There’s a lot about psoriatic arthritis (PsA) that is invisible, such as joint pain and stiffness and debilitating fatigue. But psoriatic arthritis, which occurs because your immune system is overactive, causing inflammation, also has some visible clues that can help doctors diagnose the condition in the first place and keep tabs on how well the disease is under control.
Psoriatic arthritis can cause changes in your nails (such as crumbling and pitting) and can make your fingers and toes swell and look like mini sausages (known as dactylitis).
But the most well-known visual clue is a psoriasis rash.
You would think that having a psoriasis rash along with joint pain would be a telltale sign of psoriatic arthritis, but in real life, things are not so straightforward.
For some people, psoriasis skin manifestations might come years prior to a psoriatic arthritis diagnosis, so they may not necessarily be top of mind.
“About 85 to 95 percent of psoriatic arthritis patients develop the rash of psoriasis before they develop psoriatic arthritis, but some people develop joint pain before the rash, or they both come at the same time,” says Rebecca Haberman, MD, Clinical Instructor of Rheumatology at NYU Langone Health in New York City. “A smaller number of people — 3 to 5 percent of patients with PsA — do not have psoriasis but they do have a first degree relative who has the rash.”
What’s more, you may even have a psoriatic arthritis rash and not realize it.
“Patients think, ‘Oh, I’ve had this one little area behind my ear that sometimes itches,’ but otherwise they never notice it,” says Dr. Haberman. “Or they could have some little flecks in their scalp and believe that it’s dandruff. But if you have so-called ‘dandruff’ and joint pain, it may be that the dandruff is actually psoriasis.”
This isn’t to say that all rashes are psoriasis, notes Elaine Husni, MD, MPH, Vice Chair of the Department of Rheumatic and Immunologic Disease at the Cleveland Clinic in Ohio, “but if you have a rash that doesn’t go away after a week or two — and it gets more red or itchier — then it’s time to see a dermatologist,” who can help diagnose your skin condition and work with your rheumatologist to comanage your condition if you do have psoriatic arthritis, she says.
What Does a Psoriatic Arthritis Rash Look Like?
A psoriatic arthritis rash can present differently for different patients. For example, one person can have just a few patches near their scalp or elbow while other people can have them on the majority of their body.
One of the most common ways it shows up is as plaque psoriasis, says Dr. Haberman. Plaque psoriasis causes red, slightly raised patches with silvery scales covering them on the elbows, knees, scalp, or in or around the belly button and lower back.
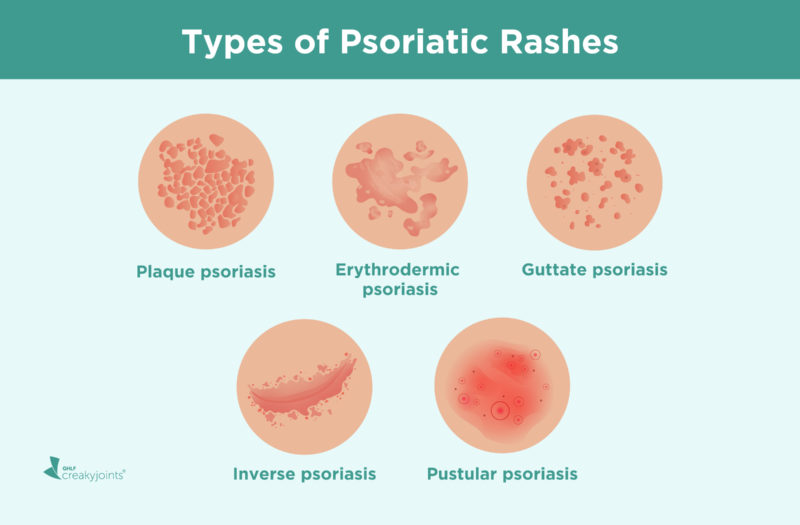
Other types of psoriatic rashes include:
- Erythrodermic psoriasis: generalized redness and scaling of a large portion of the body
- Guttate psoriasis: small, tear-dropped dots or lesions, usually on the trunk, upper arms, and thighs
- Inverse psoriasis: flat, red, shiny psoriasis patches in areas where the skin folds, such as elbows, knees, groin, armpit, or underneath the breast
- Pustular psoriasis: small, fluid-filled blisters, known as pustules, which often develop on the palm of the hands and feet
“The reason a psoriatic rash can be hard to diagnose is that it can present in such different ways,” says Dr. Haberman. Also, a psoriatic rash can mimic or be easily mistaken for other skin conditions, including:
- Acne
- Allergic reactions
- Cutaneous lupus
- Dermatophytosis (a fungal infection)
- Dry skin
- Eczema
- Jock itch
- Lichen planus
- Pityriasis rosea
- Pityriasis rubra pilaris
- Ring worm
- Seborrheic dermatitis (dandruff)
- Tinea versicolor
Psoriatic Rashes in Skin of Color
Psoriasis rashes can also present differently on different skin tones, which can lead to psoriatic rashes being misdiagnosed more often in people of color.
According to the American Academy of Dermatology:
- In white people, psoriasis tends to be red or pink, and the scale is often silvery white.
- In Hispanic and Latinx people, the psoriasis tends to be salmon-colored and the scale is often silvery white
- In Black people, the psoriasis often looks violet or dark brown, and the scale is often gray.
What Causes Psoriatic Rashes?
Unfortunately, we don’t yet know the exact cause of psoriatic arthritis or psoriatic rashes, although certain risk factors may play a role, including genetics and family history.
Roughly 40 percent of people with psoriatic arthritis have at least one close family member with psoriasis or psoriatic arthritis, says Dr. Haberman. Research is still ongoing, however, to determine whether a family history of psoriasis alone can increase your risk of psoriatic arthritis.
Other risk factors for psoriatic rash include:
- Alcohol consumption
- Bacterial or viral infections (including recurring strep throat or HIV)
- Obesity
- Skin trauma or injury (Koebner phenomenon)
- Smoking
- Stress
- Sunburn
- Taking certain drugs (including beta blockers, chloroquine, lithium, ACE inhibitors, indomethacin, terbinafine, and interferon-alfa)
What Is the Role of Rash in Psoriatic Flares?
For most people, a psoriatic rash can come and go, flaring for several weeks or months and then calming down. It can also go into remission, in which your skin may clear almost entirely.
Depending on the severity of your psoriatic rash, your dermatologist or rheumatologist will start with the mildest treatments — such as topical creams and ultraviolet light therapy — and then progress to stronger options if necessary. Read more about treatment options below.
Joint flares and skin flares in psoriatic arthritis are often separate, notes Dr. Husni. “For some people they do flare at the same times, so it’s really variable, which makes a psoriatic arthritis flare even harder to define,” she says.
You may have a lot of joint pain and no skin rash, or significant skin rash and one joint acting up, adds Dr. Haberman. “They don’t always flare at the same time at all.”
There is one exception, however. If your psoriatic arthritis joint pain and psoriatic rash is caused by skin trauma or injury (Koebner phenomenon) both your skin and joints would likely flare at the same time, she says.
Dr. Haberman also notes that you can get psoriatic arthritis whether your whole body is covered in psoriasis or you have just a fleck of psoriasis. In other words, the amount of psoriatic rash does not play a role in whether you develop joint pain.
Research shows that PsA patients with both joint and skin involvement have more disease burden and worse quality of life. One study published in the journal Rheumatology and Therapy found that 65 percent of patients with both joint and skin symptoms reported anxiety and depression compared with 56 percent of “joint-only” patients.
How to Treat Psoriatic Rashes
Treatment of psoriatic rash will depend on the severity of your rash, says Dr. Haberman. But, luckily, the options for the treatment of psoriasis are plenty and work very well, she says.
Topical Treatment
For mild cases of psoriatic rash, topical agents and medicated creams might include:
- Anthralin: inhibits DNA replication, slows hyperproduction of the skin cells that can lead to skin plaques
- Calcineurin inhibitors: reduce red, scaly plaques
- Coal tar: suppresses inflammation on the scalp
- Topical corticosteroids: ease the itchiness and pain, slow skin cell turnover by suppressing the immune system
- Emollients (Aquaphor, Eucerin, Vaseline): reduce dryness, itching, scaling
- Retinoids: slow skin growth, decrease scaling
- Vitamin D analogs: slow skin cell growth and help to rebalance your immune system
- Salicylic acid: encourages skin to self-exfoliate, reduces scaliness by getting rid of debris and excess proteins called keratins
Disease-Modifying Medications
For moderate to severe cases, the same systemic disease-modifying medications taken for psoriatic arthritis — to lower immune system overactivity and inflammation — also help reduce psoriatic arthritis rash. They fall into three general categories.
- Conventional disease-modifying antirheumatic drugs (DMARDs), which are often taken orally and include medication such as methotrexate, leflunomide, and sulfasalazine
- Targeted disease-modifying antirheumatic drugs (DMARDs), which are oral pills that are more targeted than conventional DMARDs [ex: a JAK inhibitor like tofacitinib (Xeljanz) or a PDE4 inhibitor like apremilast (Otezla)]
- Biologic disease-modifying antirheumatic drugs (DMARDs), which are administered as injections or infusions and are more targeted than conventional DMARDs [ex: a TNF inhibitor like adalimumab (Humira) or etanercept (Enbrel), an IL-17 inhibitor like ixekizumab (Taltz), an IL-23 inhibitor like guselkumab (Tremfya) or a T-cell inhibitor like abatacept (Orencia)]
UV Light Therapy
Another option for psoriatic rashes is light therapy (called phototherapy), says Dr. Haberman. This is not like going to a tanning salon, she explains. A dermatologist uses a special machine that emits UV light with shorter (and safer) wavelengths than you’d get from the sun or a tanning bed. “You go in for a couple of minutes, for a couple of sessions per week,” she says.
Home Remedies
Many people with psoriatic rashes may also turn to home remedies as part of an overall treatment plan, yet Dr. Haberman urges her patients to discuss with her what they’re planning to try first so they can decide together whether it will be helpful or harmful.
For example, here are some home remedies that dermatologists approve.
Lifestyle Changes
The following healthy lifestyle changes might also help reduce psoriatic skin flares and help your medical psoriatic rash treatments work more effectively:
- Get regular exercise
- Identify your triggers
- Maintain a healthy weight
- Manage stress
- Quit smoking
- Reduce alcohol consumption
- Stay educated about your condition
Track Your Psoriatic Arthritis Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Learn more and sign up here.
Can You Get Psoriasis If You Have Skin of Color? American Academy of Dermatology Association. https://www.aad.org/public/diseases/psoriasis/treatment/could-have/skin-color.
Huzar T. Which skin conditions can mimic psoriasis? Medical News Today. January 18, 2019. https://www.medicalnewstoday.com/articles/324220#pityriasis-rubra-pilaris.
Interview with Elaine Husni, MD, MPH, Vice Chair of the Department of Rheumatic and Immunologic Disease at the Cleveland Clinic in Ohio
Interview with Rebecca Haberman, MD, Clinical Instructor of Rheumatology at NYU Langone Health in New York City
Kvist-Hansen A, et al. Systemic Treatment of Psoriasis with JAK Inhibitors: A Review. Dermatology and Therapy. February 2020. doi: https://doi.org/10.1007/s13555-019-00347-w.
Psoriasis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/psoriasis/diagnosis-treatment/drc-20355845.
Tillett W, et al. Disease characteristics and the burden of joint and skin involvement amongst people with psoriatic arthritis: a population survey. Rheumatology and Therapy. May 2020. https://doi.org/10.1007/s40744-020-00221-8.
Wang C, et al. Efficacy of topical calcineurin inhibitors in psoriasis. Journal of Cutaneous Medicine and Surgery. January-February 2014. doi: https://doi.org/10.2310/7750.2013.13059.