Gout and psoriatic arthritis (PsA) are both kinds of inflammatory arthritis that can cause joint pain and swelling in fingers and toes, ankles, and knees, as well as other joints. Both gout and psoriatic arthritis are chronic diseases. Having metabolic syndrome — a cluster of risk factors including obesity, high blood pressure, and high blood sugar — raises the risk for both.
Yet gout and PsA are very different health conditions with distinct causes and treatments, despite having some similar symptoms.
Read on to find out the different symptoms of gout vs. PsA, how these conditions are diagnosed and treated, and why having PsA may even increase your risk of developing gout.
The Basics of Gout
Previously called a “rich man’s disease” or the “disease of kings,” gout was once thought of as a condition that affected only wealthy men who consumed indulgent foods and drinks. We know now that gout has to do with how much uric acid you have in your blood, not how much money you have in the bank. Gout is also much more related to your genetics than your diet: While cutting back on certain foods and drinks may help manage gout to a degree, the condition usually requires medication to manage optimally. Gout can impact anyone, including the nearly 4 percent of the U.S. population living with gout today.
This does not mean that certain individuals aren’t more at risk. “Men are reported to have gout more frequently than women. However, women can get gout but do not always present with the classic podagra of gout [gout in the big toe],” says Minna Kohler, MD, director of the Rheumatology Musculoskeletal Ultrasound (MSKUS) Program at Massachusetts General Hospital in Boston.
Other risk factors for gout include:
- Obesity (BMI over 30)
- Metabolic syndrome
- Decreased kidney function (due to hypertension or diabetes, for example)
- Family history (specifically, if your father, grandfather, or brother had gout)
- Genetics
- Heavy, habitual alcohol consumption
- High consumption of foods rich in purines (red meats, organ meats, certain types of seafood)
- High consumption of high fructose corn syrup in drinks and foods
Common Symptoms of Gout
“Gout is characterized by intermittent episodes of sudden onset of red, hot, and swollen joints — one or more — with symptom-free intervals,” says Shailendra Singh, MD, FACP, Rheumatology Medical Director at White River Medical Center in Batesville, Arkansas. A gout attack can last anywhere from a few days to 10 days or longer. Gout attacks often strike in the middle of the night, so you feel sudden pain when you wake up in the morning (and with no warning). You can go to bed feeling fine and wake up with severe symptoms.
Pain in the big toe
Excruciating pain (it may hurt if your sheet touches your toe), warmth, and redness in your big toe is a hallmark sign of gout, occurring in about half of all cases. “If a patient says ‘I drank a lot of beer and woke up with a shooting pain in my toe,’ it’s likely gout,” say Fardina Malik, MD, MS, of the Center for Arthritis and Autoimmunity in the division of rheumatology at NYU Langone Orthopedic Center in New York City. But, of course, a gout diagnosis is not always that straightforward.
Pain in your knees, ankles, wrists, or elbows
“While shooting pain in the big toe is very characteristic of gout, it can affect any joint and present like psoriatic arthritis,” says Dr. Malik. Uric acid crystals can form in your foot, ankle, knee, elbow, hand, wrist, and small joints in your fingers. Roughly 25 percent of gout patients experience “polyarticular” symptoms. This means the pain strikes in more than one joint at a time — for example, the big toe and the left knee. While gout rarely impacts the spine, it can affect soft tissues in the body, including your bursae (fluid-filled sacs near certain joints, such as the hips and shoulders) and sheaths around your tendons.
Strange lumps around your joints
Called tophi, these lumps are mounds of uric acid crystals that develop under the skin and around joints. They usually occur after gout has become chronic or severe, so they’re not one of the early signs of gout.
Read more here about gout symptoms.
The Basics of Psoriatic Arthritis
Psoriatic arthritis is a type of inflammatory arthritis known for affecting the skin and nails (psoriasis) and the joints (pain, swelling, and damage). Typically, your immune system uses inflammation to help fend off disease or heal the body and then shuts it off. In people with PsA, the inflammation doesn’t shut off but instead becomes out of control, attacking healthy skin, nails, and joints. Since it’s a “systemic” disease, PsA can impact the entire body, increasing your risk for heart disease, diabetes, and depression.
The autoimmune disease psoriasis — which causes silvery red scaly patches to form on the skin — impacts roughly 2 percent of the world population. About 10 to 30 percent of people with psoriasis go on to develop psoriatic arthritis. For most people, the joint pain and swelling characteristic of PsA strike within five to 10 years of psoriasis skin outbreaks, though some patients develop skin plaques and arthritis-like symptoms at the same time and others develop arthritis symptoms first.
While the cause of psoriatic arthritis is not yet known, genetics, environmental factors, immune system problems, infection, and physical trauma can all play a role. PsA impacts men, women, and children alike.
Some of the risk factors for PsA overlap with those of gout, including having metabolic syndrome, says Dr. Malik.
Other risk factors for PsA include:
- Having psoriasis
- Family history (a parent or sibling with the disease)
- Age (between ages 30 and 50)
Common Symptoms of Psoriatic Arthritis
The symptoms of PsA can differ from person to person and depend on the type of psoriasis you have. For some, PsA may just involve the skin while others may have joint or even spine involvement. In 10 to 15 percent of cases, people get joint pain before having psoriasis skin plaques.
Classic psoriatic arthritis symptoms include:
Plaques on the skin
These red patches of skin with silvery scales often cover large areas of the body, but they can also appear in less noticeable parts of the body including the scalp, elbows, knees, and around the ears.
Swollen fingers and toes
People in the early stages of PsA can experience swelling that causes toes and fingers to look “sausage-like” as they become red, tender, and painful to bend. This condition is called dactylitis.
Painful joints
Achy, swollen, and stiff joints (typically on one side of the body and often in the lower extremities like the knees and ankles) is common for people with PsA. People with PsA who have axial involvement also have inflammation in the joints of the spine, which can cause pain and stiffness in the neck, lower back, and sacroiliac joints (where the hips connect with the pelvis). In general, PsA joint pain is worse in the morning after the body has been in a state of rest.
Heel pain and foot pain
PsA also attacks the areas where ligaments and tendons attach to the bones (entheses), causing pain and tenderness in areas of the body including the Achilles tendon as well as the back of the heel and the sole of the foot (plantar fascia). This is called enthesitis.
Nail changes
Roughly 90 percent of people with PsA develop nail changes on the fingernails and toes. This includes pitting of the nail, onycholysis (separation from the nail bed), subungual (debris under the nail), ridging (Beau’s lines), thickening, crumbling, and color changes.
Read more here about psoriatic arthritis symptoms.
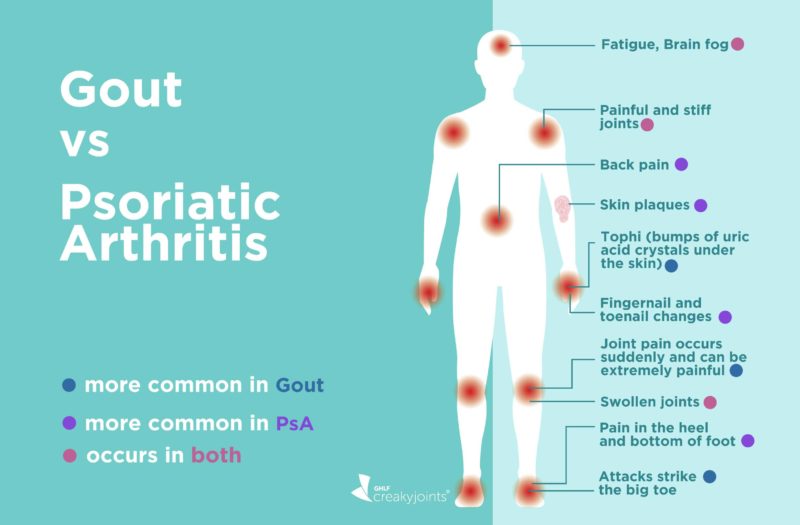
Symptoms That Gout and PsA Have in Common
While the causes of and treatments for gout and psoriatic treatment are very different, the two conditions can be confused for each other because they have some key symptoms in common:
Joint pain and stiffness
PsA and gout both cause red, hot, swollen joints. If you have acute gout, which is an episodic disease, the pain and stiffness is intermittent. It will last from one to two days to one to two weeks, with periods of no pain, says Dr. Singh.
Psoriatic arthritis, on the other hand, is associated with chronic progressive pain and swelling. “Long-term untreated gout, however, can lead to chronic gout which is difficult to differentiate from PsA,” adds Dr. Singh.
Swollen fingers and toes
Both PsA and gout can cause swelling around the fingers or toes. In PsA, however, the sausage-like appearance is called dactylitis — and it is not caused by the build-up of uric acid crystals. “When a dactylitis flare occurs, which involves inflammation of joint, tendon, and soft tissue, it can mimic an appearance of gout in the toe or finger,” says Dr. Kohler.
Fatigue
When you have PsA or chronic gout, you can feel wiped out, almost as though you have the flu. “Chronic gout and PsA can be associated with chronic fatigue mainly due to chronic inflammation,” says Dr. Singh. “Chronic inflammation can lead to anemia of chronic diseases.”
Flare-ups
All inflammatory arthritis, including psoriatic arthritis and gout, has potential to flare, says Dr. Kohler. “A gout flare can differ in that it is often associated with redness and warmth and most often associated with podagra [big toe pain and swelling],” he says. “PsA may ‘flare’ and affect axial spine or peripheral small joint arthritis.”
Overlap Between Psoriatic Arthritis and Gout
Interestingly, people with psoriatic arthritis and/or psoriasis also have a higher risk of developing gout compared to those without these conditions. According to a study in the journal Annals of the Rheumatic Diseases, the risk of developing gout was nearly five times greater for men and women with psoriasis and psoriatic arthritis. “Individual studies have varied with incident rates ranging from one to seven times higher in people with psoriasis and psoriatic arthritis,” says Dr. Kohler.
While researchers have yet to determine the exact link, possible theories include the fact that high uric acid levels in gout are thought to be a product of the high skin cell turnover and inflammation that occurs in PsA. “People with PsA have injured skin or bone that contributes to increasing inflammation, which in turn may active existing gout crystals that may be present,” says Dr. Kohler.
“We need to be mindful that just because a person has psoriasis, it doesn’t mean the acute joint pain is psoriatic arthritis,” says Dr. Malik. “It could also be gout.”
Diagnosing Gout
In many cases, primary care physicians can diagnose gout. While there’s no one simple diagnostic test, your doctor will likely give you a physical exam, ask about your history of joint pain and symptoms, and check for pain or swelling in other joints. You’ll also be asked questions about your family history and eating and drinking habits, such as whether you consume alcohol regularly.
To diagnose gout, your doctor will also give you a blood test to measure your uric acid levels, which if you have gout, are typically elevated above 6.0 mg/dL. “Gout can also be diagnosed by aspirating fluid from the swollen joint and looking for crystals of uric acid,” says Dr. Singh.
Removing and analyzing joint fluid for urate crystals is especially important when the doctor needs to distinguish gout from psoriatic arthritis.
Diagnosing Psoriatic Arthritis
If your health care provider suspects you have PsA, you’ll likely be referred to a rheumatologist for further evaluation. They will ask about your health history and skin (psoriasis), nails, joints and other symptoms and perform a physical exam. The rheumatologist will order a series of blood and imaging tests to rule out other forms of arthritis, including rheumatoid arthritis, osteoarthritis, and gout.
Read more here about how psoriatic arthritis is diagnosed.
If psoriatic arthritis symptoms are identified and treated, and a patient continues to have symptoms suspicious of gout, imaging can be helpful in specifying gout crystals contributing to symptoms. This is especially helpful if there is no joint fluid present for joint aspiration to identify gout crystals in the synovial fluid, says Dr. Kohler. “Ultrasound can identify synovitis, joint effusion, and presence of gout crystals while dual-energy CT can identify gout crystals and differentiate it from calcific crystals,” she says.
Clinching a diagnosis can be more difficult when someone has both PsA and gout, adds Dr. Singh. “One clue can be the presence of tophi — the deposition of uric acid crystals in joints and skin leading to firm nodules.” These whitish, chalk-like nodules can be seen under the skin and are typically found in the ear, elbow, and finger pulps.
Treatment for Gout vs. Psoriatic Arthritis
If you have both PsA and gout, you will need to treat both conditions. There are separate medications to treat PsA and gout. In general, PsA is treated with medication that suppresses your immune system while gout requires treatment with medications that lower uric acid in the blood and controls gout flares, says Dr. Singh.
For gout patients: The goal of gout treatment is to first reduce the inflammation causing flare-ups by using such medications as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids (also called glucocorticoids or “steroids” for short), and oral colchicine. Once an acute gout flare is under control, your doctor may prescribe medication to control your uric acid levels, including xanthine oxidase inhibitors (XOIs), uricosuric agents, and enzymes that break down uric acid.
“If there is suspicion that a patient has both gout and PsA, sometimes treating the more acute symptoms of gout first allows for more clear assessment of other arthritis involvement, and the need for additional treatment for psoriatic arthritis,” says Dr. Kohler.
For psoriatic arthritis patients: There are many drugs available to treat PsA. The ones your health care provider recommends will depend on your most troublesome PsA symptoms. Treatments and medications for psoriatic arthritis include:
- NSAIDs
- Glucocorticoids
- Disease-modifying antirheumatic drugs (DMARDs) like methotrexate, sulfasalazine (Azulfidine), and leflunomide (Arava)
- TNF inhibitor biologics like adalimumab (Humira), certolizumab pegol (Cimzia), etanercept (Enbrel), golimumab (Simponi), and infliximab (Remicade)
- Other biologics like ustekinumab (Stelara), secukinumab (Cosentyx), ixekizumab (Taltz), and abatacept (Orencia)
- JAK inhibitors like tofacitinib (Xeljanz)
- Phototherapy
- Topical creams for psoriasis skin plaques
Because both gout and PsA have risk factors related to your lifestyle and diet, patients with PsA and gout can benefit from adopting healthy habits, including:
- Reducing alcohol intake
- Avoiding sugary foods and beverages
- Eating a well-rounded diet full of fruits and vegetables
- Limited the consumption of red meat
- Getting more exercise
- Losing weight
- Controlling stress
While gout and PsA do have similar symptoms, they are ultimately distinct conditions that require individualized treatment and management. If you suspect you have gout, PsA, or both conditions, don’t wait to visit your health care provider. The sooner you get a proper diagnosis, the sooner you can start feeling less joint pain and discomfort.
Not Sure What’s Causing Your Pain?
Check out PainSpot, our pain locator tool. Answer a few simple questions about what hurts and discover possible conditions that could be causing it. Start your PainSpot quiz.
Keep Reading
Brockbank JE, et al. Dactylitis in psoriatic arthritis: a marker for disease severity? Annals of the Rheumatic Diseases. February 2005. doi: http://dx.doi.org/10.1136/ard.2003.018184.
Chen-Xu M, et al. Contemporary Prevalence of Gout and Hyperuricemia in the United States and Decadal Trends: The National Health and Nutrition Examination Survey, 2007–2016. Arthritis & Rheumatology. June 2019. doi: https://doi.org/10.1002/art.40807.
Clinical manifestations and diagnosis of gout. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-gout.
Clinical manifestations and diagnosis of psoriatic arthritis. UpToDate.https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-psoriatic-arthritis.
Gout. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Gout.
Gout. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/gout/symptoms-causes/syc-20372897.
Interview with Fardina Malik, MD, MS, Center for Arthritis and Autoimmunity in the division of rheumatology at NYU Langone Orthopedic Center in New York City
Interview with Minna Kohler, MD, director of the Rheumatology Musculoskeletal Ultrasound (MSKUS) Program at Massachusetts General Hospital in Boston
Interview with Shailendra Singh, MD, FACP, Rheumatology Medical Director at White River Medical Center in Batesville, Arkansas
Merola JF, et al. Psoriasis, psoriatic arthritis and risk of gout in US men and women. Annals of the Rheumatic Diseases. August 2015. doi: http://dx.doi.org/10.1136/annrheumdis-2014-205212.
Ogdie A, et al. The Epidemiology Psoriatic Arthritis. Rheumatic Disease Clinics of North America. November 2015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4610151.
Psoriatic arthritis. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Psoriatic-Arthritis.
Psoriatic arthritis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/psoriatic-arthritis/symptoms-causes/syc-20354076.