Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
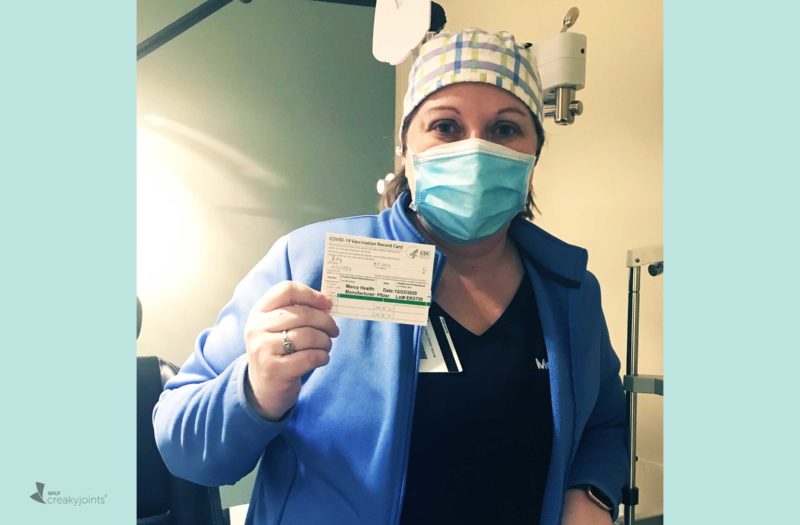
Kristen Schlichting, 38, has had a number of close calls with COVID-19 since the pandemic began. But now that she is vaccinated, she hopes she can keep doing her job as an eye surgery nurse with a lot more reassurance.
In her St. Louis, Missouri hospital, Kristen’s job involves preparing patients for surgeries for conditions like glaucoma and cataracts, as well as injuries and trauma. She’s responsible for doing eye exams that are 20 to 30 minutes long, during most of which she is fewer than two inches away from a patient’s face. She sees about 20 patients a shift and has been working steadily throughout the pandemic.
During her shifts, Kristen wears an N95 respirator mask (which she purchases herself to ensure she always has enough), a surgical mask, and a face shield — and patients wear cloth face masks as well. But it’s clear that Kristen’s job is the very definition of prolonged close contact.
This ongoing, high level of exposure is concerning for anyone, but it’s especially worrisome for Kristen, who has underlying health issues and takes medications that could increase her risk for COVID-19 complications.
Kristen has had ankylosing spondylitis (AS), a type of inflammatory arthritis that causes debilitating back and hip pain, as well as other symptoms, for more than 20 years. She currently takes the biologic infliximab (Remicade), which affects immune system function. She has lung and kidney damage (only one kidney left) as a result of extensive injuries from a rollover car accident she suffered as a passenger at age 16. And she is currently experiencing high blood pressure that she says is linked to a large uptick in pain. She has had multiple neck and back surgeries over the past few years due to damage from her AS and the car accident (and still needs to have more discs in her spine replaced).
“I’ve been extremely cautious and careful during the pandemic because we didn’t know whether I’d be more or less at risk from being on a TNF inhibitor biologic and I have plenty of health issues that are concerning,” says Kristen. “Mentally, it gets to you. I have to be so careful every single second.”
Kristen got married in October — “it was a Zoom wedding; not even our parents came.” She and her husband have been strictly quarantining outside of their jobs, which put them both at considerable COVID-19 risk. Her husband works on power lines, so he is frequently in close contact with other crew members and occasionally has to travel out of town to work in high-risk areas.
Kristen and her husband have had to quarantine from each other within their home four separate times since the pandemic began. “One of us stays in the basement and the other upstairs. Sometimes we’ll meet in the backyard for a socially distanced dinner outside.”
Deciding to Get the COVID-19 Vaccine
When Kristen first learned that she’d be eligible to get the Pfizer COVID-19 vaccine, she had mixed emotions and thoughts.
On one hand, she wanted to get it as soon as possible because of how exposed she is to the coronavirus on a daily basis.
On the other, she had a lot of questions about her medications, like the biologic Remicade she currently takes as well as the fact that she had been on the disease-modifying antirheumatic drug (DMARD) methotrexate for 15 years (she stopped it last year).
When the COVID-19 vaccine first received emergency use authorization from the U.S. Food and Drug Administration (FDA) in December, there was little information from medical authorities about immunosuppressant medications and autoimmune conditions.
Although researchers are starting to study how people on specific immunosuppressants fare after the getting the vaccine, data won’t be available for some time. Patients and their health care providers must make decisions together based on what is known about COVID-19 safety and efficacy generally and weigh that against the risks of not getting vaccinated.
Kristen did her homework as thoroughly as she could. She spoke to her rheumatologist, who was a little wishy-washy but said that “it was better for me to get the vaccine even if I might have less of a response to it.”
She also met with her hospital’s head of vaccine distribution to review all of her questions. While he couldn’t provide answers about her medications based on data from the COVID-19 vaccine specifically, he did share information about her medications and other types of vaccines, like flu.
For example, there is evidence that the DMARD medication methotrexate can decrease the effectiveness of the flu vaccine. But since Kristen hadn’t been taking methotrexate recently, it wouldn’t be an issue.
Overall, he and her rheumatologist had a similar perspective.
“Even if the vaccine turns out to be less effective in people on DMARD medication, it’s still better than nothing if you get COVID-19,” Kristen recalls him saying. “I felt extremely comfortable getting the vaccine after that conversation.”
What Immunocompromised Patients Need to Know About COVID-19 Vaccines
Because the Pfizer and Moderna vaccines are not live vaccines, there’s no reason to think they would be less safe in people on immunosuppressant medication, though they be may less effective.
People on immunosuppressant medications were not included in the clinical trials for the COVID-19 vaccine, but this is not unusual. These medications are first studied in healthy adults and then are typically studied in special populations (such as the immunocompromised, pregnant or breastfeeding women, or children) once more is generally known about safety and effectiveness.
You can read more here about getting the Pfizer vaccine or the Moderna vaccine when you’re immunocompromised.
What Getting the Vaccine Was Like
Kristen’s hospital set up a special clinic to administer the vaccine, so she was able to easily get it at work. She described a three-room flow: In the first room, you meet with a staff person who looks at your medical chart and answers any questions you have; you also fill out paperwork and do a screening for COVID-19 symptoms like fever and cough. In the second room, a nurse gives the injection. In the third room, you wait for up to 30 minutes after receiving the vaccine to monitor for allergic reactions. This room was designed for comfort and care: “We sat in recliner chairs, ‘thank-you’ snacks were available, and there was a movie playing on a big screen on the wall,” Kristen remembers.
As for actually getting the shot, “it was the easiest vaccine I’ve ever had,” Kristen says, noting that it was a much smaller needle than other vaccines or blood draws she’s received. “It was hardly noticeable and I felt completely fine afterward.”
What I Want Other People to Know About Getting the COVID-19 Vaccine
Kristen feels relieved now that she has her first dose, but she attributes a lot of her relief to the thorough process and that she was able to get her main questions addressed.
“If you’re going to get the vaccine and have some questions, find out who will be on site that can try to answer things about your personal situation and medications,” she suggests.
In online support groups, Kristen says she sees two main groups of patients: people who are eager and can’t wait to get it and others who “don’t want to be a guinea pig.” To the latter group, she encourages people to learn more about the research that went into developing the vaccines. “I know the timeline seems quick, but they’ve been researching and studying these for years.”
“Getting the vaccine was the best choice for my personal circumstances,” says Kristen, who acknowledges that the level of COVID-19 risk she is exposed to certainly influenced her decision to get it sooner than later. “But everyone will be different.”
She does admit that she feels a little safer now. “Having the vaccine has lowered my stress and anxiety tremendously, just knowing that I have a little help on board.”
Get Free Coronavirus Support for Chronic Illness Patients
Join the Global Healthy Living Foundation’s free COVID-19 Support Program for chronic illness patients and their families. We will be providing updated information, community support, and other resources tailored specifically to your health and safety. Join now.