Autoimmune disorders are among the trickiest types of conditions to diagnose, and psoriatic arthritis is no exception. There are no specific diagnostic tests for psoriatic arthritis, but there are tests that can rule out other diseases, such as rheumatoid arthritis, which can present with similar symptoms–inflammation of the joints, skin, and nails.
“Psoriatic arthritis is often grouped with rheumatoid arthritis,” says Alexis Ogdie, MD, MSCE, a rheumatologist in Philadelphia and Director of the Penn Psoriatic Arthritis Clinic. “While they do share some symptoms and disease features and in the very early phase are treated similarly, they are associated with different outcome and different treatments overall.” (Learn more about the difference between rheumatoid arthritis and psoriatic arthritis here.)
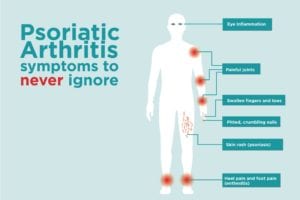
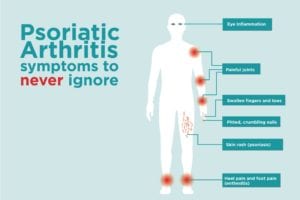
Signs of Psoriatic Arthritis
Here, she shares the signs the doctors should be looking for when considering a diagnosis of psoriatic arthritis.
Skin Rash (Psoriasis)
Most people experience this symptom for an average of seven to 12 years before the onset of psoriatic arthritis. According to the National Psoriasis Foundation, skin disease precedes joint disease in 85 percent of patients with psoriatic arthritis. Overactivity of the immune system speeds up the life cycle of skin cells, causing a buildup of rough, dead skin. The result: Red patches of skin with silvery scales called plaques. While plaques are often quite noticeable and may cover large areas of the body, that’s not always the case.
“Psoriasis can appear in multiple areas,” Dr. Ogdie says. “The scalp is one of the most common locations. Sometimes people don’t pay much attention to it and may think they have dandruff or eczema.”
Plaques can appear anywhere on the body, but other common spots include the elbows, knees, and around the ears. It’s estimated that up to 30 percent of people with psoriasis will develop psoriatic arthritis.
Pitted, Crumbling Nails
Psoriasis can also affect the fingernails and toenails, causing them to separate from the nail bed, develop pits, and appear thick and flaky. It’s generally considered that people with psoriasis who experience these nail changes are more likely to develop PsA than those with no nail involvement, according to Dr. Ogdie.
Swollen Fingers and Toes
This condition, called dactylitis, is another symptom of psoriatic arthritis that tends to appear in the early stages of the disease. Toes and fingers swell to the point that they appear sausage-like, and are red, tender, and painful to bend, Dr. Ogdie says. The presence of dactylitis is one of the symptoms that sets psoriatic arthritis apart from rheumatoid arthritis.
Painful Joints
Like people with rheumatoid arthritis, those with psoriatic arthritis experience achy, swollen, and stiff joints, though usually just on one side of the body. (With rheumatoid arthritis, the pain is more likely to be symmetrical.) The pain from psoriatic arthritis is worse in the morning or after resting. Any joint may be affected by PsA, but it’s most common in the large joints in the lower extremities, like the knees and ankles.
People with psoriatic arthritis can also experience back, hip, and shoulder pain — symptoms it shares with other conditions called spondyloarthropathies, which include ankylosing spondylitis and reactive arthritis. Rheumatoid arthritis, unlike PsA, isn’t categorized as a spondyloarthropathy, so pain in these areas helps distinguish between the two diseases. Read more about ankylosing spondylitis symptoms here.
Heel Pain and Foot Pain (Enthesitis)
In addition to attacking the joints, psoriatic arthritis also causes pain and tenderness where ligaments and tendons attach to the bones, which are called entheses. The two most commonly affected spots are the Achilles tendon and the plantar fascia, which causes pain at the back of the heel and the sole of the foot.
Eye Inflammation
People with psoriatic arthritis are at higher risk of developing an inflammatory eye condition called uveitis, which causes eye pain, redness, and blurry vision. However, this is more common among children with psoriatic arthritis, Dr. Ogdie says.
Inflammatory Bowel Disease
The impact of psoriatic arthritis goes beyond external manifestations. People with psoriatic arthritis are at higher risk of developing inflammatory bowel disease (IBD) – up to four times as likely, according to a 2021 Frontiers in Medicine review article. Forty percent of IBD patients have some form of joint disease, the review found.
Ruling Out Other Types of Arthritis to Diagnose PsA
Even though there aren’t any blood tests that help identify psoriatic arthritis, your doctor will test for some markers of inflammation — such as rheumatoid factor — to rule out RA and other types of arthritis. Imaging tests such as X-rays and ultrasounds are also used to detect changes associated with PsA. Some changes your doctor will be looking for include
- New bone formation
- Inflammation in the capsule of the joint
- Inflammation in the attachment points of the tendons and ligaments
If you have previously undiagnosed psoriasis, your doctor may also take a skin biopsy of a skin plaque to make the diagnosis. The presence of dactylitis and fingernail and toenail changes also factor heavily into establishing a diagnosis of psoriatic arthritis.
If you’re experiencing symptoms of PsA, it’s very important to see your doctor as soon as possible.
“The less time between the onset of symptoms and a diagnosis, the better,” Dr. Ogdie says. “A lot of joint damage can occur if the diagnosis is delayed.”
While there’s no cure for psoriatic arthritis, there are several treatment options available, and most people will gain some benefit from them, she adds. Treatment guidelines, as recently published in Rheumatology include:
- Nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen
- Disease-modifying antirheumatic drugs (DMARDs), which can slow or prevent tissue and joint damage and the progression of PsA.
- Biologic therapies, including TNF and IL-17 inhibitors, which target molecules involved in inflammation and are usually given by infusion or injection
- Certain psoriasis therapies, such as phototherapy
- Phosphodiesterase inhibitors, which promote blood vessel dilation and muscle relaxation
- Targeted oral agents such as JAK/STAT inhibitors, which calm an overactive immune system
- Topical treatments such as retinoid and steroid creams, prescription vitamin D creams, and over-the-counter or prescription salicylic acid creams, gels, and shampoos.
- Physical and occupational therapies
Powerful Podcasts to Help You Live Better with Psoriasis
The Global Health Living Foundation/CreakyJoints is embracing audio storytelling as part of our mission to reach the chronic disease patient community where they are. Click here to listen to one of our many podcasts, including Getting Clear on Psoriasis, The Psoriatic Arthritis Club, Breaking Down Biosimilars, The Health Advocates, Talking Head Pain, MatterofVax, Gut Culture, and more.
If you enjoyed reading this article, you’ll love what our video has to offer.
Interview with Alexis Ogdie, MD, MSCE, a rheumatologist in Philadelphia and Director of the Penn Psoriatic Arthritis Clinic.
Ogdie A., et al. Treatment Guidelines in Psoriatic Arthritis. Rheumatology. March 11, 2020. doi: https://academic.oup.com/rheumatology/article/59/Supplement_1/i37/5802853.
Yu Ting Chia, A., et al. Managing Psoriatic Arthritis with Inflammatory Bowel Disease and/or Uveitis. Frontiers in Medicine. September 16, 2021. doi: https://www.frontiersin.org/articles/10.3389/fmed.2021.737256/full.





