Rates of gonorrhea, a bacterial sexually transmitted infection, are rising dramatically in the United States. They increased by 18.6 percent from 2016 to 2017, according to the Centers for Disease Control and Prevention.
While you might think of the sexually transmitted infection as causing symptoms like painful urination or vaginal/penile discharge, gonorrhea can also spread beyond the genitals, rectum, and throat. In some cases, the Neisseria gonorrhoeae bacteria can travel throughout the body in what’s known as disseminated gonococcal infection (DGI). One of the main areas the bacteria like to settle in is the joints, which results in a condition known as gonococcal arthritis.
Gonococcal arthritis is a type of septic arthritis, which means that the joint symptoms are caused by an infection in the joint.
Symptoms of Gonococcal Arthritis
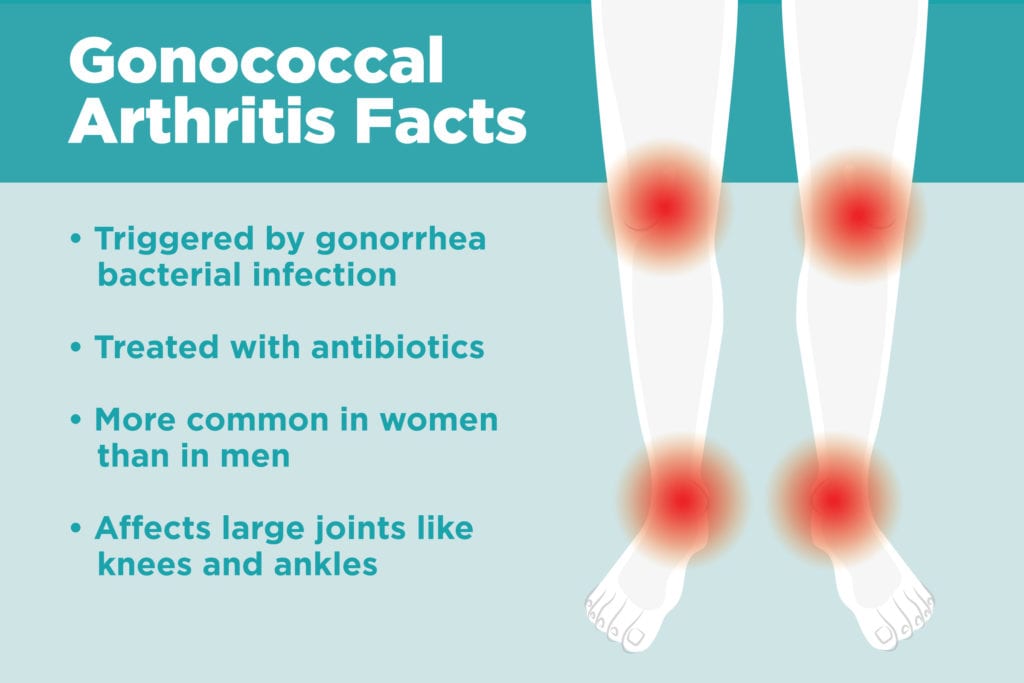
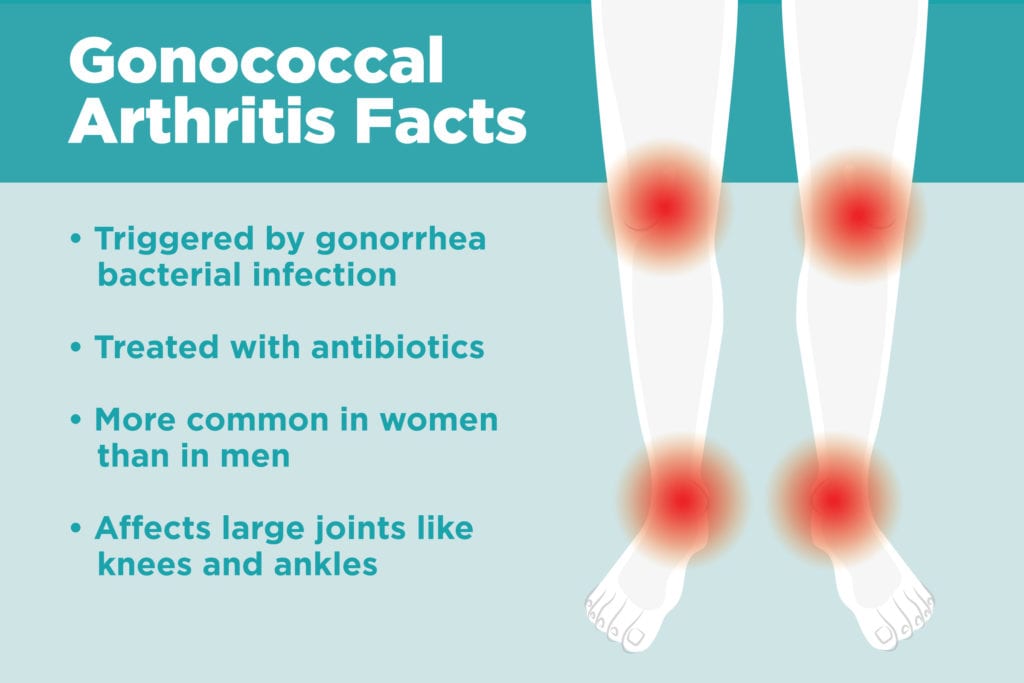
Someone with gonococcal arthritis might experience gonorrhea symptoms, such as pain when urinating or noticing discharge, but most women and about half of men will never experience those genital symptoms. They might not realize they have an STI until the DGI symptoms appear. Gonococcal arthritis normally affects one to four joints — most commonly large joints like the knees, wrists, or ankles, says Jeanne Marrazzo, MD, director of the infectious diseases division of University of Alabama at Birmingham School of Medicine.
Pustules on the palms are another telltale sign of gonococcal arthritis, adds Chris Morris, MD, a rheumatologist with Arthritis Associates in Kingsport, Tennessee. Gonococcal arthritis could also be accompanied by fever, rash, or painful, inflamed tendons in the wrist.
Causes of Gonococcal Arthritis
Gonococcal arthritis starts when Neisseria gonorrhoeae are passed through vaginal, anal, or oral sex. In about 0.5 to 3 percent of those cases, the bacteria spread beyond the initial infection site through the blood and infect other areas of the body. “[The bacteria] like to focus on the joint, where they gets in there and grow,” says Dr. Morris.
Some people are more at risk for disseminated infection than others.
For instance, HIV and certain arthritis medications can suppress the immune system, leaving patients more at risk for the bacteria to spread from the initial infection site, says Dr. Morris.
Women are also more likely to develop gonococcal arthritis than men, and not just because of their initial risk for gonorrhea. “For men, the only place [bacteria] can go is in the testes,” says Dr. Marrazzo. “But women have an entire upper reproductive tract to start establishing an infection up there.”
Gonococcal Arthritis vs. Nongonococcal Septic Arthritis
Gonococcal arthritis shares some similarities with nongonococcal septic arthritis. Both normally affect few joints, often the knees or ankles.
Here are a couple of key differences:
- Although both can be seen at any age, gonococcal arthritis is most common in people under age 40, while older people are at a higher risk for other types of septic arthritis, like those caused by staphylococci, streptococci, or fungal or viral infections.
- Inflammation of the sheath around a tendon (tenosynovitis) shows up in gonococcal arthritis but not other types of septic arthritis, and fever would also be rare in nongonococcal septic arthritis.
How Gonococcal Arthritis Is Diagnosed
“It’s always a good idea when you see people with musculoskeletal complaints … to take a sexual history,” says Dr. Marrazzo. “Especially in young people, but we don’t want to assume older people aren’t also at risk.”
To diagnose gonococcal arthritis, doctors will search for signs of gonorrhea through various tests. They could take joint fluid or urine samples, or swabs from the throat, vagina, or penis. In those samples, doctors will use a culture test or a Gram stain, both of which can show evidence of the bacteria.
Anyone who’s been diagnosed with gonorrhea or gonococcal arthritis should let their sexual partners know so that they can be tested for gonorrhea too.
How Gonococcal Arthritis Is Treated
Treatment for gonococcal arthritis is the same as for the sexually transmitted infection gonorrhea: antibiotics. The CDC recommends taking ceftriaxone intramuscularly or through IV once a day, plus an oral dose of azithromycin. “Usually it’s really, really responsive,” says Dr. Marrazzo. “People will feel better within 24 hours.”





