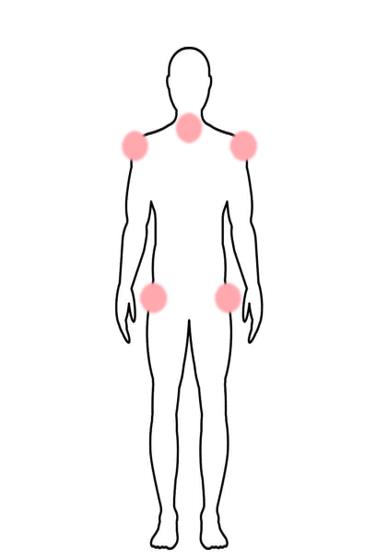
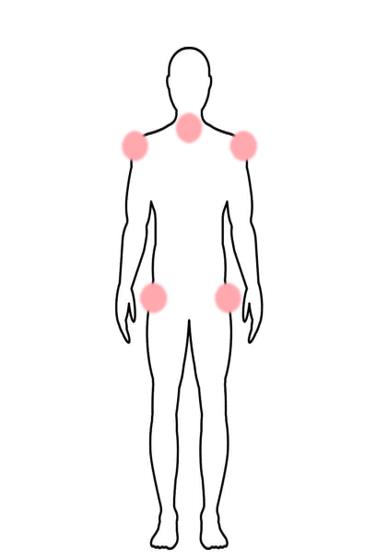
Polymyalgia rheumatica (PMR) is an inflammatory disorder that causes severe pain and stiffness that can come on suddenly, in a few days or even overnight. The pain mostly targets the shoulders, upper arms, neck, and the pelvic area. Polymyalgia rheumatica is the second most common type of inflammatory rheumatic disease, after rheumatoid arthritis, among people over 50.
In about half of cases, polymyalgia rheumatica (PMR) resolves itself in a period that can last from a few months to a few years. But in other cases it can become chronic. The good news: symptoms can be managed with the proper medication.
Who Gets Polymyalgia?
Women are most affected by PMR, making up two-thirds of people with the disease. According to the Mayo Clinic, most people who develop polymyalgia rheumatica are older than 65. There is a higher prevalence of PMR among people of Scandinavian descent, compared to those of other backgrounds. There are nearly 8,000 people in the United States affected by PMR.
While there is no known cause of the disease, studies of patients with PMR have shown the appearance of inflammation in the connective tissue around joints (synovium), particularly around the shoulders and hips.
What triggers the inflammation is uncertain, although a gradual dysfunction of the immune system that happens with aging (immunosenescence) is thought to be an important part of the disease and may explain why this condition almost exclusively affects people over age 50, says Dr. Michael George, MD, MSCE, Assistant Professor of Medicine at the Hospital of the University of Pennsylvania.
Additionally, some researchers think that certain types of white blood cells may trigger the inflammation of PMR, according to a 2023 review in Frontiers in Medicine. Like a domino effect, these cells can cause other immune cells to kick off a chronic inflammatory response. Dr. George adds that studies have shown high levels of the inflammatory protein called interleukin 6 (IL-6) in the blood of patients with PMR.
Signs and Symptoms of PMR
Polymyalgia rheumatica can have some symptoms in common with other inflammatory diseases, but there are some signs that are unique to the condition.
What are the symptoms of PMR?
The major symptom of PMR is pain and stiffness that is bilateral, or on both sides, and focused in the shoulders, neck, upper arms, and pelvic area that lasts for more than 45 minutes. It is usually worse in the morning or after long periods of inactivity. You may have limited range of motion, making it difficult to dress, brush your hair or raise your arms above the shoulders.
You may also experience more general symptoms such as:
- Flu-like symptoms
- Low grade fever
- Malaise
- Fatigue
- Unintended weight loss
- Loss of appetite
- Depression or mood changes
Listen to the podcast episode The Health Advocates, featuring PMR patient Linda Rinaldi, to get a real-life description of the symptoms of PMR.
What does the pain of polymyalgia rheumatica feel like?
The pain of PMR is often sudden or rapidly escalating over a period of a few days, says Dr. Anisha Dua, MD, MPH, Associate Professor and Director of the Vasculitis Center in the Division of Rheumatology at Northwestern University. Her patients often describe having pain when they do regular activities that require reaching overhead. Getting in and out of bed can be painful, too. The pain is usually worse in the morning with stiffness, especially in the shoulders or hip. It can sometimes improve as the day goes on.
How does PMR impact your well-being?
“Patients with PMR often feel very unwell,” says Dr. Dua. “Comments like ‘I feel like I got hit by a bus’ or feeling suddenly run down and unable to do regular activities are common.” But once you get the diagnosis and start treatment, you should feel significantly better within a few days.
Is polymyalgia rheumatica worse than rheumatoid arthritis?
Many of the symptoms of polymyalgia are nonspecific and can easily be confused with other diseases. For example, differentiating between PMR and early onset rheumatoid arthritis (RA) is a challenge for health care professionals and can hinder the start of effective treatment, according to a 2023 review on differentiating between the two diseases.
RA typically leads to stiffness and pain or swelling in the symmetric small joints like fingers, wrists, toes, and ankles, whereas the larger joints such as the shoulders and knees are less commonly affected. In contrast, PMR may affect these peripheral joints in ways that can resemble RA. PMR also prominently involves the hips and shoulder girdles, an attribute not present in RA.
A key distinction between the two is the pronounced joint swelling associated with RA. In contrast, a subset of PMR patients may experience minor swelling, predominantly in the knees, but this is typically mild and temporary. The erosive damage often seen in RA’s small joints doesn’t occur in PMR. The discomfort and stiffness felt in PMR, especially around the shoulders and hips, usually stem from inflammation in the surrounding tissues, not directly from the joints.
Distinguishing between RA and PMR becomes challenging when individuals over 60 begin to exhibit RA symptoms, especially since approximately 30 percent of RA patients first notice symptoms after this age.
Keeping up with your doctor appointments is crucial in correctly distinguishing PMR from RA — it can be challenging to obtain a clear diagnosis at times, leading to delays in the initiation of appropriate therapy. Another complicating factor is that patients with PMR can later be diagnosed with RA, indicating that the two diseases may share a single disease process, according to the review.
“Both PMR and rheumatoid arthritis can have a major effect on a person’s function and quality of life,” says Dr. George. “Unlike rheumatoid arthritis, however, PMR does not cause joint damage.” PMR also often responds very well to low doses of prednisone, while rheumatoid arthritis typically requires the use of other medications, he says.
Rheumatoid arthritis is usually more insidious in onset so the symptoms build over time whereas PMR is usually a more rapid with marked decline in functioning, adds Dr. Dua.
How are polymyalgia rheumatica and giant cell arteritis related?
People with PMR can sometimes have another condition called giant cell arteritis, which is an inflammation of the arteries on each side of the head, on the scalp, and in the aorta. If the blood vessels that supply the eye are affected, giant cell arteritis can lead to permanent vision loss if untreated, so it is very important to see your doctor if you are experiencing problems with your vision.
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, about one in 10 people with PMR have giant cell arteritis and about 50 percent of people with giant cell arteritis have PMR.
Similar to PMR, the symptoms of giant cell arteritis can start abruptly or can appear in a matter of weeks or months. And, like PMR, the condition can also bring on flu-like symptoms such as low grade fever, appetite loss, weakness, and weight loss.
The symptoms of giant cell arteritis also include:
- Headaches or scalp tenderness
- Jaw pain, especially when chewing
- Visual disturbances like double vision and loss of vision
- Inflammation of the aorta and its branches, which can cause cramping in the arms and legs
People with PMR should be aware of the risks of having giant cell arteritis, says Dr. George. “It can cause serious health problems, including vision loss if not identified and treated. New headaches, tiredness of the jaw when chewing, fevers, or any new vision symptoms should be evaluated by a physician as soon as possible.”
Have You Tried PainSpot?
What’s causing your joint, back, or neck pain? PainSpot will ask you a simple set of questions about your pain symptoms and help you figure out why you’re in pain. Use your PainSpot results to help you and your doctor get to the bottom of your pain. Learn more.
This article was made possible with support from Sanofi.
Interview with Dr. Anisha Dua, MD, MPH, Associate Professor and Director of the Vasculitis Center in the Division of Rheumatology at Northwestern University.
Interview with Dr. Michael George, MD, MSCE, Assistant Professor of Medicine at the Hospital of the University of Pennsylvania.
Ohta R, et al. Differentiating between Seronegative Elderly-Onset Rheumatoid Arthritis and Polymyalgia Rheumatica: A Qualitative Synthesis of Narrative Reviews. International Journal of Environmental Research and Public Health. January 2023. doi: https://doi.org/10.3390/ijerph20031789
Wu J, et al. Elderly-onset rheumatoid arthritis vs. polymyalgia rheumatica: Differences in pathogenesis. Frontiers in Medicine. January 12, 2023. doi: https://doi.org/10.3389/fmed.2022.1083879





