Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
You may have been one of the many patients who took advantage of telehealth during the COVID-19 pandemic. However, now that rates of COVID are dropping and more people are becoming fully vaccinated, it poses the question: How safe is it to go to in-person doctor’s appointments if you’re fully vaccinated but immunocompromised?
Although many experts believe that immunocompromised people get some protection from the vaccine, they may not have the same level of protection as immunocompetent people.
Depending on which medications you take and other factors, “if you’re immunocompromised and fully vaccinated, what we know right now is that you probably have some protection, but likely not the same amount of protection from the vaccine as an immunocompetent patient might have,” says Sajal Tanna, MD, a transplant infectious diseases physician at Northwestern Medicine who treats immunocompromised patients.
For this reason, many experts urge immunocompromised patients, even those who are fully vaccinated, to continue taking standard mitigation efforts until is known about how the vaccine works in these patients. This includes people who take certain immunosuppressive medications, like methotrexate and rituximab, as these drugs may decrease your immune response to the vaccine, leaving you less protected than a fully vaccinated person who is not taking such medication.
But if you are immunocompromised, and therefore possibly also at a higher risk for COVID-19 complications, you may have to see doctors on a more regular basis than those who are not, which can make the whole situation feel like a catch-22.
As more places loosen restrictions like requiring face masks and social distancing, immunocompromised patients may feel less safe while doing everyday activities and errands. But going to a doctor visit in person is still very different — and safer — than, say, buying groceries in a store full of maskless shoppers.
Here’s everything to know about returning to in-person doctor appointments if you’re fully vaccinated but immunocompromised.
1. Doctor’s Offices May Be the Safest Places to Visit
Although many mask and social distancing regulations have relaxed in public spaces based on the latest guidelines from the U.S. Centers for Disease Control and Prevention (CDC), your doctor’s office is likely still following standard mitigation efforts for the safety of its staff and patients.
“In-person doctor’s visits are actually one of the safest places you can be outside of your own home,” says Dr. Tanna. “Even with the new CDC guidance of lifting mandatory masking, health care settings are one environment where everyone is still mandated to be masked. So I think it’s quite safe, especially in the setting of the decreasing coronavirus rates in our country and local communities.”
In May, the CDC clarified that its new mask recommendations for those fully vaccinated against COVID-19 do not apply to health care settings — meaning staff, patients, residents, and visitors should still wear masks as recommended in all health care facilities, per the American Hospital Association, which had requested the clarification.
The CDC also noted in April that, “health care facilities should continue to follow the infection prevention and control recommendations for unvaccinated individuals (e.g., quarantine, testing) when caring for fully vaccinated individuals with an immunocompromising condition.”
Most states are following the CDC’s guidance to maintain mask rules for everyone (regardless of their vaccination status) in health care and long-term facilities, reports AARP.
How long this will last may depend on vaccination rates in your state. For instance, New York State lifted COVID-19 restrictions on June 15, 2021, but specified that, “the State’s health guidelines continue to be in effect for large-scale indoor event venues, pre-K to grade 12 schools, public transit, homeless shelters, correctional facilities, nursing homes, and health care settings per CDC guidelines.” The CDC has not made any indication that its guidance will change in the near future.
Naturally, you’ll also have a smaller risk of contracting COVID-19 at a doctor’s office if case numbers in your local community are low, which is true for most regions of the country right now. As of mid-June, COVID-19 case numbers in the United States have fallen to the lowest point since testing became widely available — and fewer deaths are being reported each day than at any point since March 2020, per the New York Times.
“Overall, I’m really encouraged by the fact that a large fraction of people in the United States are being vaccinated and that’s really driving the community rates to go down,” says Dr. Tanna. “As those rates go down, it really does protect our immunocompromised patients.”
The best way to protect yourself at the doctor’s office and beyond is to get vaccinated and to encourage those in your immediate circle to get vaccinated as well.
2. Protect Yourself with a Few Tips
If you’re in a small waiting room, there could be a risk of infectious particles building up as aerosols in the air, though most doctor’s offices will have measures in place to protect against this, such as proper ventilation.
According to the CDC, exposure to SARS-CoV-2 — the virus the causes COVID-19 — can occur when:
- Respiratory droplets and particles carrying the virus directly come in contact with your mouth, nose, or eyes.
- You inhale very fine respiratory droplets and aerosol particles (these can remain suspended in the air).
- You touch your mouth, nose, or eyes with hands that have come in contact with virus-containing respiratory fluids.
“We think there is aerosol transmission, but it’s likely not the primary mode,” says Dr. Tanna. “It’s probably mostly respiratory droplets. In a doctor’s office where everyone is masked and probably a decent fraction are vaccinated and likely don’t have the coronavirus, I think it’s actually quite safe.”
Additionally, current evidence suggests that contaminated surfaces don’t contribute substantially to new COVID-19 infections, per the CDC.
Of course, there is still a lot you can do to protect yourself before and after your appointment, such as:
- Call ahead to ask what risk mitigation efforts are being followed at the doctor’s office.
- Stick to your appointment time and avoid coming in too early so the waiting room doesn’t get overcrowded.
- Ask to be called when it’s time for your appointment and wait nearby outside or in your car.
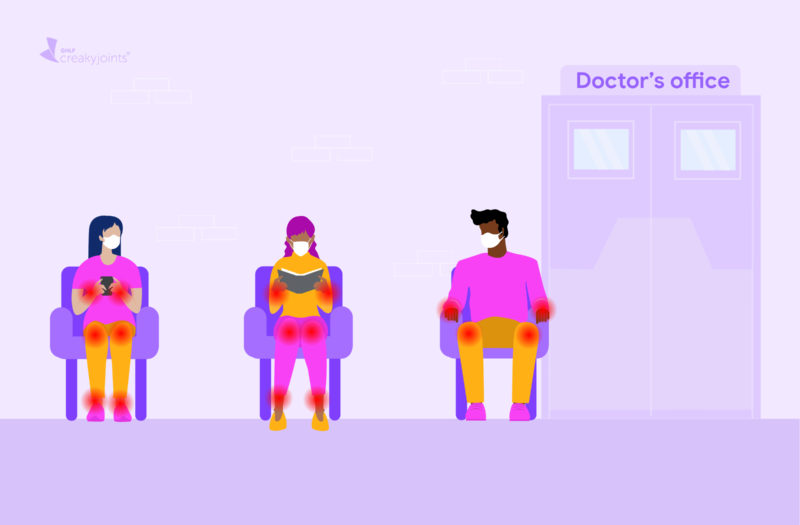
- If you do wait in the waiting room, choose a seat at least six feet from other patients.
- If you need to eat a meal at a medical center between doctor’s appointments, try to do so outside or in your car.
- Keep your mask on at all times unless otherwise instructed by your doctor.
- Wash your hands or use alcohol-based hand sanitizer after touching surfaces.
“I think the most important thing is to remember to wear your mask throughout your entire travel to the doctor’s office, including if you have a long day at the hospital,” says Dr. Tanna. “When you go to the hospital cafeteria or you’re in the parking garage and elevators, you really need to make sure you’re wearing your mask.”
Research from the CDC has found that double masking or knotting and tucking a medical procedure mask can reduce your exposure to infectious particles from an unmasked person by 83 percent and 64.5 percent, respectively. Your hospital or doctor’s office may even ask you to wear a surgical mask that they provide.
3. Get Prescriptions Through Mail Order
Waiting at the pharmacy to pick up medications could add to your exposure to COVID-19 if people around you are not masked or vaccinated. To avoid additional risk, consider getting your prescription through the mail or ask your doctor to prescribe larger supplies of medications so you don’t have to visit the pharmacy as often, per the Mayo Clinic.
Some pharmacies also offer drive-through, curbside, or delivery options.
4. Follow Precautions While Commuting to Your Appointment
If you need to take public transportation to get to your appointment, you can minimize your exposure to COVID-19 by wearing a mask, social distancing when possible, and getting vaccinated.
The CDC is working to amend the January 29, 2021 order that required face masks to be worn by anyone on public transportation, so that fully vaccinated people in outdoor areas of public transportation don’t need to wear one. Until then, it says it will use discretion in enforcing the order so that fully vaccinated individuals can go without masks in these outdoor settings (think a bus stop or outdoor subway platform).
As of now, masks are still required when indoors on public transportation, including on subways, trains, buses, and in taxis or ride-shares. However, people are not required to wear a mask indoors on public transportation under certain circumstances — say, if they’re eating or drinking for brief periods of time.
If you’re traveling to the doctor’s office via public transportation like a bus, train, or ride-share, the CDC’s general guidance for protecting yourself remains the same:
- Wear a mask covering your nose and mouth.
- Try to keep at least six feet from those not in your household (say, when you’re waiting for the bus or selecting seats on a train).
- Wash your hands with soap and water for at least 20 seconds or use hand sanitizer containing at least 60 percent alcohol before and after using transportation.
- Consider traveling during non-peak hours when there are fewer people.
- Refrain from eating or drinking on public transit so you can keep your mask on.
- If you’re in a ride-share, ask the driver to improve ventilation by opening the windows or setting the air conditioning to non-recirculation mode.
5. Know When Telehealth Visits Are Appropriate
If you’ve taken advantage of telehealth medical appointments over the past year, you can certainly continue to do so when it’s possible.
“Telehealth has really been a great benefit that we’ve incorporated into our practice in the past year,” says Dr. Tanna. “The best thing to do is to ask your own physician if telehealth is appropriate for your condition.”
Whether or not telehealth is appropriate for a given appointment will depend on a number of factors. Read more here about how to decide whether a telehealth vs. in-person rheumatology visit is right for you.
“People who are ideally suited for telehealth are those on maintenance therapy and stable treatments, or who have had no major interim changes in their health,” says Leonard Calabrese, DO, Director of the R.J. Fasenmyer Center for Clinical Immunology at Cleveland Clinic.
Many follow-up evaluations can easily be done over telehealth. A virtual visit may also be an appropriate option for general questions about your medication or mild symptoms. But “if there are a lot of joints with pain or swelling, other symptoms like a rash or shortness of breath, or anything in addition to the joint pain, an in-person visit is most likely required,” says clinical rheumatologist Magdalena Cadet, MD, Associate Attending Physician at NYU Langone Health in New York City.
Similarly, if you have new or worsening symptoms or you have a high-risk disease that involves a vital organ, it’s best to see a doctor in-person. And of course, blood tests, lab work, and certain treatments like biologic infusions will need to be done at your doctor’s office. It’s also usually best to see a new provider for the first time in person.
6. Don’t Neglect Your Medical Care
During the pandemic (particularly the early days of it), experts saw a concerning drop in patients seeking both routine and emergency care. However, it’s very important to stay on top of your appointments so you don’t miss opportunities to manage your condition or detect new issues, which could impact your health in the long-run.
“Stay in contact with your providers, and get to your visit,” says Dr. Calabrese. “Don’t ignore your health and don’t stop your medications on your own.”
Work with your doctor to determine when you need to come in for an in-person visit and when you can be treated via a telehealth visit. Meeting with your doctor virtually when possible may make it easier to keep appointments.
And remember, those appointments in and of themselves could help protect you from COVID-19.
“It’s thought that one of the biggest risk factors for having severe outcomes of COVID-19 in the rheumatic disease population is having under-controlled or highly active disease,” says Dr. Calabrese. “Thus, avoiding care under any circumstances — and allowing disease to become active — is itself a major risk for severe outcomes for COVID-19.”
Get Free Coronavirus Support for Chronic Illness Patients
Join the Global Healthy Living Foundation’s free COVID-19 Support Program for chronic illness patients and their families. We will be providing updated information, community support, and other resources tailored specifically to your health and safety. Join now.
CDC: Masks still required in health care settings. American Hospital Association. May 17, 2021. https://www.aha.org/news/headline/2021-05-17-cdc-masks-still-required-health-care-settings.
Coronavirus in the US: Latest Map and Case Count. The New York Times. June 11, 2021. https://www.nytimes.com/interactive/2021/us/covid-cases.html.
Governor Cuomo Announces COVID-19 Restrictions Lifted as 70% of Adult New Yorkers Have Received First Dose of COVID-19 Vaccine. New York State. June 15, 2021. https://www.governor.ny.gov/news/governor-cuomo-announces-covid-19-restrictions-lifted-70-adult-new-yorkers-have-received-first.
How to safely go to your doctor during the COVID-19 pandemic. Mayo Clinic. October 21, 2020. https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/how-to-safely-go-to-your-doctor-during-coronavirus/art-20486713.
Interim Public Health Recommendations for Fully Vaccinated People. COVID-19. U.S. Centers for Disease Control and Prevention. May 28, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated-guidance.html.
Interview with Leonard Calabrese, DO, Director of the R.J. Fasenmyer Center for Clinical Immunology at Cleveland Clinic
Interview with Magdalena Cadet, MD, Associate Attending Physician at NYU Langone Health in New York City
Interview with Sajal Tanna, MD, a transplant infectious diseases physician at Northwestern Medicine who treats immunocompromised patients
Markowitz A. State-by-State Guide to Face Mask Requirements. AARP. June 14, 2021. https://www.aarp.org/health/healthy-living/info-2020/states-mask-mandates-coronavirus.html.
Protect Yourself When Using Transportation. COVID-19. U.S. Centers for Disease Control and Prevention. June 11, 2021. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/using-transportation.html.
Requirement for Face Masks on Public Transportation Conveyances and at Transportation Hubs. COVID-19. U.S. Centers for Disease Control and Prevention. June 10, 2021. https://www.cdc.gov/coronavirus/2019-ncov/travelers/face-masks-public-transportation.html.
Science Brief: SARS-CoV-2 and Surface (Fomite) Transmission for Indoor Community Environments. COVID-19. U.S. Centers for Disease Control and Prevention. April 5, 2021. https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/surface-transmission.html.
Updated Healthcare Infection Prevention and Control Recommendations in Response to COVID-19 Vaccination. COVID-19. U.S. Centers for Disease Control and Prevention. April 27, 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-after-vaccination.html.