. “If your trigger is stress, then you can invest in stress management strategies such as seeing a counselor or therapist or taking a mindfulness class,” Crow says. “If your trigger is getting a virus, you can boost your infection control measures; most patients who are on immunosuppressants for PsA understand they should wash their hands, but many forget the other small steps they can take to avoid illness, such as not touching their face and eyes. If your trigger is skin lesions or other skin traumas, then doing your best to avoid those would be very beneficial.”
Modify your lifestyle
For an overall reduction in psoriatic arthritis symptoms, Dr. Husni says to make sure you’re living a healthy life: stop smoking, cut back on alcohol, eat heathy, exercise and lose weight. “Weight is really hard to talk about, but it can really help the joints when you have decreased weight,” she says. “It’s like carrying a 10-pound book bag around with you all the time — when you don’t have to do it you feel so much better.”
With eating habits, Dr. Husni says it’s most important to consume nutrient-dense foods, rather than going on a “pop culture” diet like gluten-free. “If there are certain foods that trigger you then you should avoid them, but we always recommend a very colorful plate and to put a variety of non-processed foods on the table,” she says.
Employ some life hacks
Crow also advises taking shortcuts that can make living with PsA flares easier. “These life hacks can help minimize fatigue or joint pain,” she says. “If your joints hurt, you can change the stuff you are using in your daily life; for example, if your hands hurt, you can use a wide-grip fork while eating. You can also change how you interact with stuff, such as choosing to have grocery delivery rather than exerting the energy required to go to the store and bag all the items yourself.”
Take care of your mental health
Managing the mental aspect of psoriatic arthritis is an important treatment component as well. “People with psoriatic arthritis are at a greater risk of anxiety and depression than the general population, and flare-ups are difficult for many to cope with,” Crow says. “Whatever you can do to invest in your mental health is likely a wise choice.”
Call your doctor
As you become more familiar with your flares, you can work out a plan with your doctor for when you can self-manage and when you need to call, Dr. Husni says. But when it doubt, it’s better to reach out. “Patients with chronic diseases tend to get habituated to pushing through pain, and sometimes are tempted to wait a long time before checking in with their doctors,” Crow says. “It’s often harder to control a flare-up once it’s gotten really severe, so checking in proactively is usually advised.” Even for established patients, a flare after not having one for a while may signal a progression of the disease, so it’s best to check in.
Get to know your disease
The positive news is, living with PsA can become manageable as you figure out how it affects you. “If the disease is new to you or early to you, flares are much more uncertain and scary,” Dr. Husni says. “Once you’ve had it for a longer period of time, flares become a lot less scary. This is a good time to have psoriatic arthritis because there are a lot of treatments available, more than we ever had before.”
Audio Guide: Understanding Healthy Lifestyle Changes for Psoriatic Arthritis
Learn more about healthy lifestyle changes for psoriatic arthritis and how lifestyle changes and medication work together to help you manage your condition. For more audio guides and insights from PsA experts, check out the Psoriatic Arthritis Club podcast.





