When you have a form of inflammatory arthritis (like rheumatoid arthritis, psoriatic arthritis, or axial spondyloarthritis) getting a handle on your flares is likely a top priority. After all, an arthritis flare can seemingly come out of nowhere and throw off your life for days, weeks, or longer.
“When patients get a flare, there is a sudden jump in the level of pain and fatigue,” says Samar Gupta, MD, a rheumatologist at the University of Michigan. In addition, your joints may also feel swollen, red, and warm to the touch, says Dr. Gupta.
While some people with arthritis can rest and recuperate during an arthritis flare, others find themselves having to “push through” due to work and family obligations.
Especially if you’re experiencing more (or more severe) flares than normal, you shouldn’t stay silent. “It’s important for patients to report their symptoms accurately to their rheumatologists,” says Dee Dee Wu, MD, a rheumatologist at Hospital for Special Surgery in New York City. “From there, it’s up to the rheumatologist to determine what may be causing the flare and the best course of action.”
Some flares can resolve in a couple of days with the help of steroid medications, over-the-counter anti-inflammatory pain relievers, and home remedies like heating pads. Other flare episodes are more stubborn and may require a change in disease-modifying antirheumatic drug (DMARD) medication to address. Either way, people with arthritis learn their own tips and tricks to cope with flares and help prevent them from recurring.
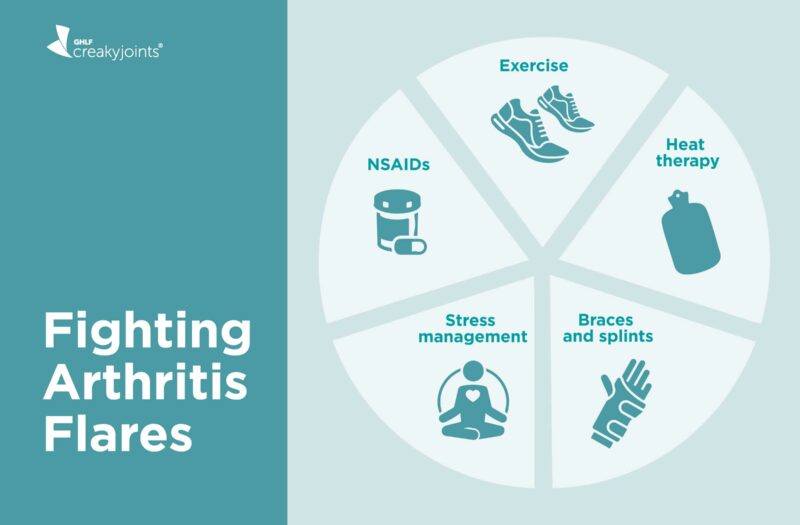
We asked rheumatologists and members of the CreakyJoints community for their go-to tips for coping with and preventing an arthritis flare.
Causes of Arthritis Flares
From humidity to stress to skipping medication, there are many possible causes of arthritis flares. While some culprits, like weather changes, are out of your control, others can be addressed to better manage and minimize these flares.
Medication
“One of the biggest culprits of flares is people not taking their medications as prescribed,” says Dr. Wu, adding that this has become more common during the pandemic. “Between accessing a pharmacy during lockdown and patients’ concerns about getting the COVID-19 vaccine while on immunosuppressant medication, people have scaled back on their immunosuppressive drugs or haven’t been taking them as prescribed.”
Additionally, if your medication is not controlling the disease as well as it should, then flares may occur more often.
“The goal of any arthritis treatment is to stop the inflammatory proteins so that not only is the patient symptom-free but they don’t get these disabling flares,” says Dr. Gupta. “If a patient is still having baseline pain or flares, then we need to reassess the treatment.”
Infection
Being sick — say, with a cold, flu, or COVID-19 — can bring on flares in people with inflammatory arthritis.
“When people are sick with viral or bacterial illness, that can trigger their immune system, causing a flare,” Dr. Wu explains. “And, on top of it, a lot of the patients have to stop their meds when they’re sick, which only fuels the flare.” Allergies and skin infections can also contribute to flares.
Unhealthy habits
While you could live your healthiest life and still deal with arthritis flares, there are some habits that are more commonly associated with periods of increased disease activity. The biggest one: smoking.
A study published in the journal Scientific Reports found that people who smoke have higher levels of inflammatory cytokines — molecules that promotes inflammation — in their blood than those who don’t smoke.
“Cigarette smoking may not directly contribute to arthritis flares, but it’s the strongest known lifestyle or environmental risk factor for rheumatoid arthritis,” says Dr. Gupta.
Dr. Gupta and Dr. Wu also note the following links between smoking and disease activity:
- Smokers have an increased risk of more severe RA
- Smokers may be less likely to achieve remission
- Smoking can decrease the effectiveness of some treatments
Another potential flare trigger is alcohol, which affects every person differently. Some people can have the occasional glass of wine without issues, while others notice more achy and sore joints after one drink.
Studies have found that, in general, drinking alcohol can worsen inflammation, cause nausea, and negatively impact sleep.
If you take methotrexate, one of the most commonly used treatments for RA, you should drink in moderation or avoid alcohol all together, says Dr. Wu. Depending on your medication dose and how much you drink, alcohol can lessen the effects of this medication and increase your risk of liver damage. Read more here about drinking alcohol while taking methotrexate.
Stress
While the connection between stress and arthritis flares isn’t totally clear, “stress is thought to dysregulate the immune system,” Dr. Gupta says. Stress can trigger immune system hyperactivity and reduce your immune system’s ability to fight off germs.
For example, recent study that found that higher levels of perceived stress were associated with an increased risk of developing inflammatory arthritis among individuals, all of whom were without active arthritis at study enrollment.
Stress also affects mentally and emotionally — when you’re very stressed, you may be less resilient and able to deal with flares when they do occur.
Disease progression
Some patients may worry that flares are a sign of disease progression, but Dr. Wu says that is rarely the case.
“[A flare] is not necessarily indicative that the disease is progressing,” she says. “If flares happen frequently, then I would say, more often than not, the medication is not completely controlling the disease and there is room for adjustment.”
Read more about what causes arthritis flare-ups.
How to Handle an Arthritis Flare
Working with your doctor is important when you have an arthritis flare. In some cases, they may recommend a short-term course of steroid medication to relieve the inflammation and pain. If symptoms persist for weeks or months, you and your doctor may need to discuss a change in your treatment plan.
But it’s also important to find ways to cope on your own. We asked community members on Facebook, Twitter, and Instagram how they handle arthritis flares. Here is some of their advice.
Get moving
Too much exercise due to overexertion of the joint(s) can cause an arthritis flare, but a little exercise can also go a long way in helping to tamp down a flare.
For people with inflammatory arthritis, staying active during a flare can help minimize symptoms, explains Dr. Wu. “But for people with osteoarthritis, which is the result of wear-and-tear to the joints over time, activity may trigger the flare.”
The goal is to start slow and small. “Any range-of-motion exercises, or even stretching exercises” can help lubricate and loosen the joints, providing some comfort,” says Dr. Gupta.
Even if it hurts a little, adds CreakyJoints member Helga D., “movement can temporarily take away the pain.” Start with a short walk just to get moving.
Wear a brace (or two)
“I wear a lot of braces during a flare,” says CreakyJoints community member Patricia M., including finger splints, knee, wrist, and elbow wraps, ankle-foot orthoses (AFOs) braces, rib wraps, and neck collars.
Other members also utilize wraps, braces, splints, and compression gloves during a flare, which Dr. Gupta says is a smart idea.“I often recommend braces to help rest and support the joints during a flare,” he says.
Heat things up
Many CreakyJoints community members agree that warming up painful spots can do a great deal to relieve symptoms during a flare. Here’s what works for them; try one and see what works for you:
- Scalding hot showers for temporary relief — Heather Y.
- A warm shower [and] hot wax treatment — Dave L.
- A warm bath with a hefty dose of Epsom salt — Ekaterina M.
Dr. Gupta has found many patients benefit from heat, but others prefer the cold. “I always let patients decide,” she says. “Both [cold and hot therapy] can help with joint flares, so it’s all about comfort.”
Read more about the difference between ice and heat therapy.
Try Voltaren gel
According to MedlinePlus, Volatren is an over-the-counter topical gel that contains diclofenac — a nonsteroidal anti-inflammatory drug (NSAID) that halts the production of substances in the body that cause pain and inflammation.
According to CreakyJoints community members Lin N. and Danielle N. it is a lifesaver during flares.
Though neither Dr. Gupta or Dr. Wu recommended Voltaren specifically, both agree that over-the-counter NSAIDs can provide temporary pain relief during flares.
Rest
While staying active is important, the body also needs rest to restore itself.
“I’ve realized that sleep is the key for me,” writes Bree T. “When I rest, I wake up with no pain. Unfortunately, life doesn’t always allow adequate sleep and that leaves me in pain.”
Resting doesn’t just mean curling up under the covers. It can also mean setting limits on your activities for the day.
“I finally learned to listen to my body and not power through as I was raised to do,” says Kathy M. “Now, I do what I can, when I can.”
Brenda K. has a similar approach: “I listen to my body and rest,” she writes. “I no longer feel bad or apologize to anyone for it. I will do better when I feel better.”
How to Prevent Arthritis Flares
When you live with arthritis, flares are bound to happen, but there are ways to reduce their occurrence and intensity.
Exercise
Dr. Gupta encourages patients to exercise regularly, as exercise keep your muscles and joints strong, which can better protect them. Exercise may also help reduce inflammation. That said, it’s important to ease into an exercise routine and make sure you don’t overdo it.
Dr. Gupta also emphasizes the importance of wearing the right gear, including comfortable, supportive shoes that aren’t too tight.
Talk to your health care provider to figure out what type (and how much) exercise is right for you. Being too active when you have osteoarthritis or not being active enough when you have inflammatory arthritis can increase joint pain.
Work with an occupational or physical therapist
Dr. Wu also suggests enlisting the help of an occupational and/or physical therapist. “They can help you make meaningful lifestyle changes so you can cope with the disability and still remain independent,” she says.
Keep in mind that occupational therapists and physical therapists provide different services, though both can be beneficial to people with arthritis.
- Occupational therapists work with patients to help make daily tasks easier. This may mean teaching them how to use assistive devices or providing ways to modify activities to make it easier on the joints.
- Physical therapists devise treatment plans for patients to improve their ability to move, reduce or manage pain, restore function, and prevent disability.
Learn more about the difference between occupational therapists and physical therapists.
Practice good hygiene and safety measures
Having inflammatory arthritis and treating it with immunosuppressant medications can increase your chances of getting sick from seasonal illnesses like the cold and flu. And if you do get sick, these factors can also make it harder to recover. Your immune system is too busy attacking the body to attack the germs. This can trigger an arthritis flare, says Dr. Wu.
Though getting sick may be beyond your control, there are some steps you can take to reduce your risk, including:
- Washing your hands thoroughly and often
- Wearing a mask in public
- Limiting your exposure to people who are or may be sick
- Staying up to date on vaccines, including flu, pneumonia, shingles, and COVID-19
Manage your weight
While arthritis can affect anyone regardless of how much they weigh, being overweight is associated with an increased risk of certain types of arthritis. It can also make it more difficult to manage arthritis because extra weight puts more stress on the joints, says Dr. Wu. Being overweight or obese is also linked with increased disease activity, perhaps due to higher levels of inflammation in the body.
Losing weight is not easy, especially if you have health conditions like arthritis that cause pain and fatigue, which make it difficult to exercise regularly and prepare healthy meal. If you need more support, talk to your doctor about your goals and discuss what resources may be available to you.
Practice stress management
Though there is no specific strategy for managing stress with arthritis, both Dr. Wu and Dr. Gupta agree that applying general stress management strategies — such as getting enough sleep, meditating, practicing yoga — can be useful.
Dr. Gupta also suggests participating in patient support organizations (such as CreakyJoints) to help mitigate stress. These support groups can provide a safe space to talk about your illness and exchange real-life advice.
Stick to your treatments
Not taking your medication as prescribed — skipping a treatment, self-adjusting the dosage, or stopping your therapy altogether — increases your risk for flares. Even if you are starting to feel better, don’t treatment without talking to your health care provider. It’s important to keep in mind that most arthritis treatments are about managing symptoms — not getting rid of them.
“Sometimes what happens is that a patient is doing well, so they stop taking the medication,” says Dr. Gupta. “But then the disease comes back so compliance to the recommended treatment is very important.”
How to Talk to Your Doctor About Arthritis Flares
Though there are many ways to prevent and manage a flare, ultimately the best thing you can do is talk to your doctor — and do it as soon as you notice symptoms.
“Being in touch with the doctor earlier rather than later, is, I think, the most important thing to do when you experience a flare,” Dr. Wu says. “I usually tell my patients not to handle this on their own. I’d rather they come to me than dabble in herbal remedies and things like that.”
When you can see your doctor, it is important to come with as much information as possible to help them better understand and assess your experience. Dr. Wu suggests keeping a detailed journal of your flares, including:
- When they occur
- How often they occur
- Intensity on a scale from one to 10
From there, you and your doctor can work together to come up with a treatment plan that minimizes your symptoms without interfering too much with your lifestyle.
“The goal of any rheumatologist is to keep patients flare-free at all times,” Dr. Gupta says. “We have very effective therapies available for pretty much all kinds of arthritis. There is no reason patients should be in intense pain in this era.”
Track Your Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Sign up.
Barr T, et al. Opposing effects of alcohol on the immune system. Progress in Neuro-Psychopharmacology & Biological Psychiatry. February 2016. doi: https://doi.org/10.1016/j.pnpbp.2015.09.001.
Diclofenac Topical. MedlinePlus. April 2021. https://medlineplus.gov/druginfo/meds/a611002.html.
Elisia I, et al. The effect of smoking on chronic inflammation, immune function and blood cell composition. Scientific Reports. November 2020. doi: https://doi.org/10.1038/s41598-020-76556-7.
Interview with Dee Dee Wu, MD, a rheumatologist at the Hospital for Special Surgery in New York City.
Interview with Samar Gupta, MD, a rheumatologist at the University of Michigan Hospitals-Michigan Medicine.
Polinkski KJ, et al. Perceived stress and inflammatory arthritis: a prospective investigation in the studies of the etiologies of rheumatoid arthritis cohort. Arthritis Care & Research. October 2019. doi: https://onlinelibrary.wiley.com/doi/10.1002/acr.24085.