Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
If you have rheumatoid arthritis (RA) or another chronic rheumatic condition, your rheumatologist’s office may have become like a home away from home over the years. After all, many patients with autoimmune or inflammatory arthritis need regular checkups every three to six months, or even more often.
Over the last year, however, the COVID-19 pandemic has created an increased demand for “telerheumatology” — rheumatology visits delivered over video/audio services like FaceTime, Skype, or special medical applications or websites used for telehealth. In fact, about 66 percent of patients reported having a telehealth appointment in the last year, according to the 2020 Rheumatic Disease Patient Survey conducted by the American College of Rheumatology (ACR).
“Telehealth is a great tool during in the throes of a pandemic,” says Howard Blumstein, MD, a rheumatologist at Rheumatology Associates of Long Island in New York. “It can be safer in terms of [reducing your exposure to] the coronavirus, but it’s not always best in terms of your health.”
In-person doctor visits are often necessary for the optimal management of complex medical conditions like autoimmune or inflammatory rheumatic diseases, including rheumatoid arthritis, psoriatic arthritis, axial spondyloarthritis, and others.
When you have a chronic rheumatic disease, there can be serious “silent” risks of avoiding medical care. Persistent inflammation that goes unchecked can lead to irreversible joint damage and may impact other parts of your body, like your heart and lungs.
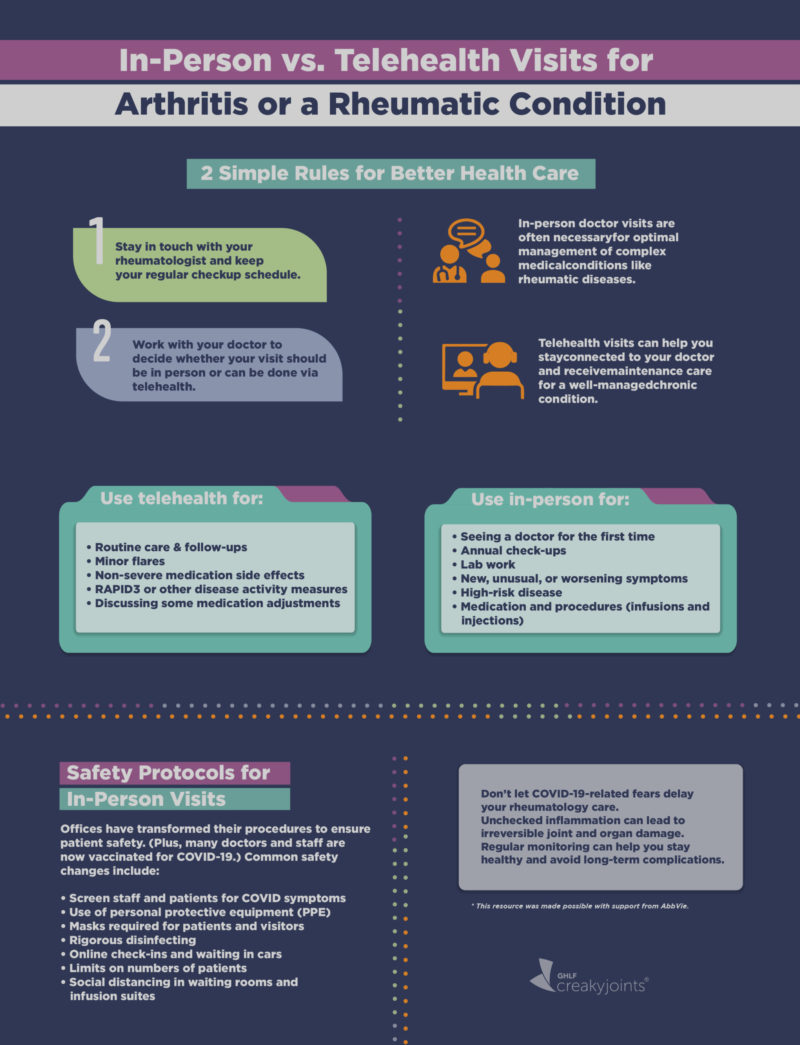
This is why it is so important to:
- Stay in touch with your rheumatologist and keep your regular checkup schedule. For many people, this means seeing the doctor every three to six months (or more often if needed).
- Work with your doctor to decide whether your visit should be in person or can be done via telehealth.
Weighing the Risk and Benefits of Telehealth vs. In-Person Visits
While waiting in your car to be called into your rheumatologist’s office and donning a mask may feel like the new norm for many rheumatic disease patients, others are still concerned about whether it is safe to see the doctor in person. This may be causing people to put off doctor’s visits altogether, which has its risks. In the ACR patient survey, for example, there was a 52 percent decline from 2019 to 2020 in the percentage of respondents who said they were currently being treated by a rheumatology provider.
All of the experts CreakyJoints has spoken with agree: Allowing coronavirus-related fears to delay your rheumatology care is not the answer.
“If you have active RA or another rheumatic disease, you need close monitoring of your disease activity and medications. If you go many months without seeing your doctor, this can result in having disease flares or medication side effects [that don’t get treated],” says Kai Quin, MD, a rheumatologist at Ohio State University’s Wexner Medical Center.
Routine rheumatology visits are critical for managing symptoms, assessing disease activity and progression, watching for medication side effects, monitoring comorbid (co-occurring) health conditions that may require additional specialists (such as heart, lung, or kidney doctors), and staying on top of your health.
As we continue to move forward in and beyond the pandemic, telehealth may act more as triage to help you and your doctor determine when you need to come in for a physical exam, go for bloodwork, or get an ultrasound or X-ray. In a recent paper, the American College of Rheumatology noted that telemedicine should be used “as a tool with the potential to increase access and improve care for patients with rheumatic diseases, but it should not replace essential face-to-face assessments conducted at medically appropriate intervals.”
While the decision of whether to have an in-person vs. telehealth visit as the coronavirus pandemic continues is one that’s best made between you and your rheumatologist, several factors may be considered:
- Your symptoms
- The severity of your condition
- Your doctor’s recommendations
- Your location and local rates of COVID-19
- Your access to transportation and proximity to the doctor
- Whether testing or procedures are necessary
If you have a health issue and are considering whether to come in to be evaluated, Dr. Quin recommends asking yourself the following:
- Have you had this before? If so, what did the doctor tell you was causing it and what was the recommended care for improving it?
- How severe is it? Is it a minor nuisance, or a sudden or worsening symptom?
- Are your vital organs impacted? “If there is any damage from the immune system on the vital organs — if you lose any lung or kidney function — it’s often not reversible and very time sensitive,” says Dr. Quin. “If you wait a couple days, weeks, or months, it will likely be much worse than the small amount of risk someone would take coming into clinic.” If you know you already have organs affected by your rheumatic condition, it’s important to make sure you see your health care provider in person regularly.
- How is your emotional health? “Patients tell me a lot more during person-to-person visits beyond what impacts them from a physical standpoint,” says Dr. Quin. “With video visits, even though they are face-to-face, there is more of a barrier.”
Telehealth Visits Work Best For:
Telehealth can be a great way to assess the following types of issues:
- Routine care and follow-up. If you’re a stable patient with an established diagnosis of RA, have a good rapport with your rheumatologist, and fill out nothing new on your health assessment questionnaire, telehealth every three months works fine, says Dr. Blumstein.
- Minor flares and stiffness. “You can see if someone has some issues or can’t make a fist over telehealth, and then get an idea whether it needs to be addressed further,” says Dr. Blumstein.
- Non-severe medication side effects like fatigue, sleep issues, gastrointestinal issues, or headaches.
- RAPID3 questionnaires, or other disease activity measures, can be done via telehealth to inform your rheumatologist about how your condition is doing without the need for blood tests to check inflammation levels.
- Some medication adjustments, including changing dosages to better manage symptoms. However, notes Dr. Blumstein, if you’re taking medication, you still need to get regular blood tests done. And some doctors prefer to discuss bigger medication changes in person, such as starting a new medication or switching from one kind of medication to another (say, going from an oral pill to an injectable biologic).
In-Person Visits Work Best For:
New patients
While it is possible for rheumatologists to see new patients via telehealth, many prefer to do so in person, especially if someone does not have an established diagnosis. Your doctor will likely want to perform a physical exam, order bloodwork and imaging, and discuss your personal and family medical history.
With rheumatology we are so dependent on physical exams that a new diagnosis would be incomplete via telehealth, says Dr. Quin. “I’ve made a diagnosis in the past where the patient had minor symptoms and a lab abnormality, but one finding on a physical exam made me think about another diagnosis and get more testing, which confirmed the presence of a different disease,” he says.
Yearly visits
“If you have well-controlled RA, no medication side effects, and all the monitoring and labs look good, a once-a-year in-person exam would be reasonable and important,” says Dr. Quin. This is because slow, insidious joint damage might not cause symptoms, he adds.
Lab work
It’s important for your doctor to monitor your bloodwork to make sure things like your blood count and liver function are healthy, especially if you start a new medication or adjust the dose.
Dr. Quin recommends patients make an appointment for an in-person visit the same day they come in for labs. “It will be beneficial to be seen in clinic and will save you a trip,” he says.
New or worsening symptoms
Especially during the pandemic, it may be tempting to brush off new or worsening symptoms or wait to see if they go away. But you know your body best: If something doesn’t feel right, get it checked out. For example, a psoriatic arthritis patient who has been complaining of worsening ankle pain and concerns of enthesitis should come in to see us, says Vinicius Domingues, MD, a rheumatologist in Daytona Beach, Florida.
New pain or swelling
“Any time a patient thinks their joint is swollen, I would recommend coming in to get evaluated,” says Dr. Quin. “Joint swelling as a whole can sometimes be difficult to access via telehealth. We can do a video where you can show the rheumatologist the joint, but it’s often a subtle finding on an exam. Just the feel of the joint can guide us to the cause,” and make a decision about how to adjust treatment.
Patients with high-risk disease that involves a vital organ
Having rheumatoid arthritis with interstitial lung disease, for example, should require in-person visits. “Not that you have to come in person every single time,” says Dr. Quin, “but someone in that scenario should not be treated solely through telehealth.”
Especially if there’s possible fluid in your lungs, it’s essential to come in. Your physician can’t hear your lungs via video.
Medications and procedures such as infusions or in-office injections
Patients on biologic infusions need to come into the office, as do patients who need a cortisone shot or a joint aspirated, says Dr. Blumstein. Read more about how to protect yourself during an infusion.
The bottom line: While a telehealth visit is better than avoiding the doctor completely, in-person visits are still important to stay on top your health and prevent any complications or worse problems down the line.
“We know that if patients are not receiving optimal care, their underlying disease is certainly at risk,” says Dr. Quin. “Whereas with COVID-19, in a relatively safe environment where all the staff are taking measures to keep patients safe, the benefit of getting care is much higher than the potential risk of exposure to COVID.”
Keep in mind that doctor’s offices now have a year’s worth of experience keeping their patients and staff safe and mitigating COVID-19 exposure. What’s more, many health care providers and staff are now fully vaccinated against COVID-19, in addition to strictly following prevention guidelines and safety protocols.
Read more about the safety protocols rheumatologists are following to keep patients safe during the pandemic.
This resource was made possible with support from AbbVie, Inc.
Want Better Virtual Care with Your Rheumatologist?
For personalized advice on getting the most out of your rheumatology telehealth visits, check out eRheum.org.
2020 Rheumatic Disease Patient Survey. American College of Rheumatology. http://simpletasks.org//wp-content/uploads/2020/09/ACR-Survey-2020.pdf.
ACR Infusion Guidance During COVID-19 Crisis. American College of Rheumatology. https://www.rheumatology.org/Portals/0/Files/ACR-Infusion-Guidance-COVID-19.pdf.
American College of Rheumatology Position Statement on Telemedicine. https://www.rheumatology.org/Portals/0/Files/Telemedicine-Position-Statement.pdf.
ACR Telehealth Provider Fact Sheet. American College of Rheumatology. May 7, 2020. https://www.rheumatology.org/Portals/0/Files/ACR-Telemedicine-Fact-Sheet-2020.pdf.
Interview with Douglas Roberts, MD, assistant clinical professor of medicine at the University of California Davis Medical School and founder of PainSpot.org
Interview with Howard Blumstein, MD, rheumatologist at Rheumatology Associates of Long Island in New York
Interview with Kai Quin, MD, rheumatologist at Ohio State University’s Wexner Medical Center
Interview with Vincent Domingues, MD, a rheumatologist in Daytona Beach, Florida