All autoimmune diseases have this in common: Your immune system mistakenly begins to attack your body, causing widespread inflammation, swelling, pain, and, over time, damage to your tissues and organs. Lupus is no different.
Lupus can affect many different parts of the body, which is why people with the disease can display a wide range of symptoms, depending on which organ or tissues are involved. They can also develop different symptoms as their disease progresses, or see symptoms come and go. This can make awareness of the disease tricky and complicate patients being able to get a timely diagnosis.
Like many autoimmune conditions, the initial symptoms of lupus can be pretty non-specific, says Michelle Petri, MD, a rheumatologist and director of the Lupus Center at Johns Hopkins Medicine in Baltimore, MD. “Some of the things that bother people with lupus can happen to almost anyone: some hair loss, some fever, some fatigue, some anemia.” Most people have these symptoms for about a year before their doctors get suspicious enough to check for lupus, she adds.
Read more here about common symptoms of lupus.
So what would make a provider suspicious? First off, your sex: A typical lupus patient is a woman, most often between the ages of 15 and 44, and often a woman of color (Black or Latina, to name two groups who have higher rates of the disease).
A doctor would also be on the lookout for more characteristic signs of the disease, like swollen joints or a rash that gets worse in the sun, before ordering tests to check for auto-antibodies, says Dr. Petri.
The trouble is even those characteristic signs can be common in other conditions too.
The Consequences of Misdiagnosing Lupus (or Getting a Delayed Diagnosis)
Lupus is considered a systemic disease because it can affect just about every organ in your body, from your skin to your heart to your GI tract. If the inflammation goes unchecked for a long time because you were misdiagnosed or not treated at all, you could experience organ damage and serious complications as a result.
“We find that patients develop organ injury from their lupus over time, especially if they’re not treated and their lupus is not controlled,” says Ashira Blazer, MD, a rheumatologist and assistant professor in the department of medicine at NYU Langone Health in New York City.
This is especially true when your kidneys are involved, Dr. Blazer notes. “We have to make sure that we catch that diagnosis, especially in patients who are likely to get kidney disease, because the ones that we can treat and control early are the ones who tend to survive. People with well-controlled lupus can have normal life expectancies. That is very different for people who don’t have well-controlled lupus, especially if they have internal organ involvement,” she adds.
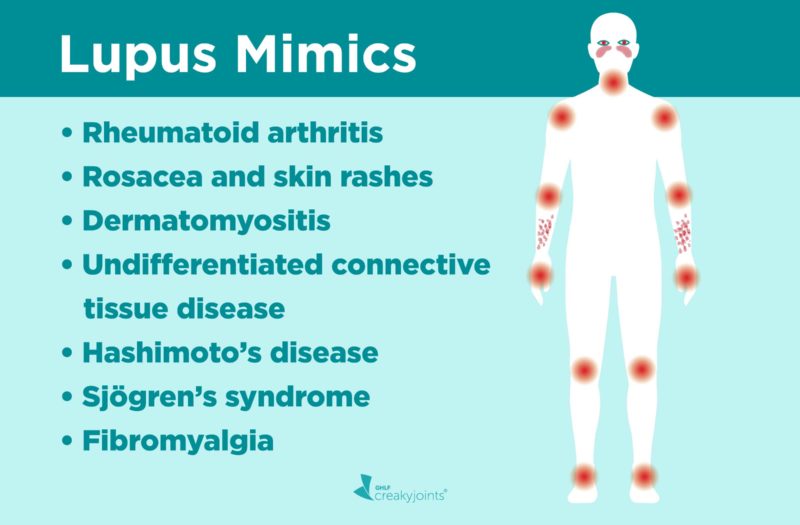
A misdiagnosis may signal something else too. “Patients who have milder symptoms, especially in this country, are the ones who are more likely to have their lupus misdiagnosed,” Dr. Blazer notes. Here are the conditions that are most likely to mimic the symptoms of lupus and how to make sure you get the right diagnosis.
Rheumatoid arthritis
This autoimmune disorder is another systemic disease, which means the inflammation not only damages joints but can cause increase the risk of heart disease and cause scarring in the lungs. Some symptoms of RA are similar to those of lupus, including fatigue, fever, rashes, and dry eyes.
“Rheumatoid arthritis and lupus affect the same distribution of joints, the small joints in the hands and wrists, for example,” says Dr. Petri. Both conditions tend to affect the joints symmetrically too. This means that if the joints in your right hand are swollen and painful, the joints in your left hand will be too.
“When someone first presents with swollen, inflamed hand joints, it might not be possible for the clinician to say exactly what the cause is just based on the physical exam,” Dr. Petri explains.
Because these diseases cannot be diagnosed based on symptoms alone, a rheumatologist will probably order blood tests to check for various autoantibodies, which are markers in your blood that your immune system makes when it is attacking itself.
“Lupus causes certain autoantibodies, and rheumatoid arthritis causes other autoantibodies,” Dr. Petri explains. One of the most common autoantibody in lupus is the antinuclear antibody (ANA), but that’s not always a sure sign of lupus. (Most people with lupus test positive for ANA, but you can have a positive ANA and not have lupus.)
Other lupus-specific autoantibodies include anti-dsDNA, anti-SSA/RO, anti-Smith, and antiphospholipid antibodies. Patients with RA tend to have rheumatoid factor or anti-CCP antibodies. (However, roughly 20 to 30 percent of RA patients do not test positive for those antibodies and are considered to have seronegative rheumatoid arthritis.)
Imaging tests such as X-rays or MRIs can look for joint damage, which is also different between lupus and RA. Usually, people with lupus don’t have deformities caused by bone erosion (although a small percentage do). Instead, their fingers may get deformed because their tendons and ligaments have loosened and lengthened.
Read more about here about differences between rheumatoid arthritis and lupus.
While some treatments for RA and lupus are the same (NSAIDs, steroids, and the disease-modifying medication hydroxychloroquine), there are big differences in the ways these diseases are treated and the damage they can do to certain organs (such as the kidneys, in the case of lupus), so getting the right diagnosis and treatment is key.
Rosacea and other skin rashes
One of the characteristic signs of lupus is a skin rash. The most common is the butterfly or malar rash that affects the cheekbones and the bridge of the nose, and the jawline. This is a red, flat rash that looks like a sunburn.
There are two other types of rashes that occur with lupus: a discoid rash, which produces round lesions that are red and scaly and often appear on the face and scalp, and another red, scaly rash known as subacute cutaneous lupus that can appear on the arms, shoulders, back, and neck — or the parts of your body that are exposed to UV rays.
For many lupus patients, these rashes get worse in the sun. “Lupus patients are particularly susceptible to ultraviolet light, not only the causing lupus rash, but affecting them internally and causing systemic flares,” says Dr. Petri. “I tell my patients that just walking from the garage into the Hopkins outpatient center is enough ultraviolet light exposure to cause them to have a rash. They need to have a hat on just for that limited exposure.”
But there are other rashes — unrelated to lupus — that can happen after sun exposure. One is called solar urticaria, which are itchy bumps that can appear in even non-exposed areas of your body. Rosacea, which can also be triggered by sunlight, often looks like a lupus rash because it tends to be red and flat and have a butterfly pattern.
Most rheumatologists and dermatologists can distinguish these rashes from a lupus rash, but if they’re not sure, they can do a skin biopsy. That will tell them if the rash is caused by lupus, another autoimmune disorder such as dermatomyositis, or something else.
Dermatomyositis
Like lupus, dermatomyositis is an autoimmune disorder that tends to affect women, (especially Black women) more than men. Most of the time, they are between the ages of 30 and 60.
The similarities don’t end there. People with dermatomyositis have a dark red or purple rash that typically appears on the back and shoulders as well as the face, especially the cheeks. Patients can also experience flares after they’ve been out in the sun, and experience fatigue and pain. Plus, when doctors do a skin biopsy, the two conditions can often look the same.
Dermatomyositis, which is a rarer condition than lupus, also causes muscle weakness, so a rheumatologist will do a physical exam to test your muscles, especially those closest to your torso, like the ones in your neck, shoulders, hips, and back. A blood test can check for particular autoantibodies that are found in people with dermatomyositis and other forms of myositis — there are about 15 specific ones. People with dermatomyositis will also have elevated levels of muscle enzyme called creatine kinase (CK).
Undifferentiated Connective Tissue Disease
“There are people who have a milder form of an autoimmune disease who just don’t meet the classification criteria for lupus. We call that undifferentiated connective tissue disease (UCTD),” says Dr. Petri.
In other words, they have some features of an autoimmune disease but they don’t have all the characteristics of lupus or RA, Dr. Blazer explains. They may test positive for antinuclear antibodies (ANAs). They also have symptoms that can look like lupus, including hair loss, rashes, and achy or swollen, red joints. They may have anemia. But they don’t typically go on to develop problems with their kidneys, liver, or other organs.
“Some rheumatologists believe that these patients have early-stage lupus, and some believe that it is its own condition that never turns into lupus,” says Dr. Blazer.
About 10 percent of people with UCTD will develop lupus. Patients diagnosed with UCTD should continue to see a rheumatologist, says Dr. Petri. That way, the doctor can keep tabs on your symptoms and continue to do lab tests to check to see if there is any organ damage.
Since UCTD usually produces mild symptoms, doctors usually recommend NSAIDs or pain relievers for joint pain and topical steroid creams. For rashes and other skin disorders, a doctor may prescribe hydroxychloroquine, an antimalarial medication that goes by the brand name Plaquenil.
Hashimoto’s disease
The thyroid is a gland in the neck that produces hormones that regulate your metabolism. When you have Hashimoto’s thyroiditis, your immune system attacks the thyroid gland and prevents it from producing enough hormones, which can slow down your metabolism and make you feel sluggish.
“Patients who have autoimmune thyroid disease might have a positive ANA, they can feel achy, and feel like they have some arthritis. They can feel very tired, they can lose weight, and that can look a lot like lupus as well,” says Dr. Blazer.
To rule out thyroid disease, your provider will give you a blood test to check the levels of your thyroid stimulating hormones (TSH) and other thyroid hormones as well as antibodies to Hashimoto’s (known as TPO antibodies). The doctor may also do a radioactive iodine uptake test (the thyroid needs iodine to make hormones). You’ll swallow liquid or a capsule with radioactive iodine, then a scanner measures how much of the radioactive iodine your thyroid absorbed. If the levels are low, that is a sign of Hashimoto’s or hypothyroidism.
About 6 percent of people with lupus can also have an underactive thyroid, according to the Johns Hopkins Lupus Center. Treatment for hypothyroidism is the same for all patients — you’ll need to take a tablet of the synthetic thyroid hormone known as levothyroxine every day.
Read more here about the connection between hypothyroidism and arthritis.
Sjögren’s syndrome
“This is a syndrome where you develop antibodies or immune activity against the moisture-producing glands in the body — the salivary glands and the tear ducts,” Dr. Blazer explains. Sjögren’s symptoms include dry eyes, dry mouth, and even dryness in the vagina. Most people with Sjögren’s are women, typically over age 40.
The condition can also damage other organs, like the kidneys, though the damage is different than the kind you get with lupus, Dr. Blazer adds. There are some other, less common signs Sjögren’s, including skin rashes, fatigue, and achy, tender joints.
While you can have Sjögren’s syndrome on its own, people with lupus and RA can also develop secondary Sjögren’s, which can further complicate diagnosis. To test for Sjögren’s, a doctor performs what’s known as the Schirmer test. A litmus paper is placed under your lower eyelid to measure tear production. Doctors may also test how much saliva you produce by injecting your saliva glands with dye and using a special X-ray to measure the flow into your mouth.
To treat Sjögren’s and prevent eye damage and inflammation, doctors can prescribe eye drops and medications to increase saliva production to prevent dry mouth symptoms. To stop inflammation, doctors may also recommend you take disease-modifying drugs such as hydroxychloroquine or methotrexate.
Fibromyalgia
“Fibromyalgia is a chronic widespread pain condition. It happens usually when the pain processing centers in the brain and the nervous system become hyperactive,” Dr. Blazer notes. Some of the symptoms of fibro mimic those of lupus — there can be fatigue and memory issues (often called fibro fog), as well as joint and muscle pain.
Similarly to lupus, fibro affects women more than men. It is not thought to be an inflammatory or autoimmune disorder like lupus is, though people with fibro might have a positive ANA test. And you can develop secondary fibromyalgia if you have lupus (or another autoimmune disorder like RA).
To check for fibromyalgia, either by itself or with lupus, a rheumatologist may use something called the tender points criteria, which involves your provider pressing specific points along your body from your head to your knees as you rate the pain. While you don’t have to meet the tender points criteria to get a definitive fibro diagnosis — and in fact, many doctors now diagnose fibro based on other criteria — it can help a rheumatologist see how widespread the pain is and how high you rate the discomfort. They will also ask you to describe your symptoms, including stiffness in your joints.
Read more here about the difference between fibromyalgia and lupus.
Treating fibromyalgia often involves many different approaches, including a mix of medications and lifestyle-oriented treatments. Here is more information about treatment options for fibromyalgia.
Making a Lupus Diagnosis
There are three sets of criteria that doctors can follow when trying to pinpoint lupus that were developed by the American College of Rheumatology and other professional groups. Though they vary slightly, overall the criteria include physical symptoms that the doctor observes (or the patient describes) as well as the presence of antibodies and auto-antibodies.
Besides taking a thorough medical history and physical exam, doctors will run certain tests to see whether lupus could be the reason for your symptoms. “Is there a rash that can be biopsied? Do patients have a positive ANA? Are there subsets of the ANA that are more specific for lupus?”
Doctors may do a urine test to check for protein, a sign that lupus may be affecting your kidneys. If the test comes back positive, doctors will then biopsy the kidneys to get more information. “If someone has chest pain [which can occur in lupus due to inflammation around the heart] we can get an X-Ray to try to see if there is fluid around the heart or evidence that there has been fluid around the heart,” says Dr. Blazer. “Especially in gray-area cases, we try to support our diagnosis as much as possible with the objective data.”
Read more here about how lupus is diagnosed.
Track Your Lupus Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Learn more and sign up here.
Keep Reading
Clinical manifestations and diagnosis of systemic lupus erythematosus in adults. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-systemic-lupus-erythematosus-in-adults.
Dermatomyositis. Medscape. https://emedicine.medscape.com/article/332783-overview.
Diagnosing Systemic Lupus Erythematosus. NYU Langone Health. https://nyulangone.org/conditions/systemic-lupus-erythematosus-in-adults/diagnosis.
Hashimoto’s disease. Office on Women’s Health. U.S. Department of Health and Human Services. https://www.womenshealth.gov/a-z-topics/hashimotos-disease.
How Lupus Affects the Skin. Lupus Foundation of America. https://www.lupus.org/resources/how-lupus-affects-the-skin
Interview with Ashira Blazer, MD, a rheumatologist and assistant professor in the department of medicine at NYU Langone Health in New York City
Interview with Michelle Petri, MD, a rheumatologist and director of the Lupus Center at Johns Hopkins Medicine in Baltimore, Maryland
Lupus. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Lupus.
Lupus. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/lupus/diagnosis-treatment/drc-20365790.
Lupus and Fibromyalgia. Hospital for Special Surgery. https://www.hss.edu/conditions_Lupus-and-Fibromyalgia.asp.
Lupus Signs, Symptoms, and Co-Occurring Conditions. Johns Hopkins Lupus Center. https://www.hopkinslupus.org/lupus-info/lupus-signs-symptoms-comorbidities.
Lupus-Specific Skin Disease and Skin Problems. Johns Hopkins Lupus Center. https://www.hopkinslupus.org/lupus-info/lupus-affects-body/skin-lupus.
Overview of the management and prognosis of systemic lupus erythematosus in adults. UpToDate. https://www.uptodate.com/contents/overview-of-the-management-and-prognosis-of-systemic-lupus-erythematosus-in-adults.
Patient education: Systemic lupus erythematosus (SLE) (Beyond the Basics). UpToDate. https://www.uptodate.com/contents/systemic-lupus-erythematosus-beyond-the-basics.
Rheumatoid Arthritis. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Rheumatoid-Arthritis.
Sjögren’s Syndrome. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Sjogrens-Syndrome.
Sjögren’s syndrome. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/sjogrens-syndrome/diagnosis-treatment/drc-20353221.
Undifferentiated connective tissue disease. Genetic and Rare Diseases Information Center. National Institutes of Health. https://rarediseases.info.nih.gov/diseases/12342/undifferentiated-connective-tissue-disease.
Undifferentiated Connective Tissue Disease – In-Depth Overview. Hospital for Special Surgery. https://www.hss.edu/conditions_undifferentiated-connective-tissue-disease-overview.asp