Chronic Pain and Sleep
People with chronic pain are used to losing sleep. Between 50 and 90 percent of people with chronic pain report that they don’t sleep well, which can lead to daytime fatigue, depression, and negative effects on work and family life. There is strong data suggesting that poor sleep makes pain worse, and this becomes a vicious cycle as the pain then further disrupts sleep. Many people assume that people who are in pain don’t sleep well because the pain keeps them up at night, but the relationship between pain and sleep is actually much more complex.
The Relationship Between Pain and Sleep

It’s not always the case that people who are in pain simply cannot fall asleep. Pain can also interfere with the sleep cycle, even if you’re not aware of it. During a normal night’s sleep, we cycle from light sleep to deep sleep to REM (rapid eye movement) sleep up to five times. If you don’t get enough deep and REM sleep, you are likely to feel tired in the morning. While sudden severe pain can wake you from a deep sleep, even milder pain can negatively impact sleep quality. That’s because milder pain can cause “microarousals” – periods of time when you are shifted back into light sleep. Though you’re not likely to be aware of these microarousals when they happen or remember them the next day, you will probably wake feeling like you didn’t sleep much if at all.
How Does Arthritis Impact Sleep?
While there are numerous painful conditions that can disrupt sleep, including headaches, back pain, fibromyalgia, nerve pain and arthritis, people with arthritis are particularly vulnerable to poor sleep. About one-third of people who have pain while trying to sleep have arthritis pain, according to a National Sleep Foundation Gallup Poll. And because the pain of arthritis can vary from day to day, it is more likely to cause sleep problems than pain that remains constant. That’s because pain that varies is unpredictable and thus more difficult for the body to adjust to.
We know that even in people without arthritis or any chronic pain, disrupted sleep leads to increased pain sensitivity and increased markers of inflammation in the blood. Researchers believe lack of sleep can trigger inflammatory pathways that worsen arthritis pain. Poor sleep can also make you more sensitive to the perception of arthritis pain – in other words, disturbed sleep is not directly making you achy; rather it is affecting how you perceive the arthritis pain.
What does the research say about arthritis and sleep?
A 2012 study of sleep quality in people with chronic pain, including those with osteoarthritis, found that the amount of pain people were in before they went to bed had little effect on sleep quality. However, sleep quality predicted how much pain they were in the next day. This further supports the theory that the worse your sleep quality, the more sensitive you are to pain.
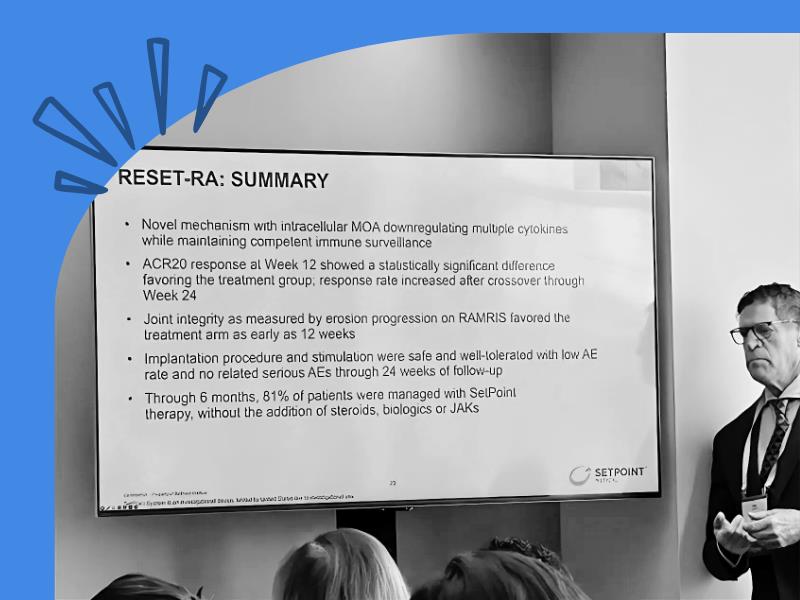
At least half of people with osteoarthritis (OA) have trouble falling asleep or staying asleep all night, and studies show people with hip and knee OA have more insomnia and daytime sleepiness than those without osteoarthritis. In people with rheumatoid arthritis (RA), sleep problems can increase levels of stress hormones and aggravate flares. Besides increased flares, RA patients with disrupted sleep are also more likely to have depression, severe pain and difficulty performing daily activities than RA patients without sleep issues. A 2011 University of Pittsburgh study showed that 61 percent of RA patients experienced these problems and were also poor sleepers. People with RA who wake during the night, even “microarousals,” may also be lacking in a type of growth hormone that is needed to repair tiny tears in the muscles that happen during the day. When muscles are not adequately repaired, increased joint and muscle pain can result.
Even when their inflammation is controlled, some people with RA have a low tolerance for pain. One study in 2013 examined why this is the case. The study showed that sleep problems increase RA patients’ sensitivity to pain, suggesting that that poor sleep may interfere with the way the central nervous system processes pain in RA patients. Another study published in the Journal of Clinical Sleep Medicine found that poor sleep not only worsened pain, it also increased functional disability in people with RA.
It’s important to note that some common RA medications can also disrupt sleep, such the steroid prednisone. The painkillers morphine, codeine and even some over-the-counter pain medications like ibuprofen can interfere with the sleep cycle. If you are unsure whether a medicine you are taking may interfere with sleep, talk to your doctor or pharmacist.
Lifestyle Changes to Improve Sleep
There are many different lifestyle changes you can make that may help improve your sleep, even if you live with chronic pain. These include:
- Don’t consume caffeine in the evening. In fact, some experts recommend stopping caffeine consumption after 3:00 pm.
- Put away your cell phone, tablet, laptop and anything else that has a lit screen at least an hour before bedtime.
- Don’t eat a heavy meal before bed, as digestion can disrupt sleep patterns.
- Don’t watch TV in the bedroom.
- Keep your bedroom cool, quiet and dark. If it is too bright in the morning, consider getting black-out drapes or shades for the windows.
- Try relaxation techniques such as meditation to reduce stress.
Keep in mind that it is possible to have sleep issues that are unrelated to your arthritis. For instance, some people with arthritis may have other health problems like a sleep disorder or sleep apnea, stress from work or other life events, or untreated anxiety and/or depression. If you find that, even with lifestyle changes, your sleep is still not sound, talk to your doctor.