A complex autoimmune disease affecting 1.5 million Americans, lupus is often referred to as a “great imitator” because its symptoms can resemble those of many other conditions, such as rheumatoid arthritis or fibromyalgia. One of those conditions is myositis, a much rarer condition characterized by muscle weakness, fatigue, and, in some forms, rash. As a result, myositis can be easily mistaken for lupus, especially at first.
“Many people at least know a little about what lupus is, but few people know what myositis is until you have it,” says Lisa Christopher-Stine, MD, a rheumatologist and director of the Johns Hopkins Myositis Center in Baltimore, Maryland. She explains that while the diseases are different, they can be considered cousins, with many aspects in common. “They do have similarities with regard to fatigue, they more often affect women, they’re a little nebulous — and there often is a delay in diagnosis.”
Read on to learn about the connections between lupus and myositis, plus more about their symptoms, diagnosis, and treatment.
The Basics of Lupus
Lupus is a chronic autoimmune disorder, which is a kind of illness in which your body’s immune system attacks healthy cells. About 90 percent of lupus patients are women. Compared to Caucasians, women of African American, Hispanic, Native American and Asian descent have a higher risk of developing lupus. Lupus often first strikes between the ages of 15 and 45, though one in five lupus patients are diagnosed as children. While it’s unclear exactly what causes lupus, genetics and environment likely play big roles.
There are multiple types of lupus. The most common is systemic lupus erythematosus (SLE), which affects about seven in 10 patients. In fact, says Dr. Christopher-Stine, “when people say lupus, most of the time they’re generalizing to SLE.” The condition causes chronic inflammation and can damage a range of body parts, including such organs as the heart and kidneys. Symptoms of SLE can be mild and tolerable or severe and potentially fatal. Though people do die of SLE, the survival rate has improved significantly over the years, and many with lupus live healthy lives.
Approximately one in 10 lupus patients have some form of cutaneous — or skin — lupus, which can cause rashes or sores. Drug-induced lupus is another type; symptoms typically disappear for good after you stop taking the responsible medication. Neonatal lupus, which affects infants, is similar in that it often goes away — usually in the first six months of life — and doesn’t cause long-term problems.
Common Symptoms of Lupus
Lupus can trigger a wide variety of symptoms. They may affect any part of the body, can appear at any point in time, and often come and go. Many patients experience cycles of flares and remission, during which symptoms get worse and then better again. The most common symptoms include:
Pain
The vast majority of lupus patients experience pain, swelling, or stiffness in joints or muscles. It’s often an early sign of the disease.
Fatigue
Extreme or prolonged tiredness is almost universal among people with lupus, and can occasionally be the only noticeable symptom.
Rash
A red rash, often in a butterfly pattern spread across the face, is considered a telltale sign of lupus. Some patients may develop scaly patches called discoid lesions.
Other symptoms of lupus include:
- Photosensitivity
- Weight fluctuation
- Low-grade fever
- Headache
- Hair loss
- Mouth sores
- Blood clots
- Anemia
Lupus can also affect organs throughout the body, including the heart, brain, and lungs. About half of patients develop inflammation of the kidneys called lupus nephritis. People with nephritis have problems removing waste from the blood, which can cause blood to appear in the urine, as well as swelling in the arms, hands, legs, and feet. Without treatment, lupus nephritis can lead to kidney damage and even end-stage renal disease.
The Basics of Myositis
Also known as inflammatory myopathy, myositis is an umbrella term for a number of different conditions that cause muscle inflammation and weakness. “Generally speaking, the word ‘myo’ means muscle and ‘itis’ means inflammation,” says Dr. Christopher-Stine. Myositis can be triggered by several different things, she explains, including an autoimmune reaction where your body starts attacking your muscles.
Myositis typically affects more women than men, often between the ages of 30 and 60, though children and older men may also develop forms of the disease. On the whole, it is not well understood, largely because it is so rare, particularly compared to lupus. “In the U.S., lupus affects about one in 1,000 people, with black women being affected more — about one in 250,” explains Dr. Christopher-Stine. “And myositis affects about one in 100,000.” All told, it’s thought that between 50,000 and 75,000 Americans have myositis.
There are different types of myositis, including polymyositis, dermatomyositis, necrotizing autoimmune myopathy, and inclusion body myositis — the only form that is more common in men than in women. Though they can be very symptomatic for a long time, most cases of myositis are treatable and usually not life-threatening in the absence of severe lung or heart disease.
Common Symptoms of Myositis
Though symptoms differ by person and disease type, the main feature of myositis is usually muscle weakness, which often starts slow and worsens over time. Often, you develop problems with particular movements. “You can have difficulty rising from a low-seated chair or getting out of a bathtub,” says Dr. Christopher-Stine, “or, in the upper extremities, you can struggle with reaching into a cabinet or reaching over your head, such as while drying your hair for a prolonged amount of time.”
Due to the weakness, myositis patients may be prone to tripping and falling. People with polymyositis or dermatomyositis can also develop serious heart issues, and even have problems breathing. Other common symptoms of myositis include:
Rash
Dermatomyositis causes a signature rash, which can help doctors tell it apart from polymyositis. Patchy and purple-red in color, the rash is often found on the eyelids, face, neck, shoulders, upper chest and/or back, though it can appear elsewhere, as well. Sometimes, dermatomyositis patients have a rash without muscle weakness.
Fatigue
Generalized, severe fatigue can occur, and patients may feel excessively tired after standing or walking.
Pain and swelling
Some people with myositis can have muscle or joint pain, and may even develop arthritis.
Some myositis patients may experience fevers, photosensitivity, or weight loss as well. People with dermatomyositis — especially kids — can develop calcinosis, or hard nodules under the skin.
Even though people with myositis have symptoms, many people with these symptoms often wait to see a doctor.
“Particularly in the case of inclusion body myositis, they make excuses for their symptoms, thinking that it’s a natural part of getting older,” says Dr. Christopher-Stine. This is dangerous, she explains, because it delays a myositis diagnosis.
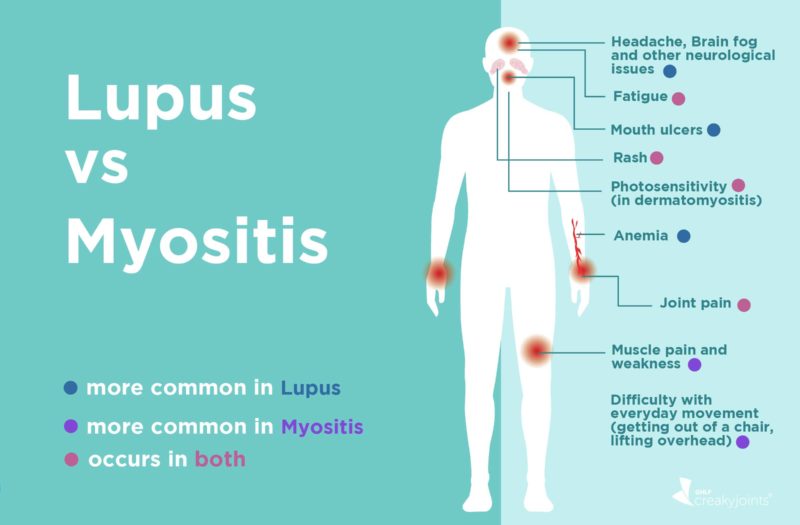
Subtle Differences in Symptoms of Lupus vs. Myositis
Due to their similar symptoms and the comparative rarity of myositis, myositis is often mistaken for lupus. “Many patients are actually told they have lupus first,” says Dr. Christopher-Stine. But there are some key differences, even in symptoms that may seem the same:
Rash
“With regard to the skin, it is not uncommon for patients to be diagnosed with lupus and actually have dermatomyositis, because the butterfly rash on the cheek is very similar,” says Dr. Christopher-Stine. One difference, she explains, is where the rash occurs. Lupus doesn’t generally appear in the area below the nose and above the lips, while dermatomyositis does.
Weakness and fatigue
People with lupus may feel tired and weak, but their muscles remain strong and useable, explains Dr. Christopher-Stine. Whereas in myositis, “it’s more than fatigue — it’s actual physical muscle weakness.”
It’s important to remember that many autoimmune diseases can have similar symptoms, at least at first. Some people with these symptoms may not have lupus or myositis, but another condition entirely. Or, they could have both diseases, since they very occasionally occur with one another. Either way, an accurate diagnosis is vital for treatment.
Diagnosing Lupus vs. Myositis
Neither lupus or myositis can be diagnosed with a single test; to identify either disease, providers have to consider many different factors and eliminate the possibility of other conditions. That often means that a diagnosis can take months — or in some cases, years. “There can be a substantial delay in diagnosis with both of these diseases, because they affects so many organ systems,” says Dr. Christopher-Stine.
Whether your doctor suspects lupus or myositis, to kick off the process, they will first ask for a rundown of your symptoms, your medical history, and your family’s medical history.
“Myositis is generally not associated in families, whereas lupus is,” says Dr. Christopher-Stine. You’ll also receive a thorough physical exam.
If your doctor believes you have lupus, they’ll proceed to blood tests. These can include a complete blood count (CBC) — to check if your white blood cell, red blood cell, or platelet count is low — and an antinuclear antibodies (ANA) test, which can show whether your immune system is attacking your body. Most people with lupus have a positive ANA test (though a positive ANA can also indicate diseases other than lupus). The diagnostic process may also involve a urine test to check for kidney issues, or a biopsy of your skin or kidney to look for inflammation.
If your doctor thinks you have myositis, they may test your blood for elevated levels of an enzyme called creatine kinase. Diagnostic tests, including electromyography, nerve conduction tests, ultrasound and magnetic resonance imaging (MRI) may help rule out other conditions. Finally, a muscle or skin biopsy is often used for confirming myositis and pinpointing the type of disease, whether it’s polymyositis, dermatomyositis, or something else.
Treatment for Lupus vs. Myositis
There is no cure for either lupus or myositis. Treatment for either disease is a little different for every patient, and should focus on controlling symptoms and improving quality of life.
For lupus patients: The goal of lupus treatment is to keep flares to a minimum, reduce the immune system reaction, and limit organ damage. Your plan should be a coordinated effort between your rheumatologist, primary care physician, and additional providers depending on the effects of your disease. Lifestyle changes, like eating a healthy diet or quitting smoking, may be involved.
Many lupus patients take medications to relieve symptoms. For example, non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help ease pain, while corticosteroids like prednisone are often used to quickly reduce inflammation and tame flares. Many lupus patients take medications that act on their immune system, such as the antimalarial drug hydroxychloroquine, or immunosuppressive medications such as cyclophosphamide, methotrexate, and azathioprine. The medication belimumab (Benlysta) was the first biologic approved specifically for patients with lupus back in 2011, and there is a lot of ongoing research into additional targeted therapies for lupus.
Lupus patients may also take additional medications for related health conditions, like high blood pressure or infections, linked to the disease.
For myositis patients: Myositis is often treated first with corticosteroids. “I think prednisone is the most quintessential anti-inflammatory and immune suppressant,” says Dr. Christopher-Stine. “And most rheumatic diseases respond to prednisone in the beginning.” Inclusion body myositis is the exception; steroids generally aren’t effective. Other treatments for myositis can include immunosuppressants (such as methotrexate, azathioprine, mycophenolate mofetil, cyclosporine, tacrolimus, cyclophosphamide, and hydroxychloroquine) and immunoglobulin, which is a blood product that contains antibodies that help the immune system.
Treatment also includes physical and occupational therapy, heat therapy, assistive devices, and exercise.
With accurate diagnosis and prompt treatment, your chances of living well with either lupus or myositis improve greatly. But you have to get to a health care provider first. “Vague symptoms can make patients doubt themselves, but you should be firm in making sure that a doctor has heard you,” Dr. Christopher-Stine says. “If you believe that something wrong, it probably is.”
Get Involved in Arthritis Research
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
Keep Reading
About Myositis. Johns Hopkins Myositis Center. https://www.hopkinsmyositis.org/myositis.
About Myositis. The Myositis Association. https://www.myositis.org/about-myositis.
African Americans and Lupus. Lupus Foundation of America. https://www.lupus.org/s3fs-public/Doc%20-%20PDF/Ohio/African%20Americans%20and%20Lupus.pdf.
Clinical manifestations and diagnosis of systemic lupus erythematosus in adults. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-systemic-lupus-erythematosus-in-adults.
Common symptoms of lupus. Lupus Foundation of America. https://www.lupus.org/resources/common-symptoms-of-lupus.
Dermatomyositis. Johns Hopkins Myositis Center. https://www.hopkinsmyositis.org/myositis/dermatomyositis.
Dermatomyositis Information Page. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/All-Disorders/Dermatomyositis-Information-Page.
Diagnosing and Treating Lupus. Centers for Disease Control and Prevention. https://www.cdc.gov/lupus/basics/diagnosing.htm.
Diagnosis. The Myositis Association. https://www.myositis.org/about-myositis/diagnosis.
Facts About Inflammatory Myopathies (Myositis). Muscular Dystrophy Association. https://www.mda.org/sites/default/files/publications/Facts_Inflamm_Myopathies_P-199.pdf.
Finding the right treatment approach for you. Lupus Foundation of America. https://www.lupus.org/resources/finding-the-treatment-approach-for-you.
How lupus affects the renal (kidney) system. Lupus Foundation of America. https://www.lupus.org/resources/how-lupus-affects-the-renal-kidney-system.
Inflammatory Myopathies Fact Sheet. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Inflammatory-Myopathies-Fact-Sheet.
Interview with Lisa Christopher-Stine, MD, a rheumatologist and director of the Johns Hopkins Myositis Center in Baltimore, Maryland
Lupus. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Lupus.
Lupus and Kidney Disease (Lupus Nephritis). National Kidney Foundation. https://www.kidney.org/atoz/content/lupus.
Lupus facts and statistics. Lupus Foundation of America. https://www.lupus.org/resources/lupus-facts-and-statistics.
Lupus nephritis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/lupus-nephritis/symptoms-causes/syc-20354335.
Manson JJ, et al. Systemic lupus erythematosus. Orphanet Journal of Rare Diseases. March 2006. doi: http://dx.doi.org/10.1186/1750-1172-1-6.
Overlapping Autoimmune Diseases. The Myositis Association. https://www.myositis.org/about-myositis/complications/overlapping-autoimmune-diseases.
Polymyositis. Johns Hopkins Myositis Center. https://www.hopkinsmyositis.org/myositis/polymyositis.
Polymyositis Information Page. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/All-Disorders/Polymyositis-Information-Page.
Systemic Lupus Erythematosus (Lupus). National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/lupus.
Treatment and Disease Management. The Myositis Association. https://www.myositis.org/about-myositis/treatment-disease-management.
Types of Myositis. The Myositis Association. https://www.myositis.org/about-myositis/types-of-myositis.
What is the appearance of malar rash in systemic lupus erythematosus (SLE)?. Medscape. https://www.medscape.com/answers/332244-19795/what-is-the-appearance-of-malar-rash-in-systemic-lupus-erythematosus-sle.
Worcester S. Malar rash flagged by crusty lips, nasolabial sparing. Rheumatology News. May 16, 2014. https://www.mdedge.com/rheumatology/article/82417/lupus-connective-tissue-diseases/malar-rash-flagged-crusty-lips.