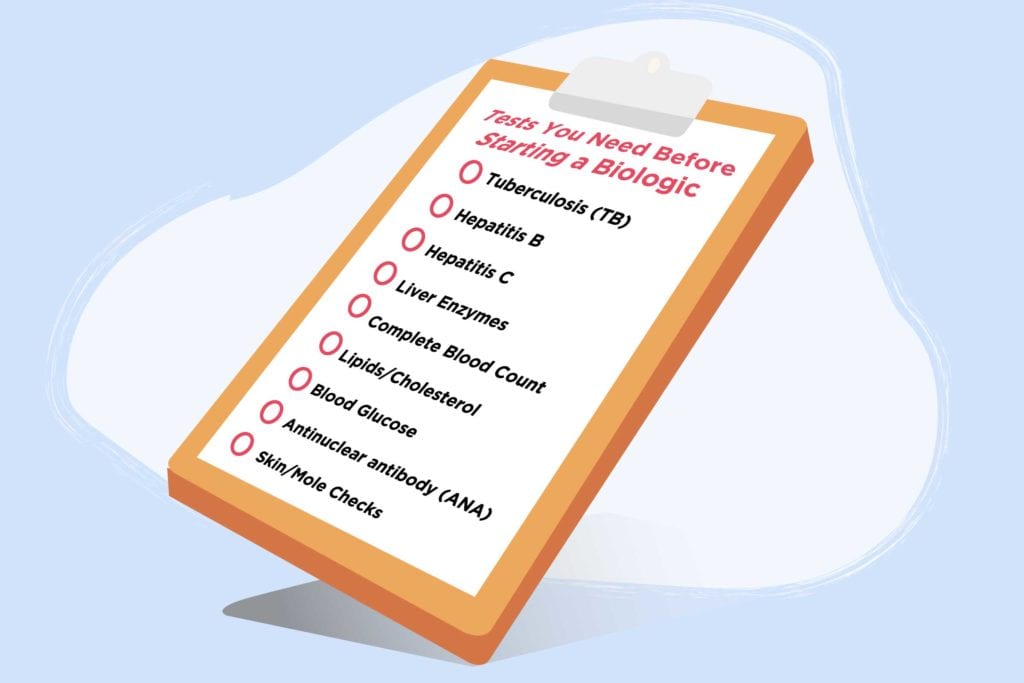
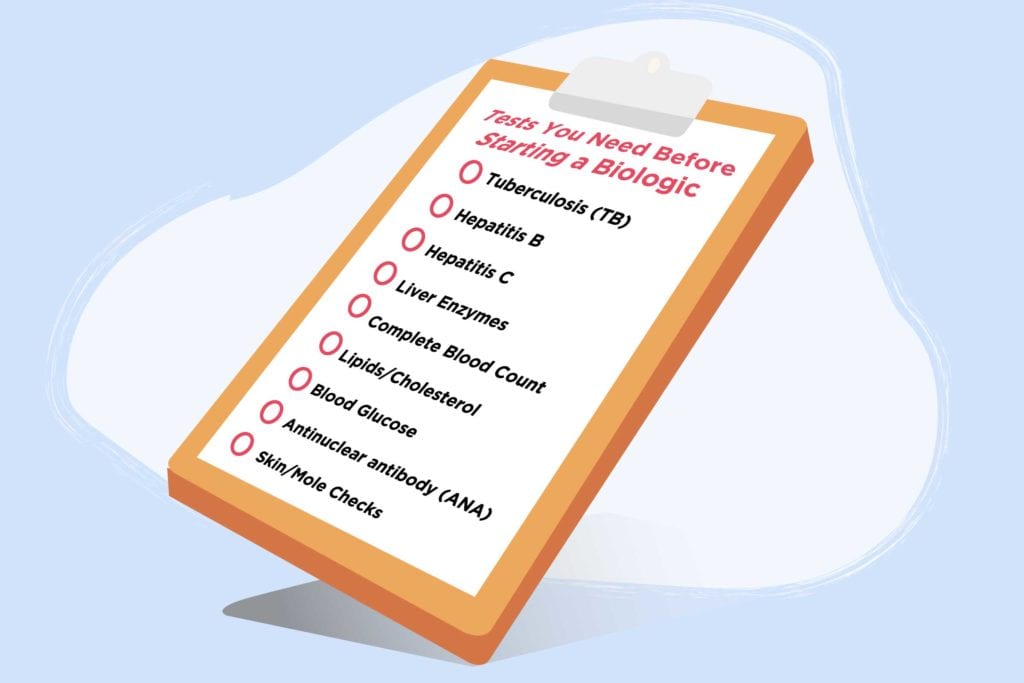
If and when the day comes when you and your rheumatologist decide you need to take a biologic drug to get your arthritis or a different inflammatory disease under control, you may be eager to get started now. But be prepared for at least a short delay. There are critical tests that need to be done before you can safely use one of these potent drugs to target inflammation-creating portions of your immune system.
Here’s a look at common tests your doctor will order before you start a biologic drug. If you’re not sure whether you’ve had any of these tests, ask your doctor about them.
Tests to Detect Silent Infections
Tuberculosis (TB)
You may have the TB bateria in your body but not know it because your immune system keeps it under control, a condition called latent TB. If you do, your doctor needs to know because treatment with a biologic can reactivate TB and lead to active disease.
To check for tuberculosis, you’ll usually get a blood test and perhaps a skin test. “We’ll often do a chest X-ray as some patients may have had past infections that show up on the X-ray. These are more likely to become active again during treatment. It doesn’t mean that the drug can’t be given but the doctor and patient may be more cautious,” says rheumatologist Scott Zashin, MD, of Dallas, Texas.
If a test reveals that you have latent TB, American College of Rheumatology guidelines call for putting off treatment with a biologic until you’ve been started on a TB drug for at least a month. If you have active TB, you may be referred to a specialist for treatment and a biologic won’t be started until the TB has cleared.
Hepatitis B (Hep B)
Doctors need to a do a blood test to check for the presence of the hepatitis B virus. This may
be positive because of previous exposure, an active disease that has resolved, or a currently active disease. “If someone screens positive for hepatitis B, I order a test to measure virus levels. If they are high, I refer patients to an infectious disease specialist for treatment. If not, I start on a biologic and monitor closely for changes in liver tests,” says Dr. Zashin. “There are drugs available to prevent reactivation of hepatitis B if you’ve been exposed in the past, but these are expensive and may or may not be recommended.”
Being positive for hepatitis B may also change the biologic drug your rheumatologist chooses to treat your arthritis. For example, in a 2017 study, the risk of hepatitis B reactivation was highest in patients taking rituximab. Using a steroid drug along with an immune suppressant also boosted the risk of reactivation.
Hepatitis C (Hep C)
Over the long term, hepatitis C can lead to liver damage and liver cancer. Many people who are infected with hepatitis C don’t know it. If a blood test reveals that you have hepatitis C, know that there are many treatments are available to eliminate the virus. These may be initiated either at the same time as or prior to starting a biologic.
“Sometimes people need additional testing or a liver biopsy and we need to coordinate their care with a liver specialist,” says Dr. Zashin.
If you have hepatitis C, your arthritis drug regimen may also need to change. In a study of veterans with hepatitis C and rheumatoid arthritis, the use of biologics was more likely to result in liver toxicity than the use of non-biologic disease-modifying drugs. When aggressive treatment is needed, the American College of Rheumatology suggests the TNF inhibitor etanercept as a possible biologic choice.
Tests that Create a Baseline for Future Monitoring
Liver enzymes
As you may be accustomed to if you’ve been on the disease-modifying drug methotrexate, your liver enzymes will be regularly monitored while you’re on a biologic. Testing before you start gives your doctor a baseline reading, and may also alter your treatment plan.
“Depending how high liver enzymes are, it may change our plan. If they are 1.5 to 3 times normal, we might give your biologic less often and keep a close eye on your liver enzymes. If they are higher than that, it might be a contraindication to using a biologic,” says Priyanka Iyer, MD, a rheumatology fellow at the University of Iowa.
Complete Blood Count
Biologics occasionally create blood abnormalities that require stopping the medication or lowering the dose, so you need a complete blood count both before starting and regularly during treatment.
Lipids/Cholesterol
Simply having rheumatoid arthritis by itself raises the risk of heart disease. In addition, some biologics can increase levels of your bad cholesterol or triglycerides, so your rheumatologist needs to know where you stand before starting treatment. If your cholesterol is high, you can usually be treated for that while starting your biologic drug, but if it’s extremely high doctors may want to treat your cholesterol first. Read more about reducing your heart disease risk when you have inflammatory arthritis.
Tests to Avoid Unnecessary Scares
Blood Glucose
If you have diabetes, you’re likely to keep close tabs on your blood sugar anyway, but a baseline reading can be helpful if you are started on the biologic abatacept. Its inactive ingredients include a form of sugar that can lead to a falsely high reading on certain test strips on the day of your infusion.
Antinuclear antibody (ANA)
This blood test is used to help diagnose lupus and other autoimmune disorders. Uncommonly, people who take TNF blockers develop drug-induced lupus, with a positive ANA test result and symptoms such as muscle and joint pain and flu-like symptoms. When that happens, they need to stop taking the drug.
“But it’s more common for people taking anti-TNF drugs to develop a positive ANA but not to have symptoms, which does not require stopping their biologic. I like to know beforehand if a patient already has ANA in their blood. If they do, I order more specific lupus blood tests, especially ones that can become abnormal while taking a TNF blocker. Depending on the results, I might reconsider the diagnosis of rheumatoid arthritis or wonder if the person has an overlapping condition,” says Dr. Zashin. Here’s why lupus and rheumatoid arthritis can be misdiagnosed for each other.
Test to Check for Long-Term Cancer Risks
Skin/Mole Checks
In addition to lab tests, it’s good to have a thorough skin check from a dermatologist prior to starting a biologic drug. Having RA raises the risk of non-melanoma skin cancers, and some biologics increase the risk further. “I would want any skin cancers to be treated before starting a biologic, and if a person has recurrent skin cancers it might influence my choice of a drug. I would stay away from a TNF blocker,” says Dr. Zashin.
Track Your Medications with ArthritisPower
Join CreakyJoints’ patient-centered research registry and log your medications to track side effects and impact on disease activity. Learn more and sign up here.





