*Please note: Certain individuals’ names have been altered to maintain confidentiality.
Jon Baldry’s journey to a correct diagnosis was anything but straightforward. In 2018, he was hospitalized with jaundice caused by gallstones, but what followed was even more unsettling. Doctors suspected pancreatic or duodenal cancer, with a strong likelihood of pancreatic cancer. As a result, Jon underwent a pancreaticoduodenectomy — known as a Whipple procedure — an intensive operation that removes part of the pancreas, stomach, and other organs, a 10-hour surgery.
Only after the surgery, when doctors evaluated the removed tissue, they realized it was not cancer after all. A blood test confirmed elevated IgG4 levels, finally providing answers that were overlooked during the initial workup. “It was a huge relief to learn I didn’t have cancer, but the uncertainty remained,” Jon recalls.
Jon’s experience isn’t unique. Charlotte’s world turned upside down when she went to the ER and was told she had a 4 cm mass on her pancreas that doctors believed was cancer.
“I thought I only had three months to live when the mass was found. I was scared and thought I’d better prepare,” recalls Charlotte Pilcic.
Terrified, she began bracing for the worst. However, after undergoing three biopsies, all of which came back negative for cancer, further testing revealed strictures in her pancreas. In the end, the mass wasn’t cancer at all — it was autoimmune pancreatitis. Charlotte’s experience highlights how IgG4-RD can mimic conditions like pancreatic cancer, making an accurate diagnosis crucial.
For Peter (name changed to protect identity), just before surgery, a pathologist questioned his diagnosis. Further testing uncovered autoimmune pancreatitis, not cancer.
If you’ve been told you have pancreatitis, but your treatments aren’t working, the underlying issue might be something rare and often misunderstood: IgG4-related pancreatitis, also known as Type 1 autoimmune pancreatitis.
This condition is often characterized by high levels of immunoglobulin G4 (IgG4) antibodies, leading to inflammation in the pancreas. It’s easy to confuse with chronic pancreatitis or even pancreatic cancer, which can delay the correct treatment.
What Is Pancreatitis?
Pancreatitis is inflammation of the pancreas, a gland behind the stomach that helps digest food and regulate blood sugar. This inflammation occurs when digestive enzymes, which usually break down food in the small intestine, start attacking the pancreas.
Pancreatitis can be acute (sudden and temporary) or chronic (ongoing and progressive). Acute pancreatitis often resolves with treatment, but severe cases may require hospitalization. Chronic pancreatitis causes long-term damage, leading to complications over time.
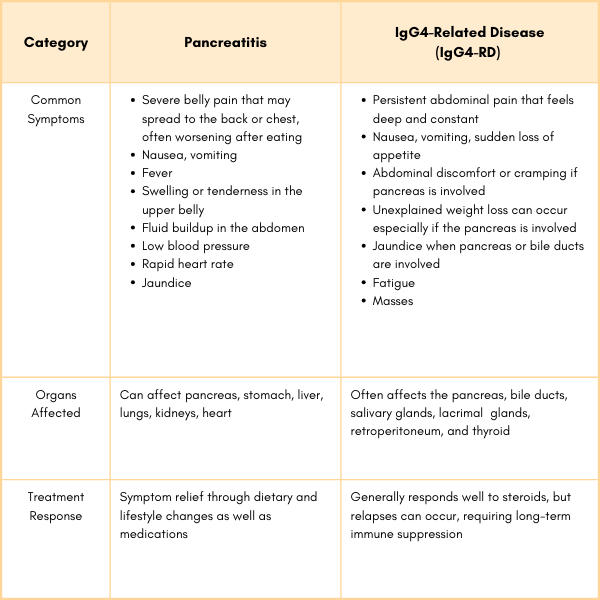
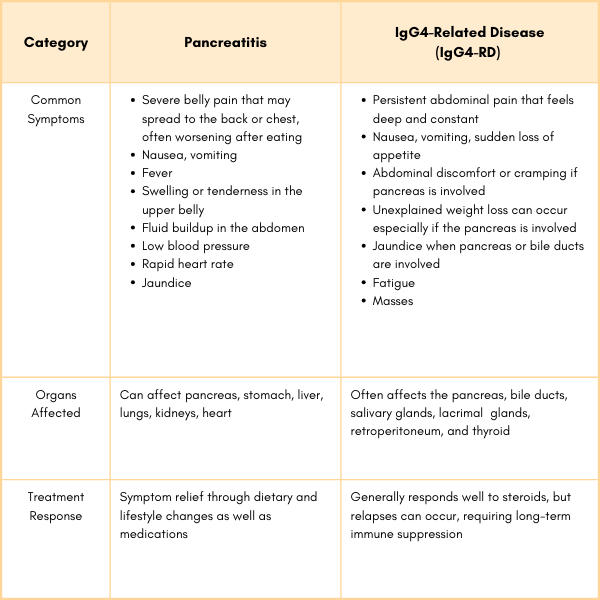
Symptoms of Pancreatitis:
- Severe belly pain that may spread to the back or chest, often worsening after eating
- Nausea and vomiting
- Fever and rapid heart rate
- Swelling or tenderness in the upper belly
- Fluid buildup in the abdomen
- Low blood pressure
- Yellowing of the skin and eyes (jaundice)
Because pancreatitis shares symptoms with other conditions, including pancreatic cancer and immune diseases like IgG4-related disease, getting an accurate diagnosis is essential for proper treatment. Keeping track of your symptoms through a diary or an app like PatientSpot will help you communicate with your doctor as you describe how you feel.
What Does IgG4-Related Autoimmune Pancreatitis Feel Like?
Patients often describe symptoms that resemble classic pancreatitis but with some surprising differences. Common symptoms include:
- Persistent abdominal pain that feels deep and constant.
- Jaundice (yellowing of the skin or eyes), often mistaken for liver issues.
- Nausea, vomiting, or a sudden loss of appetite.
- Unexplained weight loss that can feel alarming.
- Fatigue that won’t go away, no matter how much rest you get.
Why Is IgG4-Related Autoimmune Pancreatitis Often Misdiagnosed?
IgG4-related pancreatitis is rare, and its symptoms mimic other conditions, like chronic pancreatitis or even pancreatic cancer.
- Imaging scans can show masses or swelling, which are often mistaken for cancer.
- It’s not triggered by common causes of pancreatitis, like alcohol use or gallstones.
- Many doctors aren’t familiar with autoimmune-related pancreatitis.
A Doctor’s Perspective
Despite growing awareness of IgG4- RD, it is still often mistaken for other conditions, sometimes leading to unnecessary and invasive treatments. “Even just jumping back five to 10 years, it was really common for patients to be initially diagnosed with cancer,” says Dr. Matthew C. Baker, a rheumatologist and IgG4-RD expert at Stanford University.
One striking example involves patients with a pancreatic mass. Instead of considering IgG4-RD or other possible causes, some patients have undergone major surgeries like the Whipple procedure. “And then they would find on pathology that there was no cancer,” Dr. Baker explains. “At that time, many people probably didn’t know what it was, but it just wasn’t cancer.”
Fortunately, awareness has improved. Dr. Baker recalls a recent case in which a patient was told they had cancer and was scheduled for surgery. Seeking a second opinion, they were correctly diagnosed with IgG4-RD and avoided an unnecessary procedure. “It’s completely in remission with therapy,” he says.
These stories highlight why recognizing IgG4-RD early is critical—so patients receive the correct diagnosis and treatment without undergoing unnecessary surgeries or cancer treatments.
How to Get the Right Diagnosis
If standard pancreatitis treatments aren’t helping or something feels “off,” it’s time to dig deeper.
Steps in the Diagnostic Process:
- Blood Tests: Many individuals with IgG4-RD have elevated levels of an antibody called IgG4 in their blood.
- Imaging Studies: CT or MRI scans to identify inflammation patterns or suspicious masses.
- Biopsy: In some cases, a tissue sample is taken to confirm the diagnosis and rule out cancer.
Questions to Ask Your Doctor
Your voice is essential in your health care journey. Here are some key questions to bring to your appointment:
Could my symptoms be related to autoimmune pancreatitis, like IgG4-related pancreatitis?
Have my imaging or blood tests shown anything that might suggest this condition?
Can we test my IgG4 antibody levels?
Should we consider a biopsy to confirm or rule out other conditions?
What are the next steps if my symptoms don’t improve with standard treatments?
Partnering with Your Doctor to Get Answers
Diagnosing IgG4-related pancreatitis can be challenging, but you can play an active role in the process.
- Be Persistent: Don’t hesitate to ask for more testing or second opinions if treatments aren’t helping.
- Document Your Symptoms: Write down when they occur, how severe they are, and what might trigger them.
- Seek a Specialist: Consider seeing a gastroenterologist or autoimmune disease expert familiar with this condition.
You Are Your Best Advocate!
If your pancreatitis diagnosis doesn’t feel right, or if treatments aren’t working, IgG4-related pancreatitis could be the missing piece. Asking the right questions and working with your doctor can help uncover the real cause of your symptoms. Quicker relief is possible with the proper diagnosis and treatment.
Learn More About IgG4-RD
Click here to get more information on IgG4-RD including a guide to getting diagnosed, managing symptoms, and treatment options.
This article was made possible with support from Amgen.
Baenas DF, Miretti V, et al. Differential Diagnosis Between Pancreatic Involvement in Igg4-Related Disease and Pancreatic Cancer. Gastroenterología y Hepatología (English Edition). February 2021. doi: https://doi.org/10.1016/j.gastre.2020.05.017
Interview with patient Jon Baldry.
Interview with patient Charlotte Pilcic.
Interview with patient Peter.*
Interview with Matthew C. Baker, MD, a rheumatologist and IgG4-RD expert at Stanford University.
Pittman T. GI Specialists Seeing More Cases Involving IgG4-Related Disease. Duke Health. March 12, 2019. https://physicians.dukehealth.org/articles/gi-specialists-seeing-more-cases-involving-igg4-related-disease.
Wang N, Zhu P, et al. IgG4-related autoimmune pancreatitis and sclerosing cholangitis: A case report and literature review. Medicine (Baltimore). 2024 Apr 26;103(17):e37922. doi: https://doi.org/10.1097/MD.0000000000037922.





