Ankylosing spondylitis is a type of inflammatory arthritis that causes inflammation, pain, and stiffness — predominantly in the lower back and sacroiliac joints (where the spine meets the pelvis). What’s behind the inflammation: Your body’s immune system is releasing chemicals into your blood and joints that cause pain, stiffness, and eventually joint damage.
Compared with many other forms of arthritis, AS symptoms usually begin young: before age 45, and often as early as the teens and twenties. The lower back pain is worse after inactivity or when you wake up. It can present as an ongoing, dull pain that feels like it is coming from deep within the lower back or buttocks. Because back and hip pain are incredibly common, it’s easy for people with inflammatory back pain from AS to chalk up their symptoms to other issues, such as athletic or overuse injuries. AS symptoms aren’t limited to the lower back; the disease can also affect the neck and peripheral joints such as the shoulders and knees.
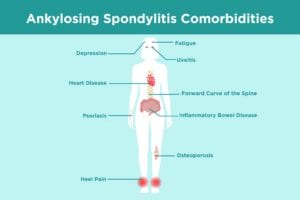
While chronic inflammatory lower back pain is a telltale symptom of ankylosing spondylitis, the disease can have a wide-ranging impact on patients’ health and well-being. The inflammation and joint damage of AS are linked with a number of additional comorbidities and complications that it’s important for patients and doctors to be aware of and proactively try to prevent or manage.
That’s why early diagnosis and treatment of ankylosing spondylitis is critical. Treatment aims to reduce pain and symptoms, help you maintain normal posture, reduce complications and comorbidities, prevent permanent damage, and improve your quality of life.
“I explain to my patients that in some — but not all — cases, an ankylosing spondylitis diagnosis leads to progressive stiffness and sometimes fusion of the joints of the spine,” says Eric M. Ruderman, MD, professor of medicine/rheumatology at Northwestern University’s Feinberg School of Medicine in Chicago. “While we don’t yet have treatments that definitively prevent this progression, medications can reduce or eliminate the pain and stiffness, allowing patients to be more functional. In addition, I talk to them about exercises and stretching that can help maintain mobility.”
Commonly prescribed medications for AS include non-steroidal anti-inflammatory drugs (NSAIDs) and different classes of biologics, which are targeted drugs that act on immune system pathways to reduce inflammation.
Once you read through this list of ankylosing spondylitis complications, bring up any questions or concerns you have with your doctor. You may need to create a health care team of different specialists — such as a cardiologist or ophthalmologist — or facilitate better communication between them to ensure you’re getting optimal care for your ankylosing spondylitis and its complications and comorbidities.
Common Ankylosing Spondylitis Comorbidities and Complications
Ankylosing Spondylitis and Forward Curve of the Spine
Ankylosing spondylitis can cause an overgrowth of the bones in your spine. That can lead to fusion, which is an abnormal joining of the bones. “By definition, ankylosing spondylitis affects the sacroiliac joints in the pelvis first and then marches its way up the spine,” says Maureen Dubreuil, MD, assistant professor of rheumatology at Boston University School of Medicine who specializes in spondyloarthritis. “It may not follow that exact pattern. But you can have involvement at any part of the spine — the neck, rib cage, lumbar spine.”
In the past, people with AS would develop significant changes in their posture over time, such that they looked hunched over, a condition known as kyphosis. However, that’s changed for people more recently diagnosed with AS, thanks to better therapies. “Some fusion is fairly common,” says Dr. Ruderman. “But progressive fusion that leads to kyphosis isn’t very common,” says Neal Birnbaum, MD, a rheumatologist, former president of the American College of Rheumatology, and founder of Pacific Rheumatology Associates Medical Group in San Francisco. “Fortunately, biologic therapies have made this a very uncommon occurrence.”
Early diagnosis and treatment of AS can help prevent fusion in the spine. “A goal of treatment is to prevent fusion from happening,” says Dr. Dubreuil. “We really want to stop this disease before it causes permanent damage.” In addition to biologics, regular exercise and physical therapy can help prevent posture changes, says Dr. Dubreuil. In PT for ankylosing spondylitis, you’ll do neck and spine extension work to prevent hunched-over posture.
Ankylosing Spondylitis and Osteoporosis
Osteoporosis, a silent condition that weakens your bones and makes them more susceptible to fractures, is a frequent complication of ankylosing spondylitis. According to the American College of Rheumatology, osteoporosis occurs in up to half of patients with ankylosing spondylitis, especially in those whose spine is fused.
A case study published in the journal Clinical and Experimental Rheumatology compared bone density scans of about 500 AS patients to healthy people without AS. About 10 percent of AS patients had osteoporosis compared with 0 percent of the control group. Nearly 60 percent of AS patients had osteopenia, a precursor to AS; just 34 percent of the control group did.
Interestingly, osteoporosis is considered more of a “woman’s disease” and AS is considered more of a “man’s disease.” However, we know AS affects women much more than previously thought. It’s important for women with AS to be aware of this additional osteoporosis risk factor, and for men with AS to keep osteoporosis on their radar.
Because osteoporosis is often asymptomatic (it rarely causes symptoms until a bone fracture occurs), you may have bone issues and not even know it. Talk to your rheumatologist and primary care health care provider about how often to get bone density scans, which can help determine if you have osteoporosis before you experience a fracture.
Screening for low bone mass density with a standard bone density scan within one year of diagnosis of ankylosing spondylosis is advisable, found a study in Current Treatment Options in Rheumatology. Your health care provider can advise what’s right for you, given your family history and other personal risk factors.
When you do get screened for osteoporosis and you have AS, “it’s important to perform the bone density scans on your wrist and hip,” says Brett Smith, DO, a rheumatologist with Blount Memorial Physicians Group in Alcoa, Tennessee. “The increased bone formation in the spine [as a result of AS disease activity] can result in inaccurate results.”
Prevent bone loss by doing weight-bearing exercises as well as taking calcium, vitamin D, or osteoporosis medications to prevent bone loss or re build bone.
Ankylosing Spondylitis and Uveitis
As many as 40 percent of people with ankylosing spondylitis may experience a kind of inflammation of the eye called uveitis, according to the American College of Rheumatology. Uveitis causes swelling of the uvea, the layer of tissues in the middle of your eye beneath your cornea. Uveitis symptoms include redness, eye swelling, eye pain, watery eyes, blurred and impaired vision, and sensitivity to light. Uveitis is usually present in only one eye at a time, says Dr. Birnbaum. It typically comes on suddenly and becomes severe quickly. The condition can lead to cataracts, glaucoma, or even vision loss if left untreated.
Uveitis happens because ankylosing spondylitis is a systemic disease, which means the inflammation that impacts the joints in your spine also affects tissues in your eye.
Steroid eye drops often are effective at helping reduce the inflammation in your eye. “If it’s mild, simple drops are sufficient,” says Susan Goodman, MD, a rheumatologist at the Hospital for Special Surgery in New York City. If the drops don’t work, you may need corticosteroid pills or steroid eye injections. While uveitis is being treated, you can also wear dark glasses so that bright lights don’t bother you.
Recurrent bouts of uveitis may mean you need an AS treatment change. If you’ve been taking non-steroidal anti-inflammatory meds but experience complications like uveitis, it may be a sign you need to escalate to a biologic drug.
When you have AS, it’s important to visit an ophthalmologist at least annually to get your eyes checked. See an eye doctor promptly if you develop any unusual vision changes or eye symptoms.
Ankylosing Spondylitis and Inflammatory Bowel Disease
Inflammatory diseases travel in packs. Inflammation from AS can also strike the intestinal tract, which makes such diseases as Crohn’s disease and ulcerative colitis common among ankylosing spondylitis patients. In fact, between 5 percent and 10 percent of cases of ankylosing spondylitis are associated with inflammatory bowel disease, according to a study in the journal Best Practice and Research: Clinical Rheumatology. Some two-thirds of people with ankylosing spondylitis have bowel inflammation without symptoms that is seen only on colonoscopy, according to research in the British Journal of Rheumatology. Sometimes people don’t even realize that they have inflammatory GI issues since they’re experiencing so much back pain.
It’s unclear why ankylosing spondylitis is linked to inflammatory bowel disease. “We’re really just beginning to understand why these two things are connected,” says Dr. Dubreuil. One possible explanation is that there’s a change in gut bacteria that leads to inflammation that affects both the GI tract and the joints in the spine and elsewhere in the body.
Symptoms of inflammatory bowel disease include chronic diarrhea, blood in the stool, stomach pain and cramping, and other digestion problems. If you have these symptoms, you may need a colonoscopy to see what’s happening in the GI tract.
Biologic medications used to treat ankylosing spondylitis may also be beneficial in managing ulcerative colitis or Crohn’s disease. If you have inflammatory bowel disease, a gastroenterologist can work with you and your rheumatologist on a treatment plan. In addition to medication, they may suggest tweaks to your diet, such as limiting dairy; eating low-fat foods (avoid butter, creamy sauces, and fried foods); and restricting high-fiber foods, depending on your condition.
Ankylosing Spondylitis and Psoriasis
Psoriasis is an autoimmune disorder characterized by red, itchy, silvery, and scaly patches on the skin. Psoriasis is known to co-occur with ankylosing spondylitis: Inflammatory spinal disease develops in some 5 percent to 25 percent of psoriasis cases.
If you have skin changes that you suspect could be psoriasis, talk to your rheumatologist. They will likely refer you to a dermatologist, who will examine your skin, nails, and scalp for signs of the condition.
Your dermatologist and rheumatologist can work together on a treatment plan to address both psoriasis and AS. Psoriasis may be treated with topical medications (like corticosteroids), phototherapy (which uses ultraviolet or natural light), systemic treatment (like methotrexate), or a combination approach. Some biologic medications may help treat both psoriasis and AS.
Ankylosing Spondylitis and Heart Disease
People with ankylosing spondylitis may be at an increased risk of developing certain heart problems, likely due to a combination of factors such as inflammation and lack of exercise due to symptoms like pain and stiffness. Medications used to treat ankylosing spondylitis can play a role as well. While NSAIDs may increase cardiac risk, TNF inhibitor biologics can help decrease inflammation and cardiac risk.
One heart complication AS patients need to know about is aortic valve disease, though it is considered rare. The aorta is the main artery in the heart that sends blood from your heart to the rest of your body. Inflammation in the aorta, called aortitis, can harm the aortic valve, which helps blood flow in the correct direction. In aortic valve disease, blood regurgitates back into the heart rather than flowing forward to the rest of the body. In ankylosing spondylitis, the usual problem is a leaky valve, known as aortic insufficiency. Medications such as anti-TNF biologics may help control inflammation in the aorta, says Dr. Birnbaum. A damaged aortic valve sometimes requires surgical repair or replacement.
Patients with ankylosing spondylitis should get the same heart protective tests, treatments, and protocols as the general population, says Dr. Dubreuil. Stop smoking; its chemicals can damage the lining of your arteries and contribute to plaque buildup that can cause heart attack or stroke. If you’re overweight, lose weight. Extra pounds strain your heart and put you at higher risk of high cholesterol and blood pressure. Control conditions like diabetes that can damage your blood vessels and heart. Exercise regularly to strengthen your cardiovascular system.
If you’re on NSAIDS to treat your AS, it’s important to get your blood pressure checked regularly. These medications can increase blood pressure, says Dr. Dubreuil.
Ankylosing Spondylitis and Depression
Recent research published in the journal Scientific Reports found that having AS more than doubles the risk of depression. This may be related to the disease process itself. People with chronic inflammatory disease tend to have high levels of immune system proteins called cytokines, which trigger inflammation and may also contribute to depression. AS patients may also experience depression and anxiety because of how the disease and its symptoms are affecting quality of life and the ability to work and socialize.
“Depression complicates the treatment of any rheumatic disease,” says Dr. Dubreuil. Patients are upset with their inability to do what they once could do. They have a reduced quality of life thanks to their pain. “People with untreated depression may continue to feel pain, even when their ankylosing spondylitis is controlled. This makes it hard to determine if the medications for ankylosing spondylitis are working.”
Symptoms of depression include loss of interest in activities you once enjoyed; persistent helplessness, hopelessness, or sadness; sleep pattern changes; difficulty concentrating; and withdrawing from your circle of friends.
Talk with your rheumatologist or primary care provider to see if you need medication to treat depression (which can help reset the chemicals in your brain). Exercising also helps release endorphins, which can boost your mood as well as keep your joints flexible and mobile.
Ankylosing Spondylitis and Heel Pain
When you have ankylosing spondylitis, you can have pain and tenderness in spots where soft tissues meet bone, which is known as enthesitis. “Enthesitis [where tendons or ligaments insert into the bone] is a common symptoms of ankylosing spondylitis,” says Dr. Goodman. “However, it’s also common in the general population and doesn’t raise suspicion unless another symptoms like arthritis or uveitis develop.”
People with ankylosing spondylitis commonly have Achilles tendonitis (at the back of the heel) and plantar fasciitis (at the bottom of the foot).
The same medications that manage AS inflammation (NSAIDs and biologics) should also help alleviate enthesitis.
To manage enthesitis, wear supportive, soft-soled shoes. Although it may hurt to walk, exercise is important. “Exercise and stretching are excellent ways to alleviate stiffness and pain,” says Dr. Goodman. Physical therapy can be helpful, too, in teaching you techniques to lessen your pain.
Ankylosing Spondylitis and Fatigue
Fatigue, which is full-body exhaustion (not just feeling tired from lack of sleep), is a common complaint of many chronic illnesses. Ankylosing spondylitis is no exception. You’re just too exhausted and weak to function like your usual self. Fatigue is physical, not just mental, exhaustion. One study found that about 65 percent of ankylosing spondylitis patients report fatigue as a symptom. Some ankylosing spondylitis patients say their fatigue is as bad as — if not worse than — the pain.
With AS, cytokines (inflammatory markers) are circulating in your body and your body is using energy to calm this inflammation, which causes fatigue. This inflammation, as well as cycles of flares, poor sleep, and stress from AS are also to blame for fatigue.
Higher levels of fatigue are associated with a worse performance at work and more activity impairment among ankylosing spondylitis patients, according to a study in the journal Arthritis Research & Therapy. The research found that fatigue is an AS symptom that has often been ignored, but it’s an important one.
Treating AS inflammation with biologics may help improve fatigue and restore energy levels. Regular exercise such as swimming, biking, or yoga can also help relieve fatigue.
“Exercise is an important part of treatment for anyone with fatigue,” says Dr. Dubreuil. Physicians should also see if fatigue could be due to other causes, such as anemia, sleep apnea, or suboptimal pain management. If patients are waking up at night in pain, their medication may need to be adjusted to help control pain. “We assess medications to see if they’re doing their job or they need to be changed,” she says.