People living with arthritis are far more likely to have depression and anxiety than the general population. There are many reasons for this connection: physical pain causes depression and inflammation plays an underlying role in both conditions. And having pain and fatigue can negatively affect social relationships and cause loneliness.
The relationship between different kinds of arthritis and mental health issues like depression and anxiety is increasingly researched and recognized by doctors. But that doesn’t necessarily mean that critical conversations about mental health are happening between people living with arthritis and the doctors who treat them.
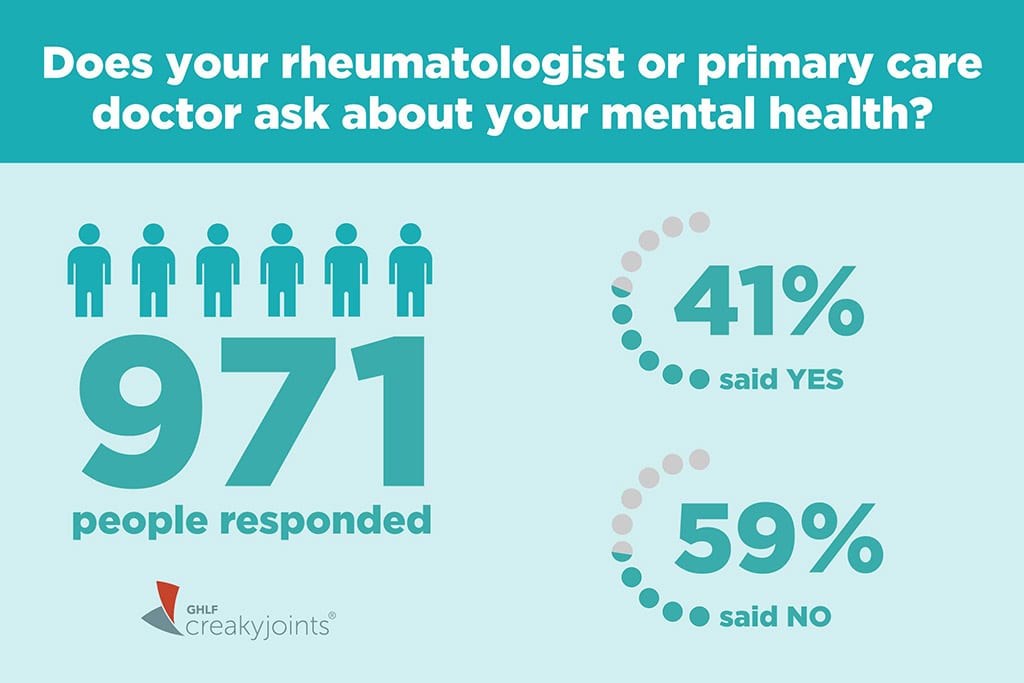
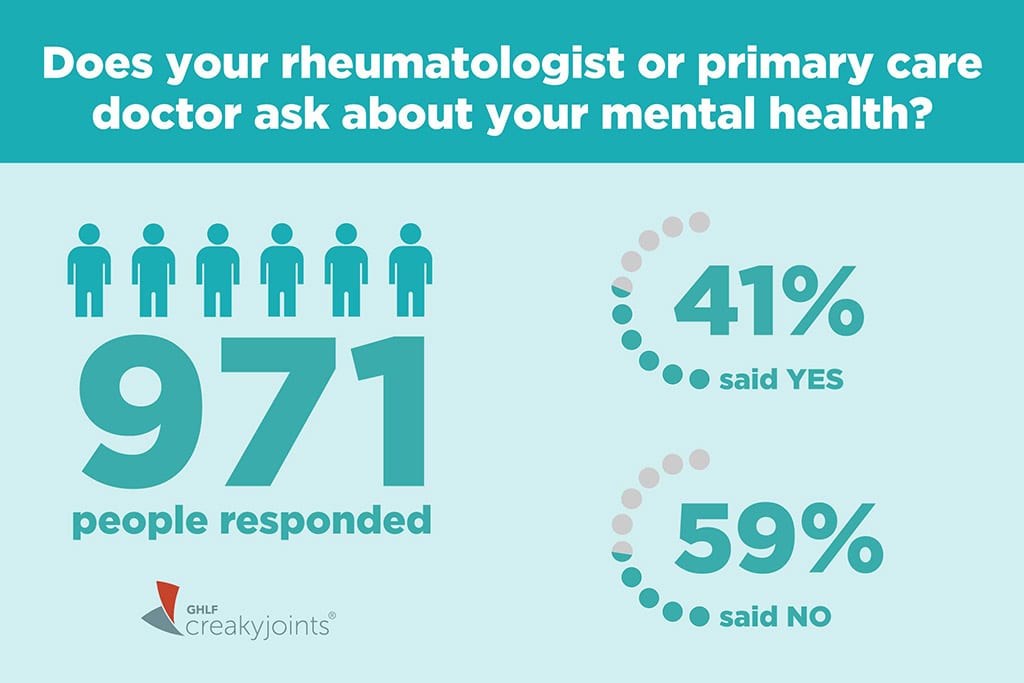
In fact, in an ArthritisPower Community Poll, we asked people if their rheumatologist or primary care doctor asks about their mental health. Of the 971 people who responded, 59 percent said no.
In a survey of rheumatologists published in the Journal of Clinical Rheumatology, authors concluded that while rheumatologists were aware that many of their patients were dealing with mental health issues, they “may lack the confidence, time, and/or referral networks to provide consistently effective care for depressed patients.”
Talking About Mental Health with Your Doctor
First, know that rheumatologists and primary care doctors are actively talking among themselves about how to provide better screening, diagnosis, referrals, and treatment for mental health issues among people living with arthritis. And these conversations are happening more frequently due to the mental toll the pandemic has taken on the rheumatic disease community.
“I think number one is normalizing it,” rheumatologist Alexis Ogdie, MD, Director of the Penn Psoriatic Arthritis Clinic, told CreakyJoints during an interview. “Having physicians just ask the question [about mental health] is remarkable in what that will do for you.”
She says that many patients think this conversation belongs in a primary care realm or that they should seek out a therapist or a psychiatrist or something on their own. And they’re not going to necessarily do that. “When I open the door and say, ‘This is really common in your disease,’ I think that makes it okay to talk about it. I think people are more comfortable.”
An article in The Rheumatologist, a publication for doctors, acknowledged that it’s not necessarily your rheumatologist’s job to treat depression, but your rheum should acknowledge the problem and help make a plan for more evaluation and management with either a primary care doctor or refer you to a specialist.
Starting the Conversation
If your doctor doesn’t ask about your mental health — and you’re concerned that you might be experiencing signs of depression or anxiety — bring it up yourself.
“Sometimes it doesn’t seem like there’s time and attention to these things in a medical encounter,” Adena Batterman, MSW, LCSW, Senior Manager of inflammatory arthritis support and education programs at the Hospital for Special Surgery in New York City, shared in an interview. She regularly coaches patients to broach their feelings with their doctor.
“Your provider needs to know [how you feel] to properly treat you, and to discern if this is a normal type of sadness and grief and anger, or is it something that really should be treated?” she says. “They need to have a full picture of who you are, not just your joint counts, your sed rate, and range of motion.”
At your next rheumatologist visit, try one of the following conversation starters to spark a dialogue about your mental health:
- Can we talk about my mental health during this visit?
- I’m having trouble sleeping and I can’t focus — are these signs of anxiety?
- I’ve feeling a little down lately and have no interest in things — how do I know if I’m depressed?
- What diet or lifestyle modifications can I try to minimize depression/anxiety?
- Are there any medications/treatments that will help my depression/anxiety?
- Do you think I’d benefit from talking to a mental health professional?
The Importance of Treating Depression and Anxiety
Having untreated depression and anxiety isn’t just bad for your overall quality of life; it can also derail your arthritis treatment, which can in turn make your mental health issues worse — leading to a vicious cycle. Depression and anxiety are associated with increased disability and a worse response to treatment.
“Depression is one of the best markers of non-adherence to treatment,” explained Susan Bartlett, PhD, a Professor of Medicine at McGill University in Canada, in an article on psoriatic arthritis and mental health. “People who are depressed are far less likely to be taking their treatment as prescribed.” She attributes this to the sense of hopelessness and helplessness that are often part of depression.
There is no formula that can predict which arthritis patients will develop depression or anxiety, according to an article on SimpleTasks, a site from the American College of Rheumatology. Many factors — including biology, coping mechanisms, and a patient’s level of distress — affect whether or not someone with a rheumatic disease will also develop depression, according to Karen Smarr, PhD, Clinical Assistant Professor of Medicine at the University of Missouri, in the article.
Only a fraction of people with depression and anxiety get treatment, however. A big part of that may be due to patients’ reluctance to take medication or to add therapy to a schedule that’s already challenging to maintain along with arthritis symptoms like pain and fatigue.
All of that is very understandable, but what’s most critical is that you don’t try to make these decisions on your own. People with depression and anxiety may experience brain changes that make them less aware of just how much they’re debilitated by their symptoms, which makes outside perspective and advice all the more important. And remember that just because you start medication or therapy for a mental health condition doesn’t mean you’ll need to stay with it indefinitely.
Bottom line: If you think you are experiencing depression or anxiety along with arthritis or another rheumatologic disease, tell your rheumatologist or primary care doctor.
“They might not bring it up because they’re really focused on controlling your illness,” says Batterman. “But I think that everybody, patients and providers alike, need to broaden their field of vision and see that [treating mental health] is part of treating inflammatory arthritis.”
Get Mental Health Support
We understand the mental health struggles that can occur when you are living with chronic illness. It is important to talk to someone who can help. You should contact your primary care physician or your insurance provider to learn about the supportive resources that are available to you. Here are other mental health resources for your reference:
- To find local support groups and services, you can call 1-800-950-NAMI (6264) or email info@nami.org. The National Alliance on Mental Illness HelpLine can be reached Monday through Friday, 10 AM to 6 PM ET.
- For a counselor or therapist in your area, view the resources page at Mental Health America: Finding Therapy.
- Crisis Text Line (free 24/7 support via text): Text HOME to 741741
- The Friendship Line from the Institute on Aging (toll-free 24/7 support for people ages 60 or over and adults living with disabilities): 1-800-971-0016
- LGBT National Hotline (free, confidential support for the lesbian, gay, bisexual, transgender, queer, and questioning community): 1-888-843-4564
- If your mental health concern is an emergency for you or someone else, you should call 911.
- If you are having suicidal thoughts or have or are thinking of hurting yourself, you should call the National Suicide Prevention Lifeline’s 24-hour toll-free crisis hotline, 1-800-273-TALK (8255).
Learn More About ArthritisPower
This question was one of our monthly ArthritisPower Community Questions, which offers ArthritisPower participants an opportunity to learn from each other and provide our research team insights.
If you’re diagnosed with RA or a musculoskeletal condition, you can participate in future polls like this, as well as research studies, by joining CreakyJoints’ patient research registry, ArthritisPower. As a patient-led, patient-centered initiative, our research team is committed to investigating research topics that matter most to you.
Beresford, L. Experts discuss rheumatologists’ role in treating depression, anxiety and psychological comorbidities in their patients. The Rheumatologist. American College of Rheumatology. December 2017. https://www.the-rheumatologist.org/article/experts-discuss-rheumatologists-role-treating-depression-anxiety-psychological-comorbidities-patients/.
Going Beyond the Physical: The Mental & Emotional Toll of Rheumatic Diseases. SimpleTasks.org. American College of Rheumatology. https://simpletasks.org/mental-and-emotional-toll-of-rheumatic-diseases/.
Heiman E, et al. Rheumatologists’ approaches to diagnosis and treatment of depression: JCR: Journal of Clinical Rheumatology. 2016. doi: https://doi.org/10.1097/RHU.0000000000000383





