Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
I’m a rule follower. That means during this global pandemic, I wear a mask religiously, I socially distance, and I don’t invite anyone into my house, though I’d make an exception for Edward Cullen (that’s a Twilight reference, btw).
So when my rheumatologist, along with the entire rheumatology medical community, advised patients with rheumatoid arthritis to continue their biologic infusion treatments during the pandemic (unless they actually had a COVID-19 infection), I did. I’ve gotten my Remicade infusions twice so far during this crisis — as scheduled — even though I knew that anytime I stepped foot outside my house, there could be a greater-than-zero chance I’d contract coronavirus.
I implicitly trusted my doctor’s office to keep me safe, so that wasn’t the issue. I think what was most scary to me about going to my infusion was that sometimes the treatments make me feel sick afterward, almost as though I have a mild flu for a few days. And that the sensation of feeling sick would trigger more crippling anxiety and panic attacks, which I’d been experiencing for the last four months on and off.
Well, maybe it was a self-fulfilling prophecy, because that’s exactly what happened at my last infusion. For whatever reason, I had a bad reaction, almost immediately after the treatment, and worse than normal. My face turned beet red. The inside of my body felt like a furnace and my chest felt heavy, tickly, and wheezy. I was so severely fatigued that I had to take naps in the afternoon or I couldn’t function. I was foggy, dizzy, and off-balance. I just did not feel right.
Making Sense of Strange Symptoms
I was truly scared I had coronavirus, even though I knew what I was experiencing were all well-known possible side effects of my infusion. Still, I frantically Googled my nearest corona testing site and had to force myself tonot make an appointment.
“This is not COVID, this is my infusion,” I kept reminding myself out loud, over and over.
Sure enough, a week later — a few days longer than usual — I finally felt “normal” again.
I’d been in such a state that I forgot or refused to remember that I usually feel like this after my infusion. I’ve had rheumatoid arthritis for more than 10 years, so it should be old hat. I usually think about it now as little as humanly possible.
But, for better or worse, the COVID-19 pandemic has forced me to pay much closer attention to my body again.
Avoiding Denial
This is not easy for someone like me.
I consider myself non-binary/transgender, so I’ve spent most of my lifetime hating and ignoring the body I was born in. When I got rheumatoid arthritis it was just another reason for me to think my body was conspiring against me and I dug further into denial.
But I don’t have the luxury of sticking my head in the sand when it comes to coronavirus. For hundreds of thousands of Americans, it clearly has been an urgent matter of life and death.
Having a chronic illness like RA (and the medications I take to control it) could possibly put me at a higher risk than the general population — or not, nobody really knows still — so my daily decisions matter.
Playing Doctor
So yeah, I’m paying closer attention to my aches, pains, creaks, and wheezes these days. And I’m learning so much.
Take, for instance, my body temperature. A fever is a sign of COVID-19, so at the beginning of the pandemic I took my temperature several times a day. I learned that when I wake up in the morning it can be as low as 95 degrees. The first time I saw that, I was like, OMG, am I dead? Then later in the day it shot up to 98.7 and I was like, OMG, am I gonna die?
But then I frantically Googled again and found a study that says the German scientist guy who claimed the average was 98.6 around 200 years ago was wrong. Today, new research claims the average temperature is closer to 97.9 but it also depends on the person, the time of day, and a bunch of other factors.
According to the U.S. National Library of Medicine’s MedlinePlus, a fever is “a higher-than-normal body temperature.” So while mine fluctuated a lot every day, it also fluctuated consistently every day — and has never gone past 99. The U.S. Centers for Disease Control and Prevention (CDC) officially considers a fever to be above 100.4 F.
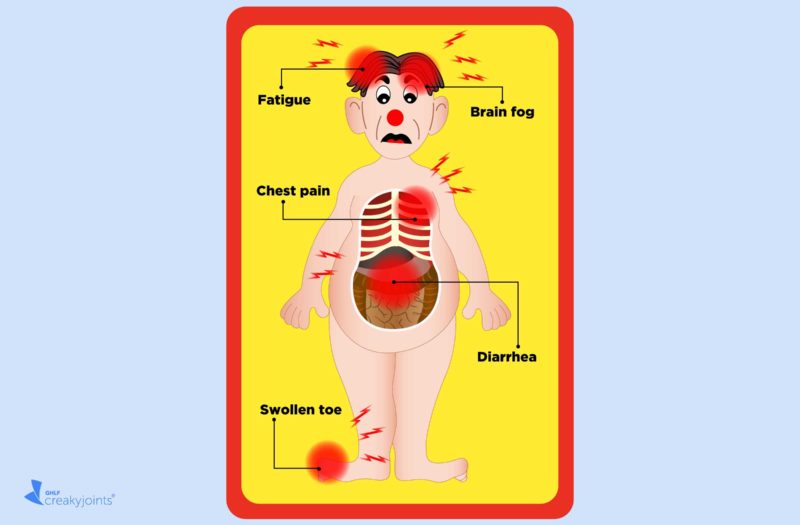
Corona and RA: Freaking Out About the Overlap
Knowledge is power but it can also be nerve-wracking. Besides fever, many other coronavirus symptoms are vague and/or common, such as headaches or nausea. Also, so many — too many — are similar to RA symptoms and medication-related side effects. That makes it way too easy to freak yourself out and misdiagnose yourself.
For example:
Diarrhea
Diarrhea is listed as a sign of COVID-19. But my meds, especially methotrexate, give me crazy IBS. Every time I’m on the terlet, I’m like, is that you, ’Rona? Probably not. It’s probably the vanilla milkshake I had DoorDash deliver from Burger King, which cost $27 with delivery fees, service fees, and tip. That’ll give you diarrhea.
Fatigue
Speaking of nausea, anyone with a chronic disease has explained ad nauseum to anyone who will listen that being tired and being fatigued are not the same. But are coronavirus fatigue and RA fatigue the same? Who knows? All I know is that I go to bed at 8 PM a lot lately. But that’s probably boredom. How many more Netflix shows can one person binge? Unsolved Mysteries, Taste the Nation, I can’t. I’m sorry, Padma, it’s over.
COVID Toe
Is that burning sensation in my big toe an RA flare or COVID toe? Probably neither. Perhaps it’s gout exacerbated by mail-ordering in and eating 40 pounds of steaks and sausages from an organic farm in Wyoming.
Cognitive symptoms
Is my brain fog actually COVID confusion? Why did I just put the remote control in the refrigerator? Nah, it’s probably just the mind-blowing realization that I may never spend quality time with another human being in person other than my mother (with whom I live) ever again.
Chest pain
After my infusion, I was having burning chest pain, which can be another sign of COVID. But using my championship caliber Googling skills, I, Dr. Baer, determined I had anxiety-induced GERD, likely from eating an entire pan of Rice Krispies Treats then immediately going to bed at 8 PM.
Read more here about making sense of coronavirus symptoms when you have an autoimmune condition.
Focusing on *My* Normal
Listen, I’m not a doctor and I don’t play one on TV. I don’t even like watching doctor shows; they make me queasy (see nausea above). I’ve fallen down some steep Internet rabbit holes looking for any medical research or articles that prove I do not have coronavirus. But the bottom line is that I do not know what I’m talking about. Nobody really does. Just look at the debate about asymptomatic carriers of coronavirus.
So, I think moving forward, my goal will be to continue to pay close attention to my body. If things seem way different than normal — which means my normal — I’ll go get myself checked out by a real doctor or get tested for COVID-19 for real. I’m making jokes here but it’s not all that funny. It’s very real.
My paranoia is also very real, but it’s like, hey, join the club. That is also a new normal. You don’t have to have a chronic illness like rheumatoid arthritis to obsess about and be terrified you’ll contract this horrible, out-of-control virus. The one thing I can control is trying to be as safe and as smart as possible. I rarely leave the house and if I do, I’m masked and at least six feet away from the nearest, mask-less Karen throwing a hissy fit about something or other.
That decreases my chances a lot. And that is all I can do.
Get Free Coronavirus Support for Chronic Illness Patients
Join the Global Healthy Living Foundation’s free COVID-19 Support Program for chronic illness patients and their families. We will be providing updated information, community support, and other resources tailored specifically to your health and safety. Join now.
Definitions of Symptoms for Reportable Illnesses. Quarantine and Isolation. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/quarantine/air/reporting-deaths-illness/definitions-symptoms-reportable-illnesses.html.
Fever. MedlinePlus. U.S. National Library of Medicine. https://medlineplus.gov/fever.html.
Shmerling RH. Time to redefine normal body temperature? Harvard Health Publishing. Harvard Medical School. March 17, 2020. https://www.health.harvard.edu/blog/time-to-redefine-normal-body-temperature-2020031319173.
Symptoms of Coronavirus. Coronavirus Disease 2019 (COVID-19). U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.