Diagnosing someone with axial spondyloarthritis (axSpA), an autoimmune form of arthritis that causes chronic back pain, can be tricky. (AxSpA is considered an earlier stage of ankylosing spondylitis.) Part of the problem is that there are so many other (and much more common) conditions can cause back pain.
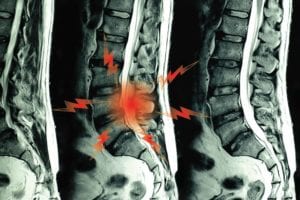
One key distinction that clinicians tend to focus on is the fact that, in axSpA, the sacroiliac (SI) joints that connect the lower spine to the pelvis will eventually deteriorate if the condition isn’t treated.
To figure out if someone has axSpA, rheumatologists often take X-rays, but you could be living with the condition for up to a decade before the SI joints deteriorate enough for the change to be visible on an X-ray. Could relying on MRIs — which are more costly but produce much clearer images — be the answer? Unfortunately, recent studies suggest that’s not the case.
One recent study, published in September in Arthritis and Rheumatology, involved 188 people who had chronic back pain as well as at least one other feature that suggested they likely had axSpA. (These are symptoms of ankylosing spondylitis to be aware of.) Patients had MRIs when the study began, three months later, and at the one-year mark.
Most of the group had no visible signs of SI joint damage on baseline MRIs. A year later, not much had changed: Only 7 percent of those who started out without evidence of SI joint erosion had developed it based on the MRIs taken a year later, even though clinicians were fairly confident that the people had axSpA.
“The usefulness of repeating an MRI [of the SI joints] in the diagnostic process after three months or one year is very limited,” wrote the authors, who are based Leiden University Medical Center in the Netherlands.
Another study, published in January in Rheumatic and Musculoskeletal Diseases, came to a similar conclusion: “MRI by itself cannot serve as the gold standard to make a diagnosis of early [axSpA] due to limitations both in sensitivity and specificity.”
Where Does This Leave Patients Eager to Get a Definitive Diagnosis?
That’s not entirely clear, but these findings aren’t necessarily bad news, either, as rheumatologist Bharat Kumar, MD, explained in commentary for MedPage Today: “Although this may sound disappointing, it comes as a relief,” writes Dr. Kumar. “MRI scans are expensive and can unintentionally pick up abnormalities that may not have any clinical significance. On the other hand, use of clinical examination methods, like careful history taking and relevant physical examination, may be more helpful in guiding therapies.”
In summary, there are no diagnostic shortcuts here, but working closely with an experienced rheumatologist can get you on the path to feeling better and stopping further joint damage — no matter what’s visible (or not) on an imaging test.
Keep Reading
- Mechanical vs. Inflammatory Back Pain: What’s the Difference?
- How Doctors Diagnose Ankylosing Spondylitis: What to Expect at the Rheumatologist
- 4 Factors That Delay Getting Diagnosed with Axial Spondyloarthritis Even Longer Than It Already Takes





