Imagine the relief of finally having a name for years of inexplicable fatigue, dry eyes, swollen glands, and discomfort. Being told you have Sjögren’s disease can feel like a breakthrough after a long search for answers.
I should know – I went years with Sjögren’s symptoms which were masked by my rheumatoid arthritis and allergies. Now that I’m facing a Sjögren’s diagnosis, I feel relieved and hopeful in finding a treatment that works for me. Yet for some, that relief soon turns to confusion as emerging symptoms lead doctors to dig deeper.
An unexpected diagnosis of immunoglobulin G4-related disease, or IgG4-RD, reveals that what once seemed like a single ailment was only part of a more complex picture. Patients then find themselves on an emotional rollercoaster as the comfort of a familiar diagnosis gives way to the daunting challenge of understanding an entirely new condition.
Understanding IgG4-Related Disease and Sjögren’s Disease
IgG4-related disease (IgG4-RD) and Sjögren’s disease can share symptoms, making it difficult to tell them apart. This overlap can lead to misdiagnosis, delays in treatment, and confusion about these autoimmune conditions. Below, we explain their similarities, differences, and how doctors diagnose and treat each condition.
What is Sjögren’s disease?
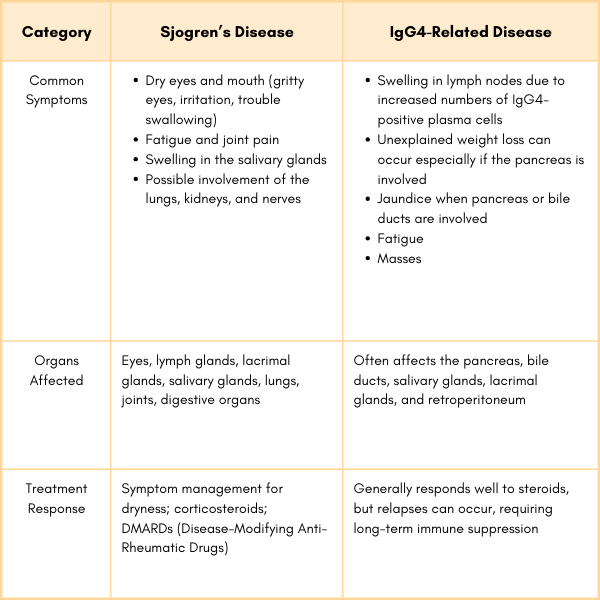
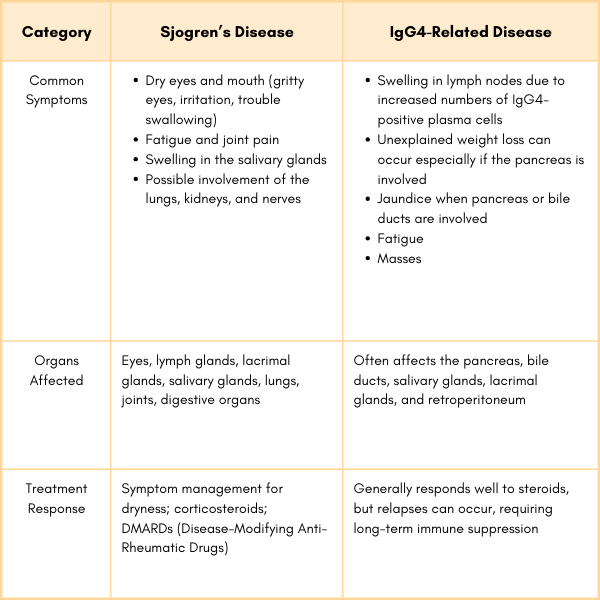
Sjögren’s disease is an autoimmune disease that mainly targets the glands that produce saliva and tears, causing dry eyes and dry mouth (sicca symptoms). Because these symptoms are also common in IgG4-RD, the two conditions are often mistaken for one another.
What is IgG4-Related Disease?
IgG4 is an antibody that helps regulate the immune system, preventing overreactions to harmless substances rather than fighting infections. IgG4-related disease (IgG4-RD) is a systemic inflammatory condition where IgG4-positive plasma cells infiltrate tissues, causing swelling, dysfunction, or fibrosis (scarring).
Why is IgG4-RD sometimes confused to be Sjögren’s disease?
Dr. Matthew C. Baker, a rheumatologist and Stanford University expert on IgG4-RD, describes the impact of IgG4-related disease, noting that it can affect multiple organs and cause significant inflammation. “The most commonly affected organs are the pancreas, the salivary glands, and the lacrimal glands,” he explains, highlighting the condition’s tendency to target glandular tissues and disrupt their function.
While Sjögren’s primarily focuses on dryness, IgG4-RD can cause symmetrical swelling of the salivary and lacrimal (tear-producing) glands, often leading to eye and mouth dryness. This condition may present as sicca symptoms or diffuse enlargement of the lacrimal and major salivary glands, known as Mikulicz disease. A misdiagnosis can occur if a doctor focuses only on dryness symptoms without looking for systemic inflammation or testing IgG4 levels.
Diagnosing IgG4-RD
Doctors use a combination of blood tests to diagnose IgG4-RD, imaging, and biopsies to confirm IgG4-RD and rule out similar diseases like Sjögren’s disease.
Blood Tests:
- Elevated IgG4 levels are a key indicator. Doctors measure total IgG and IgG4 levels.
- Low complement Levels (C3 and C4) may point to immune system involvement.
Imaging:
- Magnetic Resonance Imaging (MRI) details swelling and soft tissue changes, such as in salivary glands, pancreas, or lymph nodes.
- Computed Tomography (CT Scans) helps to identify organ enlargement, tissue thickening, or fibrosis.
Tissue Biopsy:
A tissue biopsy is the most definitive test for diagnosing IgG4-RD. It involves taking a small tissue sample from an affected organ or gland and looking for specific features:
- A dense collection of immune cells known as lymphoplasmacytic tissue inflammation
- A high number of IgG4-positive plasma cells in the tissue
- Storiform fibrosis – a unique “whorled” or layered pattern of scarring
How Does IgG4-RD Differ from Sjögren’s Disease?
While both conditions can cause swelling in the salivary and lacrimal glands, there are key differences.
- Systemic involvement: IgG4-RD affects a broader range of organs (e.g., pancreas, bile ducts, kidneys) compared to Sjögren’s disease.
- Symptoms of dryness: Dry eyes and dry mouth are hallmark features of Sjögren’s disease but are less common in IgG4-RD.
- Lab differences: Elevated IgG4 levels and plasma cells are specific to IgG4-RD, while anti-SSA (Ro) and anti-SSB (La) antibodies are markers for Sjögren’s disease.
What Questions Can You Ask Your Doctor?
If something feels off and especially if treatments are not working as intended, talk with our doctor about additional testing and changes to your treatment plan.
Could my symptoms be caused by something other than Sjögren’s, such as IgG4-related disease?
Have my imaging or blood tests shown any signs that could indicate IgG4-related disease?
Should we test my IgG4 antibody levels to help differentiate between these conditions?
Would a biopsy help confirm whether my symptoms are due to IgG4-related disease or Sjögren’s?
Should I see a rheumatologist, immunologist, or another specialist for further evaluation?
What are the next steps if my symptoms don’t improve with treatments typically used for Sjögren’s?
Why Proper Diagnosis Matters
Since symptoms and lab results for Sjögren’s disease and IgG4-RD can overlap, seeing a specialist, such as a rheumatologist, is essential for an accurate diagnosis.
If you have persistent dry eyes, dry mouth, or swelling in your glands, don’t wait – seek medical care. Correctly identifying whether you have IgG4-RD, Sjögren’s, or another condition ensures you get the right treatment and care.
Learn More About IgG4-RD
Click here to get more information on IgG4-RD including a guide to getting diagnosed, managing symptoms, and treatment options.
This article was made possible with support from Amgen.
Baker, Matthew C, MD. Personal Interview. Division of Immunology and Rheumatology Clinical Chief and Assistant Professor of Medicine, Stanford University. February 3, 2025.
Stone, J. H., et al. “IgG4-Related Disease.” New England Journal of Medicine, 2012. Doi: https://doi.org/10.1056/NEJMra1104650.
Shiboski, C. et al. Natural history and Predictors of Progression to Sjögren’s Syndrome Among Participants of the SICCA registry. Arthritis Care & Research. 2017. Doi: https://doi.org/10.1002/acr.23264.
Veenbergen, S., et al. Autoantibodies in Sjögren’s syndrome and its classification criteria. Journal of Translational Autoimmunity, 5, 100138, 2022. Doi: https://doi.org/10.1016/j.jtauto.2021.100138.





