When Alicia Meyer’s husband was diagnosed with a serious liver condition, their world turned upside down. Doctors suspected cholangiocarcinoma, a type of bile duct cancer, and told them there was only a 5% chance it was something else. With time running out, he underwent a major liver resection—a surgery that led to serious complications, including six weeks in the ICU and five days on life support.
But after enduring eight weeks in the hospital, they learned that the surgery might not have been necessary after all.
He did not have cancer. Instead, he was later diagnosed with immunoglobulin G4-related disease, or IgG4-RD, a condition that had been mistaken for primary sclerosing cholangitis (PSC) or bile duct cancer. Since starting treatment, his condition has stabilized, but the journey to a correct diagnosis was long and painful.
Alicia husband’s story is not unique. Up to one-third of patients with IgG4-related sclerosing cholangitis (IgG4-SC) undergo major, invasive surgeries – including liver transplants – because their condition is mistaken for malignancy (cancer) before they receive the correct diagnosis.
While IgG4-SC and PSC both affect the bile ducts and can appear similar on imaging tests, they require different treatments. That’s why knowing the key differences and asking the right questions can help ensure you receive the best care possible.
Understanding Sclerosing Cholangitis: PSC, IgG4-SC, and Secondary SC
Sclerosing cholangitis (SC) is a condition that causes progressive narrowing and damage to the bile ducts due to ongoing inflammation and scarring (fibrosis). This can lead to problems with bile flow, liver function, and long-term complications.
There are three main types of SC, each with different causes and treatment approaches:
- Primary Sclerosing Cholangitis (PSC)
- The cause is unknown (idiopathic), but it’s strongly linked to inflammatory bowel disease (IBD), such as ulcerative colitis.
- It mainly affects younger adults and does not respond to steroids.
- Over time, it can lead to liver damage and may require a liver transplant.
- IgG4-Related Sclerosing Cholangitis (IgG4-SC)
- A form of IgG4-related disease (IgG4-RD), an immune system condition that can affect multiple organs.
- Patients are typically older (60+ years old) and often also have autoimmune pancreatitis.
- Unlike PSC, IgG4-SC responds well to corticosteroid treatment, which can significantly improve symptoms and slow disease progression.
- Secondary Sclerosing Cholangitis (Secondary SC)
This occurs when the bile ducts are damaged by another condition, such as:
- Surgical complications (postoperative biliary strictures)
- Severe bacterial infections (bacterial cholangitis)
- Gallstones (choledocholithiasis) blocking the bile ducts
- Treatment focuses on resolving the underlying cause, such as removing blockages or treating infections.
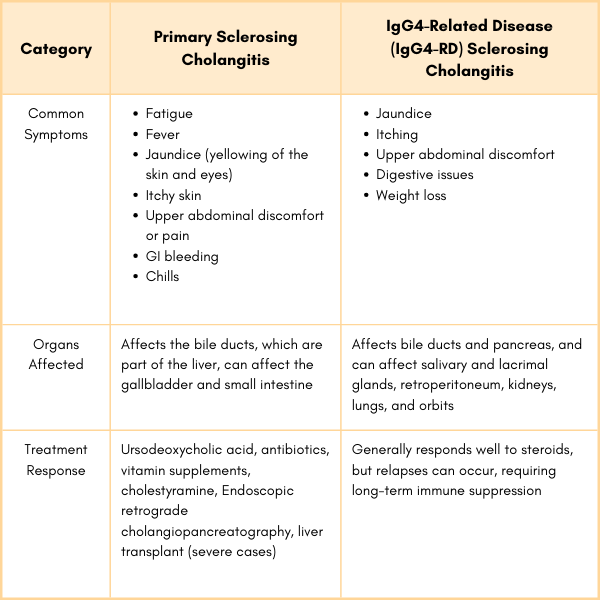
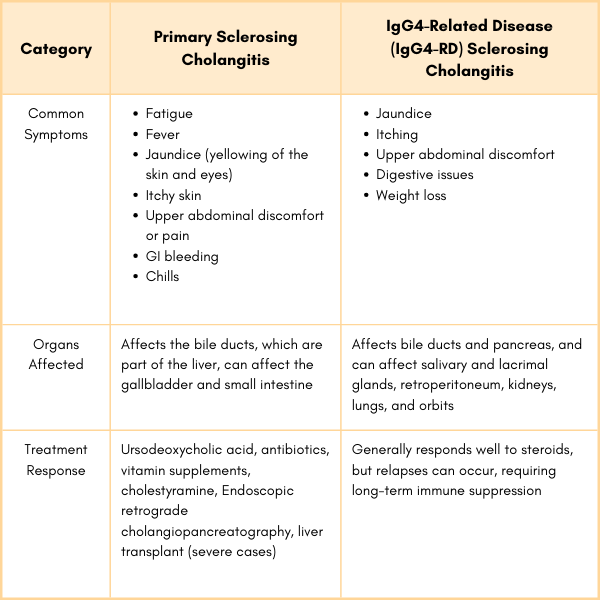
Symptoms: How PSC and IgG4-SC Compare
Many people with PSC have no symptoms at first. When symptoms do appear, they often include:
- Fatigue
- Fever
- Jaundice (yellowing of the skin and eyes)
- Itchy skin
- Upper abdominal discomfort
- GI bleeding, which may be seen in PSC patients who also have ulcerative colitis
While IgG4-SC can have overlapping symptoms, key differences can help tell the two conditions apart:
- Age at Diagnosis: PSC is usually diagnosed between 35-47 years old, while IgG4-SC typically affects people over 60.
- Response to Treatment: PSC does not respond to steroids, but IgG4-SC dramatically improves with corticosteroid treatment.
- Other Organ Involvement: IgG4-SC is often linked to autoimmune pancreatitis and inflammation in multiple organs, while PSC primarily affects the bile ducts and liver.
Dr. Daniela (Elena) Ghetie, a rheumatologist in Oregon who serves as the director of the Vasculitis Center and co-director of Myositis Center at Oregon Health and Science University, provides insight into how elevated IgG4 levels can impact the liver and pancreas, leading to visible symptoms.
“People may develop yellowish skin and sclera, so their eyes and skin can appear yellow due to the accumulation of bilirubin, a liver byproduct,” explains Dr. Ghetie. “This often occurs in individuals with autoimmune pancreatitis, particularly those with elevated IgG4 levels, which can involve their ducts that connect the pancreas and the liver.”
Dr. Ghetie continues by explaining that this involvement can lead to fibrosis and narrowing of the ducts, contributing to ineffective production and elimination of biliary enzymes.
Could Your PSC Diagnosis Be Wrong? Questions to Ask Your Doctor
If you’ve been diagnosed with PSC but your symptoms don’t fully align, ask your doctor:
Could my symptoms be caused by IgG4-SC instead of PSC?
Have my blood IgG4 levels been tested?
Would a biopsy help confirm whether I have IgG4-SC?
Should I try a short course of corticosteroids to see if my symptoms improve?
Are there any signs in my imaging scans that suggest IgG4-SC rather than PSC?
Would it be helpful to see a specialist in autoimmune liver diseases?
Advocating for the Right Diagnosis
Charlotte Pilcic knows firsthand how frightening a misdiagnosis can be. In 2023, she went to the ER with what doctors believed was pancreatic cancer after finding a 4 cm mass on her pancreas. “I thought I only had three months to live,” she recalls. After multiple biopsies and imaging scans, her diagnosis changed to autoimmune pancreatitis, but her doctors were still unsure whether she had PSC or IgG4-SC. After three months on prednisone, the mass disappeared, pointing to an IgG4-related condition.
Charlotte’s story highlights the importance of pushing for further testing when a diagnosis doesn’t seem to fit. Here’s how you can advocate for yourself:
- Track your symptoms carefully. Keep a log of what you’re experiencing, including any changes over time.
- Ask for a second opinion. If your doctor is unsure, seeing a specialist in autoimmune liver diseases may provide clarity.
- Request the proper tests. Blood tests for IgG4 levels and a biopsy of the bile ducts can be key to distinguishing between PSC and IgG4-SC.
- Know your treatment options. If you have IgG4-SC, steroids can dramatically improve symptoms, while PSC does not respond to them.
The Bottom Line
Because PSC and IgG4-SC can look alike, many patients are initially misdiagnosed. But getting the correct diagnosis is critical since the conditions require different treatments. If you or a loved one has been diagnosed with PSC but is older, has high IgG4 levels, or isn’t responding to treatment as expected, talk to your doctor about whether IgG4-SC could be the actual cause. The sooner you get the correct diagnosis, the sooner you can start the proper treatment and take control of your health.
Learn More About IgG4-RD
Click here to get more information on IgG4-RD including a guide to getting diagnosed, managing symptoms, and treatment options.
This article was made possible with support from Amgen.
Cooper J, Markovinovic A, Coward S, et al. Incidence and Prevalence of Primary Sclerosing Cholangitis: A Meta-analysis of Population-based Studies. Inflammatory Bowel Disease. 2024 Nov 4;30(11):2019-2026. doi: https://doi.org/10.1093/ibd/izad276.
Gidwaney N G, Pawa, S, and Das KM. Pathogenesis and clinical spectrum of primary sclerosing cholangitis. World Journal of Gastroenterology. 2017. https://doi.org/10.3748/wjg.v23.i14.2459
Interview, Ghetie, D. Director of the Vasculitis Center and Co-Director of Myositis Center, Oregon Health and Science University. https://www.ohsu.edu/people/daniela-ghetie-md.
Interview, Charlotte Pilcic.
Interview, Alicia Meyer.
Tanaka A. IgG4-Related Sclerosing Cholangitis and Primary Sclerosing Cholangitis. Gut Liver. 2019 May 15. doi: https://doi.org/10.5009/gnl18085.





