At first glance, it might seem like gout and rheumatoid arthritis aren’t so different. Both cause pain, swelling, and stiffness of the joints that can limit your range of motion. However, the cause differs. RA is an autoimmune disease, which means the body’s own immune system attacks the joints, whereas the pain of gout is due to elevated levels of uric acid in the blood. But despite some similarities in symptoms, rheumatologists usually don’t have much trouble telling the two conditions apart.
“Cases of gout are often clear-cut because the flash of pain patients experience during a flare is so dramatic,” says Kelly A. Portnoff, MD, a rheumatologist at The Portland Clinic in Portland, Oregon. “It feels like a hot poker in their joint. Whereas if you have RA, the pain kind of creeps up on you.”
A patient’s age also provides clues. While rheumatoid arthritis can affect almost anyone, it most often first appears in women in their reproductive years. Gout tends to arise in one of two life stages: the late twenties/early thirties and the seventies and eighties.
“When gout strikes earlier, it’s often due to lifestyle factors that promote high levels of uric acid, such as meat-heavy diet and excessive alcohol intake,” Dr. Portnoff says. When gout appears later in life, it’s more likely the result of kidney damage or health conditions that increase the risk of gout, such as high blood pressure, diabetes, and heart disease.
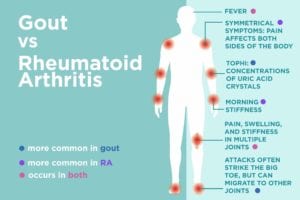
There are also some differences in the symptoms of gout and rheumatoid arthritis, as you’ll see below.
Common Symptoms of Gout
Pain that migrates: Gout usually affects the big toe, but it can also occur in the ankles, knees, elbows, wrists, and fingers. The symptoms are rarely symmetrical, and the location varies from flare to flare. For example, an attack in the left big toe might be followed by an attack in the right toe, and the next gout attack might strike one of the knees or wrists.
Fever: People with RA do sometimes experience a fever, but it’s much more commonly seen in those with gout, says Dr. Portnoff: “The burden of inflammation in a gout flare and the body’s robust response to it can be so great that it causes a fever.”
Tophi: Over time, people with chronic gout can develop tiny, hard lumps in the affected joints. These lumps, called tophi, are concentrations of uric acid crystals. They can also form in the kidneys and lead to kidney stones.
Common Symptoms of Rheumatoid Arthritis
Symmetrical symptoms: In RA, joint pain usually affects both sides of the body. Symptoms typically begin in the small joints in the hands and feet; as the disease progresses, pain can develop in the wrists, knees, ankles, elbows, hips, and shoulders.
Morning stiffness: The pain of RA is typically at its worst in the morning, which causes a period of stiffness that can last an hour or longer. Motion helps ease RA symptoms, so people generally feel better later in the day as they accumulate more activity.
Gout vs. Rheumatoid Arthritis: Getting the Correct Diagnosis
The Role of Blood Tests
With no definitive blood test available for RA, doctors instead look for certain antibodies in the blood that would suggest its presence, such as antinuclear antibodies, rheumatoid factor, and anti-cyclic citrullinated peptide (anti-CCP) antibodies. Your rheumatologist will also order a complete blood count to see if you have anemia, which is common among those with RA.
“RA is more difficult to identify than gout because measuring the amount of uric acid in the blood is considered a definitive test for gout,” Dr. Portnoff says. However, levels of uric acid are actually lower during a gout flare, so your doctor will want to repeat the test when symptoms subside.
The Role of Imaging Tests
Both RA and gout can cause joint erosion, so rheumatologists will order X-rays to look for this. X-rays can also detect the beginnings of tophi, but Dr. Portnoff says they’re not an essential part of the diagnostic process for gout because a patient’s clinical history, physical exam, and uric acid testing will identify gout.
Getting Prompt Treatment for Gout or RA
If you’ve been experiencing symptoms of either condition, you should see your doctor as soon as possible because both can cause significant joint damage if a diagnosis is delayed. However, Dr. Portnoff notes that the pain gout causes is so intense that patients with gout rarely put off seeing a doctor when they’re having an attack. (Taking medication regularly to treat gout, even when you’re between attacks, is important though.)
There’s no cure for gout or RA, but there are several good treatments available for the two conditions. Some pain relief treatments, including NSAIDs and corticosteroids, are recommended to help manage both RA and gout. Because RA is an autoimmune disease, patients may also take disease-modifying immunosuppressant drugs such as methotrexate or other DMARDS (disease-modifying anti-rheumatic drugs) or biologics.
Gout, on the other hand, may be treated with the drug colchicine, which relieves pain and helps prevent future attacks. Rheumatologists may also prescribe drugs called xanthine oxidase inhibitors (which reduce the amount of uric acid your body makes), and sometimes combine those with medications called uricosuric drugs that improve your kidneys’ ability to remove uric acid from your body. People with gout are also advised to limit foods that promote high levels of uric acid, including red meat, alcohol, and shellfish. However, diet changes alone cannot usually control gout symptoms, and medications are necessary to help prevent complications.
Keep Reading
- Lupus vs. Rheumatoid Arthritis: What’s the Difference?
- This Is What Gout Does to Your Bones Even When You’re Not Having an Attack
- Gout Home Remedies: Here’s What You Can (and Can’t) Do to Relieve Gout Pain Fast





