Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
This has been reviewed and updated as of July 30, 2020.
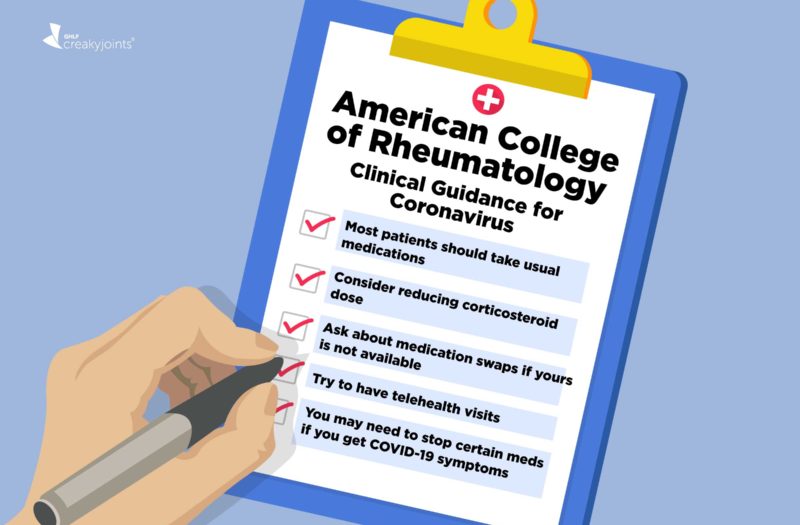
When the COVID-19 pandemic first started, rheumatologists were making their own best guesses based on experience with prior infectious diseases (such as the seasonal flu, swine flu, and SARS) and advising patients accordingly. That changed in April when the American College of Rheumatology (ACR) issued a clinical guidance document designed to inform rheumatologists across U.S.
In July, the organization issued an update to this document — and it probably won’t be the last one.
Because this coronavirus strain is such a new virus, information about it is rapidly developing. In light of this, the authors noted that new clinical guidance document is not the final word on the subject; rather, it should be considered a “living document” that will be updated as new studies and reports from physicians continue being released. They also emphasized the importance of personalized treatment and shared decision-making between patient and provider.
With that in mind, here are some key highlights patients should know about:
Most patients should continue taking their usual medications
If you don’t have COVID-19 and are stable on your current regimen, it’s generally wise to stick with it. That includes continuing to use:
- Hydroxychloroquine or chloroquine
- Sulfasalazine
- Methotrexate
- Leflunomide
- Immunosuppressants (such as tacrolimus and cyclosporine)
- Biologics
- Janus kinase (JAK) inhibitors
- Non-steroidal anti-inflammatory drugs (NSAIDs)
If you take corticosteroids, such as prednisone, now may be a good time to wean off or reduce your dose
Corticosteroids increase your risk of infections — even more so than biologics. They also carry a long list of other side effects, which is why they’re not optimal for long-term use.
“This recommendation [to use corticosteroids at the lowest possible dose] is really intended to serve as a reminder to do what we should be doing anyway; that is, following best practices by using the lowest dose of steroids needed to control underlying inflammation,” says Ted Mikuls, MD, MSPH, chair of ACR’s COVID-19 Clinical Task Force. “However, any tapering or reductions should not come at the cost of poor rheumatic disease control.”
If the medication you normally take isn’t available, ask your doctor about making a swap
Certain medications, such hydroxychloroquine and chloroquine, may be harder to come by since some people still believe they may help treat COVID-19. If there’s a shortage in your area and you can’t get your usual medication, talk to your doctor.
Patients who normally use hydroxychloroquine but can’t access it may consider switching to a traditional DMARD like methotrexate, perhaps in conjunction with a biologic drug.
Look for ways to reduce in-person contact in health care settings
COVID-19 is highly contagious and can spread in health care settings like doctors’ offices and hospitals. To reduce your chances of being exposed (and of exposing other people if you could possibly be a carrier), your provider might suggest making some changes, such as seeing you by telehealth (phone and video) instead of in person. Assuming your condition is stable, you might also be advised to postpone your next appointment for blood tests or, depending on your geopgraphic area and the prevalence of COVID-19 there, to come in for infusion of IV medications less often.
“For all of the guidance generated, decisions have to be made on a case-by-case basis, as the risk of delaying some infusions may far outweigh benefit,” says Dr. Mikuls. “In other circumstances, such as a patient with well-controlled rheumatic disease — perhaps even in remission — slight delays in intravenous dosing might pose little to no risk. But in each instance, this is a decision that must be made as part of a collaborative exchange between the rheumatologist and patient.”
If you develop COVID-19 symptoms, your doctor might suggest taking a break from some medications
If you normally take hydroxychloroquine or chloroquine, you should continue taking it even if you develop infection symptoms.
But many other medications, including sulfasalazine, methotrexate, leflunomide, immunosuppressants, biologics, and Janus kinase (JAK) inhibitors should be stopped while you combat the virus.
Most people can restart these treatments seven to 14 days after their symptoms resolve, but you should always ask your rheumatologist for guidance.
Decisions regarding the timing of resuming medication in patients who are recovering from more severe cases of COVID-19 should be made on a case-by-case basis.
Some of these drugs interfere with your natural immune response, but “immunosuppression is only one part of the equation,” says Dr. Mikuls. He explains that some rheumatology treatments have side effects that can mimic problems caused by COVID-19 infection, and doctors need to be able to accurately monitor people who have been infected. “The downside of holding [rheumatologic] medicines for a brief duration while patients recover from COVID-19 is likely minimal in most instances,” he says.
People who test positive for COVID-19 but don’t develop any symptoms should also stop drugs that suppress the immune system or cause side effects that could mimic COVID-19 symptoms.
These drugs include sulfasalazine, methotrexate, leflunomide, immunosuppressants, biologics, and Janus kinase (JAK) inhibitors. If you remain asymptomatic, your doctor will likely advise you to wait 10 to 17 days after your positive test to resume these medication.
People with COVID-19 who develop severe respiratory symptoms should not use NSAIDs (like ibuprofen)
Some small studies and anecdotal reports have suggested that people who have used NSAIDs to treat pain and fever related to COVID-19 have gotten worse, but the evidence is scant. For that reason, “the panel demonstrated low consensus with regards to stopping NSAIDs in the absence of severe symptoms,” the authors wrote.
When in doubt, check with your provider. Some are advising patients who develop COVID-19 symptoms not to use NSAIDs.
Get Free Coronavirus Support for Chronic Illness Patients
Join the Global Healthy Living Foundation’s free COVID-19 Support Program for chronic illness patients and their families. We will be providing updated information, community support, and other resources tailored specifically to your health and safety. Join now.
COVID-19 Clinical Guidance for Adult Patients with Rheumatic Diseases. American College of Rheumatology. July 13, 2020. https://www.rheumatology.org/Portals/0/Files/ACR-COVID-19-Clinical-Guidance-Summary-Patients-with-Rheumatic-Diseases.pdf.
Interview with Ted Mikuls, MD, MSPH, chair of the American College of Rheumatology COVID-19 Clinical Task Force
Laday J. ACR: Patients can restart rheumatic treatments 7-14 days after COVID-19 symptoms resolve. Healio Rheumatology. July 23, 2020. https://www.healio.com/news/rheumatology/20200723/acr-patients-can-restart-rheumatic-treatments-714-days-after-covid19-symptoms-resolve.