While rheumatoid arthritis (RA) most commonly affects the peripheral joints — such as those in the hands, feet, and knees — some people with RA also report experiencing back pain.
Keep in mind, though, that if lower back pain is your primary symptom, it’s likely not due to RA. Several types of inflammatory arthritis affect the spine, most notably spondyloarthropathies such as psoriatic arthritis and ankylosing spondylitis, in which back pain is one of the main symptoms of the disease. (Read more about ankylosing spondylitis symptoms here, and about psoriatic arthritis symptoms here.)
To help demystify back pain among people with rheumatoid arthritis, we asked Marcy Bolster, MD, associate professor of medicine at Harvard Medical School and director of the Rheumatology Fellowship Training Program at Massachusetts General Hospital, to answer questions many RA patients have when they find themselves dealing with back pain.
How Does Rheumatoid Arthritis Cause Back Pain?
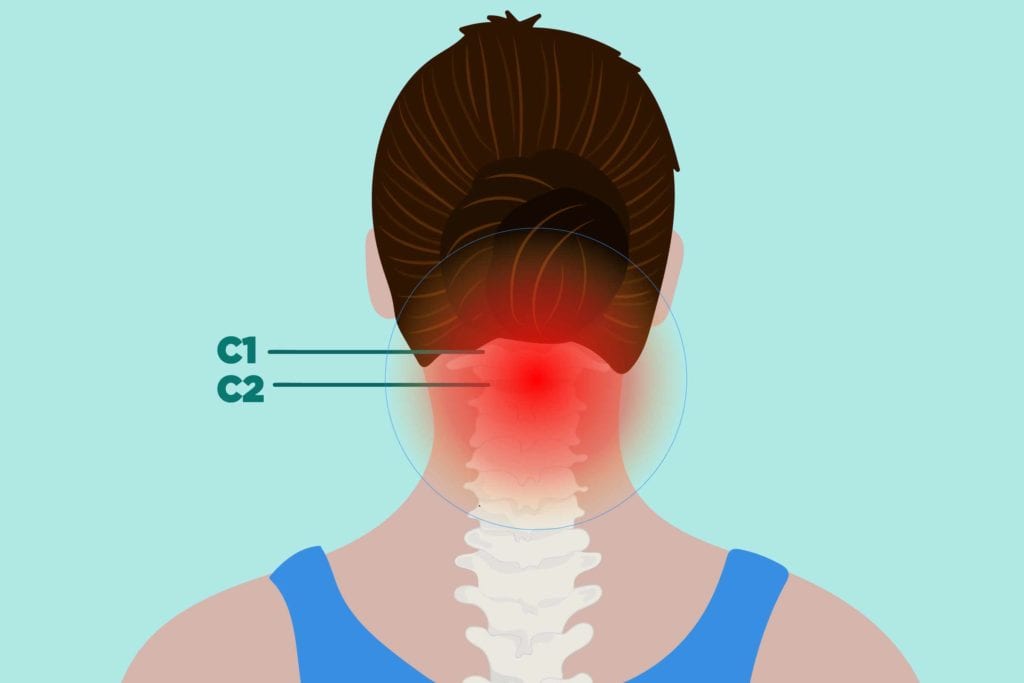
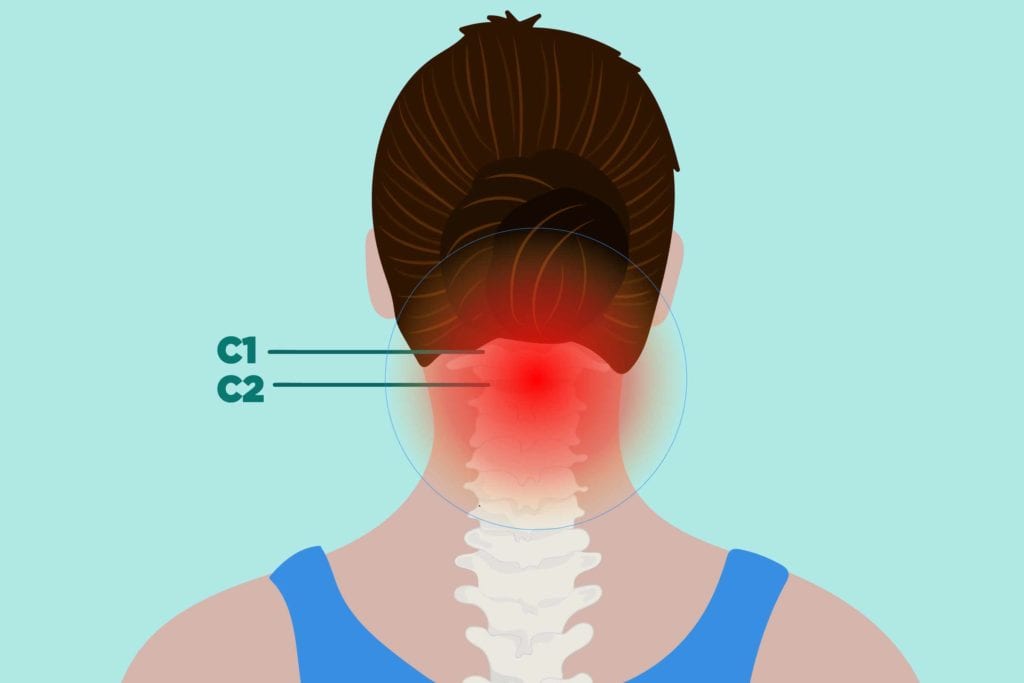
In terms of spine involvement, RA primarily affects the cervical spine, which is located at the top of the spinal cord and forms your neck. While it is possible for the middle or lower back to be affected, this is considered rare.
“If a patient with established RA comes to me with pain in the mid or lower back, I’m less likely to think their symptoms are directly related to RA,” Dr. Bolster says.
Here’s the reason that the cervical spine is more commonly affected: In RA, the immune system attacks the synovium, the thin membrane that lines your joints; it’s the main site of the inflammatory process in rheumatoid arthritis.
The spine’s top two vertebrae, C1 and C2, are synovial-lined joints, and are therefore subject to developing the inflammation and joint erosion you experience in your peripheral joints.
It’s unclear how many people with RA have cervical spine involvement. It typically develops in the later stages of RA, but Dr. Bolster says it has been reported earlier.
“My back pain started pretty quickly, within the first year of my RA diagnosis,” says CreakyJoints community member Lisa Powell, who experiences both cervical and lumbar back pain. “My doctor hasn’t totally ruled out that osteoarthritis might be the cause of the damage to my lower back, but the pain there seems very tied to my RA symptoms. It gets worse when my RA is flaring or isn’t well controlled.”
What Are the Long-Term Consequences of RA-Related Back Pain?
Middle or lower back pain is most often a mechanical issue, and does not occur because of RA. However, in some cases the disease can indirectly cause pain in the mid or low back. For example, severe pain in other joints could alter the mechanics of your gait, which could result in back pain over time.
“My neck has been affected the most by my RA, but my lower back also hurts, and I think that’s caused by the pain in my hips and knees,” says CreakyJoints member Mary Eldreth Pearson. “If I have to stand for longer than 30 minutes my lower back hurts more.”
RA may also indirectly affect the back because it increases a person’s risk of developing osteoporosis, Dr. Bolster says. While osteoporosis itself isn’t painful, it can result in insufficiency fractures of the vertebral bodies in the thoracic and lumbar spine.
“If someone with RA came to me with sudden onset of back pain, that could indicate a compression fracture of the spine, which occurs in people with osteoporosis,” she explains.
If RA Isn’t Causing Middle or Lower Back Pain, What Else Could Be to Blame?
Your rheumatologist will likely consider potential causes including:
- Osteoarthritis
- Degenerative disc disease
- Bulging disc
- Pinched nerve
- Spinal stenosis
- Conditions unrelated to the spine that can cause back pain (kidney stones or infections, for example)
How is RA-Related Back Pain Treated?
If you have C1 or C2 involvement, your rheumatologist may work in collaboration with a neurosurgeon to treat and monitor you, since surgery is sometimes necessary. However, surgery is reserved for more advanced cases where spinal instability has begun to put pressure on the spinal cord, and many people never reach this stage. So it’s more likely that your pain can be managed with non-invasive treatments.
To treat inflammation and slow joint erosion in the cervical spine, Dr. Bolster says that aggressive treatment of the underlying arthritis with disease-modifying anti-rheumatic drugs (DMARDs) is important.
DMARDs can help alleviate back pain by treating the underlying inflammation that may affect the cervical spine. NSAIDs, acetaminophen, and/or muscle relaxants are used to treat both the pain associated with cervical spine involvement by RA as well as for middle and lower back pain that people with RA can have, but that isn’t occurring becauseof RA. Your rheumatologist will also likely recommend other ways to keep back pain at bay.
“Physical therapy and exercise are important parts of treating back pain,” Dr. Bolster says. A physical therapist can teach you stretches and strengthening exercise, particularly core strengthening exercises, you can ultimately do at home, and your rheumatologist will likely recommend you perform low-impact workouts such as cycling and swimming. If you’re overweight, weight loss can benefit your back pain symptoms.
CreakyJoints member Dave Stinson says that while exercise hasn’t resolved his back pain, it has helped.
“I ride my bike, walk, and added regular stretching protocols to my routine, and I have high hopes for attending a yoga class in the near future,” he says. Revamping his diet and losing weight have also made a difference in managing his rheumatoid arthritis back pain. When his back bothers him, he treats it with ice, heat, and NSAIDs.
Powell also credits weight loss and exercise with easing her back pain from rheumatoid arthritis.
“I recently learned about an exercise technique called Egoscue, and my overall pain level has really improved ever since I started doing it,” she says. (The Egoscue Method targets postural issues that can cause pain.) “Between that, my weight loss, and finally finding a medication that controls my symptoms pretty well, I’m the closest I’ve ever been to remission in the eight years I’ve had RA.”
Your rheumatologist may also recommend assistive devices to alter the mechanics of your posture and gait to help manage your back pain. Pearson uses a cane, or sometimes a walker if necessary. Powell, a full-time student, says her doctor advised her to use ergonomic furniture to support her back when she has to sit for long periods.
“I registered with disability services at my university, and they provide me an adjustable-height table and an ergonomic chair for all my classes,” she says. “It’s been immensely helpful.”
Keep Reading
Subscribe to CreakyJoints
Get the latest arthritis news in your inbox. Sign up for CreakyJoints and hear about the latest research updates and medical news that could affect you.





