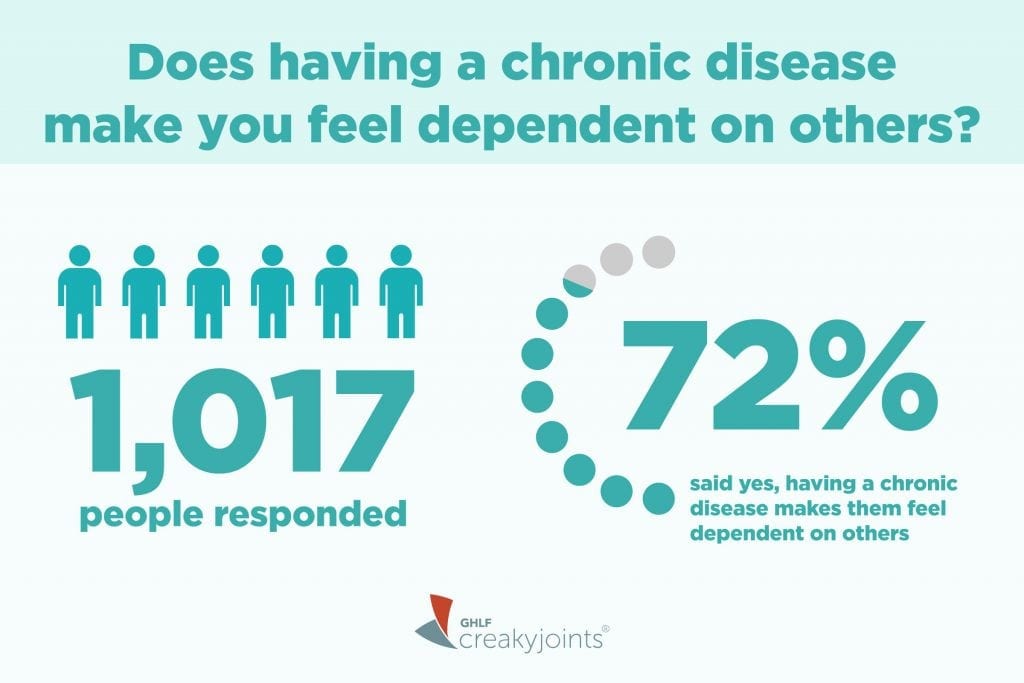
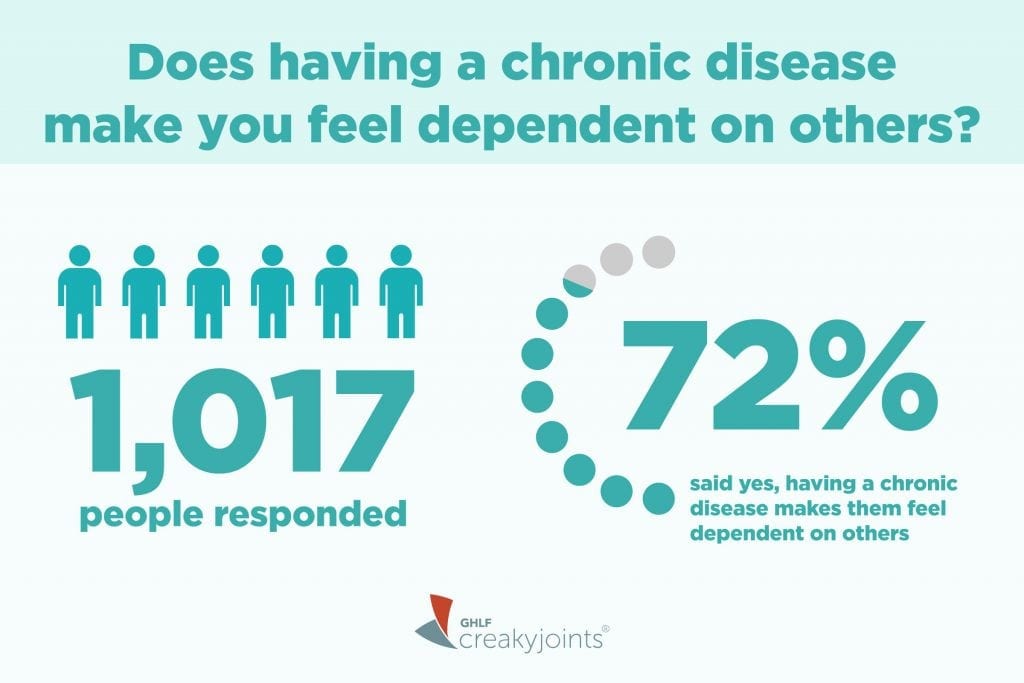
Does having a chronic disease make you feel dependent on others?
That’s the question we posed in our June 2018 monthly poll to participants in ArthritisPower®, our patient-centered research registry for joint, bone, and inflammatory skin conditions.
Of the 1,017 participants who responded, 72 percent said that yes, having a chronic disease makes them feel dependent on others. In other words, nearly three-fourths of individuals who took June’s poll report relying on others for some form of support.
It’s natural to have mixed feelings about needing support — your rational brain may know that you can no longer do everything by yourself, but at the same time, you feel may guilty about over-relying on others, or feel frustrated that you can’t get through your usual daily activities without extra help.
These are sentiments we hear over and over in the chronic illness community. For example:
“I’m having a really hard time accepting that letting go and allowing my family to help me isn’t a sign of weakness, it actually allows me more independence,” rheumatoid arthritis patient Bonnie H. told Healthline. “Because, when I have good days, I always completely overdo it, which means I’m going to be more dependent on them for a while.”
Guilt is the worst symptom of chronic illness for The Mighty blogger Jenna. “The hardest parts of my illnesses are not the symptoms or the drug side effects or even the illnesses themselves,” she writes. “The hardest parts are the internal battles between wanting help but thinking I shouldn’t need it, between knowing it’s out of my control and shaming myself for not controlling it.”
The Importance of Support for Chronic Illness
Receiving support is critical while you live with chronic illness.
“There are many types of support that may be useful,” according to an article by Joan Westreich, LCSW-R, a social work coordinator in the Early Arthritis Initiative at the Hospital for Special Surgery in New York City. “It could be physical support, such as help with housework or chores, but emotional support — expressed as caring, love, and empathy (that is, trying to put yourself in another person’s shoes) — is also meaningful.”
Positive support can help improve the way people with chronic illness cope emotionally and reduce the odds of depression or social isolation.
Support that simplifies activities of daily living can help manage pain and fatigue; assistance getting to and from the doctor and pharmacy can help with disease management, medication compliance, and more.
Assistance in the workplace, such as allowing for a more flexible schedule or having empathetic managers or colleagues, could affect your ability to stay employed and feel effective at work.
When Seeking Support Feels More Complicated
A common sentiment in a Healthtalk article about support among people with RA was that “people wanted others to understand their problems, to help when necessary, but not to fuss too much.”
For RA patient Alyssa B., feeling independent means knowing the difference between when to struggle to do things independently versus knowing when to seek help. “In the past, I would stubbornly do everything on my own, even if it put me in more pain,” she says in the Healthline article. “Now I know that asking my husband or family and friends for assistance is not weak but actually makes me stronger.”
A common mistake: Don’t assume your support community — even your partner, closest family members, or best friends — always knows what you need or want.
“Getting the support you want isn’t just about the people in your life doing right by you,” according to Westreich in the HSS article. “Often, your friends, family and colleagues won’t actually know what you need.” This can even lead to people shying away from reaching out because they’re worried about doing or saying the wrong thing.
Westreich suggests that you think about who could help make life easier for you, then reach out to those people and tell them what you need or how they can help. “Keeping in mind that even well-meaning loved ones and others may not be able to identify your needs,” she says, “actively collaborate with your support network of partners, family members, friends, coworkers, and religious communities to get what you need.”
When Outside Support Groups Can Play a Key Role
If you find that your current networks don’t meet your needs for emotional and concrete support,” Westreich notes, “it may be time to develop new avenues of support.”
One Healthtalk patient found an RA support group helpful because she could be herself there; she didn’t have to pretend she was stronger than she was.
“I believe in self-help and support groups because if you can actually positively talk to people where you don’t have to put on this big act that you’re always being strong,” she says, noting that support groups allow you to “actually be a real person and you can let your guards down but it’s very difficult.”
Learn more about finding arthritis support groups here.
If you’re someone who struggles with feeling dependent on others, consider these wise words from our recent Twitter #CreakyChats:
Remind myself this is temporary. Focus on what’s going right. Hold my husband’s hand. #CreakyChats https://t.co/XMg7yx6Blw
— Cathy Kramer (@cateepoo88) August 13, 2018
Related Resources
If you’re interested in reading more about this topic, here are some articles that might interest you:
- Learning to be Dependent After Chronic Illness
- How My Husband and I Make Our Marriage Work, Even With Chronic Illness
- The Guilt of Depending on Someone When You’re Ill
- Getting What You Want and Need While Living with Rheumatoid Arthritis
Learn More About ArthritisPower
This question was one of our monthly ArthritisPower community questions, which offers ArthritisPower participants an opportunity to learn from each other and provide our research team with valuable insights.
If you’re diagnosed with rheumatoid arthritis, osteoarthritis, or another musculoskeletal condition, you can participate in future polls like this, as well as other voluntary research studies, by joining CreakyJoints’ patient research registry, ArthritisPower.
As a patient-led, patient-centered initiative, our research team is committed to investigating research topics that matter most to you. Learn more about joining ArthritisPower here.





