If you’re one of the roughly 780,000 Americans with Crohn’s disease, an inflammatory bowel disease (IBD) that causes damage along the length of the gastrointestinal tract, you’ve probably heard a lot of mixed messages about how diet may or may not help manage your disease.
One way of eating called the low-residue diet comes up a lot in conversations about Crohn’s disease. Here’s what you need to know about Crohn’s and the low-residue diet.
How Food Can Help with Crohn’s Disease
Crohn’s disease can cause damage and inflammation in any part of the GI tract — from the mouth all the way to the anus. Most often, it affects the end of the small intestine, called the ileum. “Symptoms vary based on the location of inflammation, but often include abdominal pain, diarrhea, and weight loss,” says Colleen D. Webb, MS, RDN, CLT, a New York-based clinical nutritionist who specializes in gastrointestinal health.
While food doesn’t cause Crohn’s disease — which is an inflammatory disease that is thought to occur as a result of genetic and environmental factors — what you eat can exacerbate symptoms. Dietary triggers of Crohn’s, however, can depend very much on the individual.
As a result, dietary recommendations for Crohn’s disease can vary widely. Often, doctors suggest a “low-residue” or low-fiber diet during an active flare to help minimize gut distress. Doctors may also suggest a low-fiber or low-residue diet for a patient who has strictures, or narrowing in the intestines.
While these terms are technically different, doctors often use them interchangeably.
Crohn’s Disease Diet: Fiber vs. Residue
Fiber is an umbrella word for types of carbohydrates that the body cannot digest. Different types of fiber impact your digestion in different ways. Soluble fiber (found in foods like beans and oats) absorbs water and slows down the speed at which your body digests food. Insoluble fiber (found in foods like bran, leafy green vegetables, and nuts) adds bulk to the stool. It works like a broom, helping food to pass more quickly through the digestive tract. This type of fiber in particular can be irritating to people with IBD, particularly when they’re in the midst of a flare. Cooking, peeling, and removing the seeds from foods that are high in insoluble fiber can help make them more easily digestible.
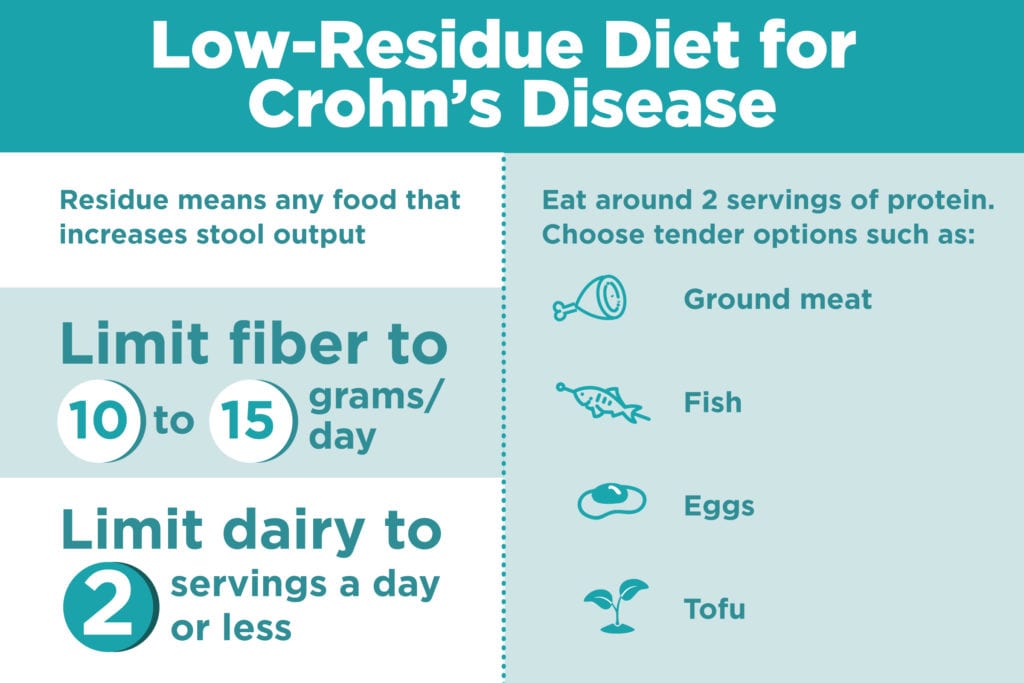
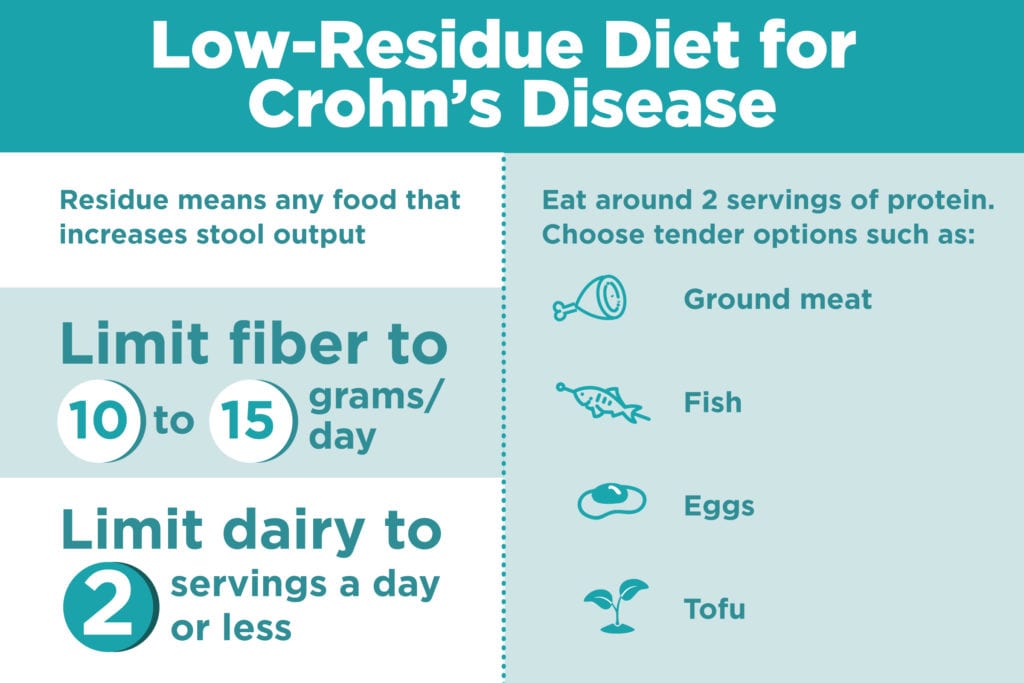
Residue refers to any food that increases stool output, which includes high-fiber foods, but extends to meat and dairy as well. A low-residue diet, therefore, limits high-fiber foods like berries, leafy green vegetables, beans, and whole grains, as well as meat and dairy.
What Do You Eat on a Low-Fiber or Low-Residue Diet?
A low-fiber diet keeps fiber intake to no more than 10 to 15 grams of fiber per day. To achieve this, a person would avoid whole-grain foods like cereal and whole-wheat bread in favor of white rice, white flour pasta, and white bread. Lower-fiber fruits and vegetables like white or sweet potato, zucchini, and melon are permitted in moderate amounts.
A low-residue diet takes the low-fiber diet and adds more restrictions. Milk and milk products should be limited to no more than two cups per day. It suggests around two servings of protein per day, but choose tender or ground meats like ground turkey, fish, eggs, and tofu for your proteins in place of foods like tough meat with gristle and beans.
Here’s a sample day of a low-residue diet:
Breakfast
- 1 slice sourdough bread
- 2 eggs, scrambled
Lunch
- Chicken noodle soup
- 1 small roll
- ½ cup cantaloupe
Afternoon snack
- 1 small ripe banana
- 1 tablespoon smooth peanut butter
Dinner
- Tofu stir fried with zucchini
- White rice
Do Low-Fiber and Low-Residue Diets for Crohn’s Disease Work?
There has been limited research on both low-fiber and low-residue diets in people with Crohn’s disease. However, current research doesn’t find much difference between following those restrictive diets and more liberal ones.
In fact, people with Crohn’s in remission who avoid fiber may be doing themselves a disservice. Adults with Crohn’s disease who did not avoid high-fiber foods were around 40 percent less likely to have a flare than those who did avoid high-fiber foods over a six-month period, according to a 2016 study from George Mason University.
Interestingly, fiber intake has no relationship with whether or not a person develops Crohn’s disease in the first place, according to a large multi-center study from Europe published in 2018 that followed more than 400,000 people.
As for during a flare, there hasn’t been much research on whether or not low-fiber or low-residue diets really help. It’s important to remember that medication is the first line of defense. Of course, it makes sense to eat foods that are less irritating to the gut when a person is experiencing an active Crohn’s disease flare, and many people do find that restricting their eating is helpful.
It’s depends on what you feel works for you personally. If you find that a low-fiber or low-residue diet helps you feel better, then it’s worth sticking with until your flare has subsided. Keeping a food and symptom journal can help you tailor your diet to what works for you.
What to Eat During Crohn’s Flares: Low-Roughage Diet
What may be more beneficial than a low-residue or low-fiber diet if you’re in an active Crohn’s flare is a low-roughage diet, says Webb. It’s got a lot in common with a low-fiber or low-residue diet, with some caveats.
“I prefer the term ‘roughage’ to fiber because one need not avoid all fiber,” says Webb. The soluble fiber found in foods like cooked apples, ground chia seeds, and oatmeal in particular may help people with Crohn’s by absorbing fluid and slowing down digestion.
A person on a low-roughage diet would avoid potentially bowel-aggravating foods like whole seeds, nuts, and popcorn, but would eat well-processed fiber-containing foods like smoothies, soups, well-cooked vegetables, and creamy nut butters, says Webb. “They produce very little residue,” she says.
Whatever diet your doctor suggests for short-term relief from a Crohn’s flare, consider looking into following up with a registered dietitian who specializes in irritable bowel disease. She will be more likely to have the time and expertise to help you go beyond fiber and roughage to identify any specific food triggers that affect you and help manage your disease over the long term.





