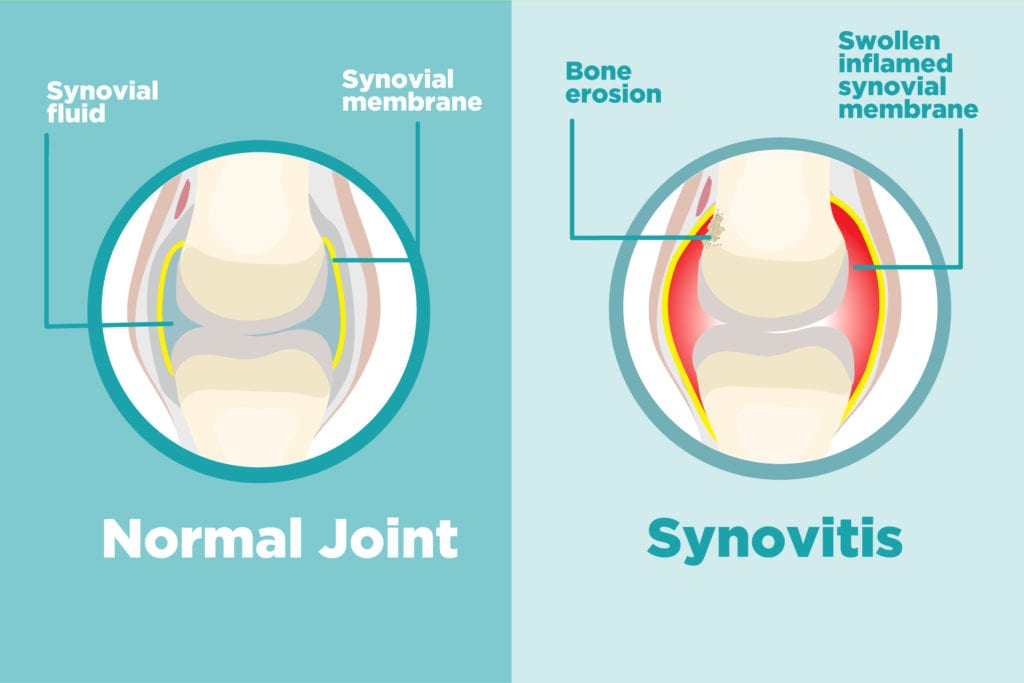
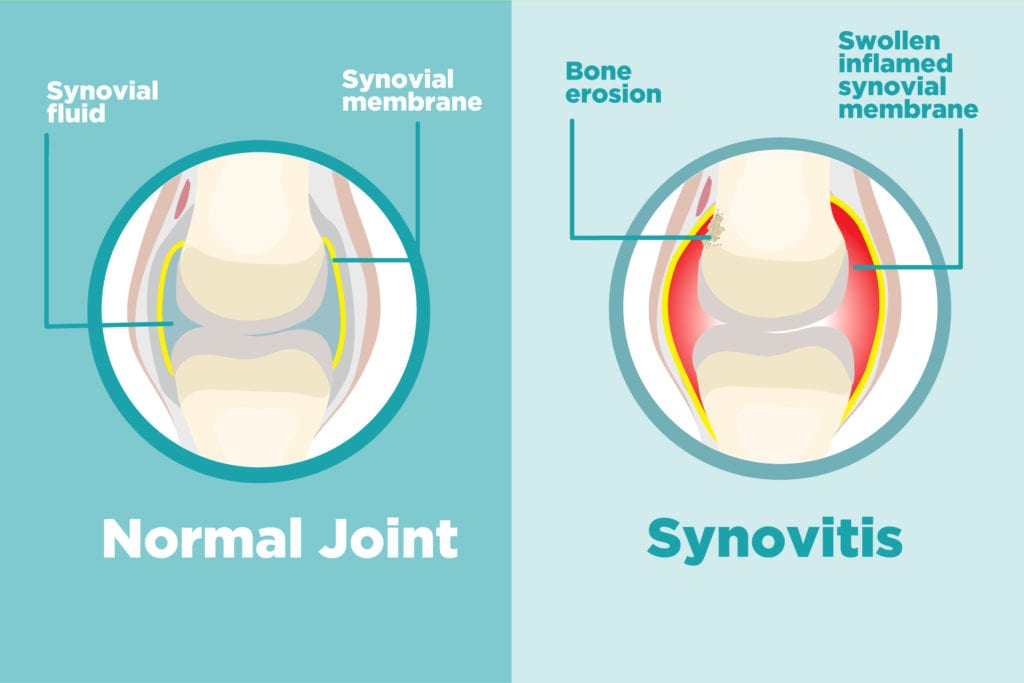
Synovitis is medical-speak for inflammation in the synovium, the membrane that lines your joints. In healthy joints, this protective tissue is only a few cells thick. Its job is to produce fluid that lubricates and nourishes the joint.
When the membrane is irritated or inflamed, it becomes thicker and swollen with excess synovial fluid. The inflamed synovium can eventually invade and destroy the cartilage and bone within the joint.
What Does Synovitis Feel Like?
The main symptom of synovitis is joint pain, accompanied by warmth, swelling, and stiffness that’s worse in the morning. You may feel synovitis symptoms in different joints at different times.
Sometimes, however, your joint will hurt worse than it looks, according to the Hospital for Special Surgery — in other words, there may be no obvious swelling or sign of injury that’s causing joint pain when you have synovitis.
Who Gets Synovitis?
Synovitis is present with inflammatory arthritis, says Vinicius Domingues, MD, assistant professor of medicine at Florida State University and CreakyJoints medical advisor. It’s common with rheumatoid arthritis (RA), but also occurs with psoriatic arthritis, lupus, and gout. Synovitis does not typically with osteoarthritis, however, says Dr. Domingues. This wear-and-tear form of arthritis causes little, if any, synovial inflammation.
In RA, your immune system mistakenly attacks healthy synovium. “When you have RA, one way to determine if the disease is active or inactive is with the presence of synovitis,” explains Dr. Domingues. “Synovitis equals active inflammatory arthritis.”
The same is true with gout. Though this form of arthritis is chronic, symptoms — such as joint pain, inflammation, and redness — come and go. During an attack of gout, you may have gout synovitis, says Dr. Domingues, but it won’t last forever. Once the attack is treated, synovitis will ebb again.
Inflammatory arthritis isn’t the only cause of synovitis, though. An injury or trauma to a joint can cause temporary reactive inflammation in the lining.
How Is Synovitis Diagnosed?
Your doctors take your history and examine the joint for warmth, tenderness to the touch, swelling, or thickening of the joint that feels “spongy.” For synovitis in a deeper joint, such as the hip, you might need an MRI or other imaging test to confirm a diagnosis of synovitis.
If there’s a history of joint trauma, the inflammation will be local to the injured joint. With inflammatory arthritis, synovitis may be seen in one or multiple joints. The way your doctor can differentiate is with medical history, says Dr. Domingues.
How Is Synovitis Treated?
Treatment depends on the cause: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen, can help reduce pain and swelling of synovitis from inflammatory arthritis or an injured joint. Taking disease-modifying drugs or biologics to manage inflammatory arthritis will help relieve inflammation and synovitis. For gout, your doctor will recommend medication to reduce uric acid levels. In some cases, your doctor may suggest steroid injections into the joint.
If those treatments don’t relieve symptoms and synovitis is persistent, you may need a synovectomy — a procedure in which much of the synovium is removed.





