COPD — short for chronic obstructive pulmonary disease — is a lung condition that makes it difficult to breathe. Rheumatoid arthritis (RA) and other forms of inflammatory arthritis are joint diseases that make it difficult to move.
So, what does one have to do the other? More than you might think. Research has shown people with inflammatory forms of arthritis are likely to develop at least one chronic comorbid disorder — and COPD ranks among the highest-risk diseases for patients, compared to those without inflammatory arthritis. In fact, a study published in the journal Arthritis Care & Research suggests people with rheumatoid arthritis are nearly twice as likely to be hospitalized for COPD than the general population. Other research suggests there is an association between ankylosing spondylitis and COPD.
How COPD Makes It Hard to Breathe
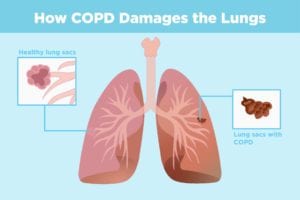
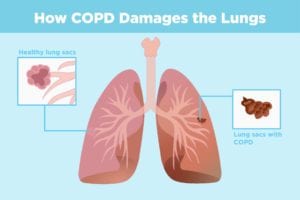
When you take a breath, air travels down your windpipe (trachea) and into your lungs through airways called bronchial tubes. These tubes branch out — kind of like a tree — into thousands of thinner tubes and end in bunches of tiny round air sacs called alveoli. Small blood vessels run along the walls of the air sacs. The oxygen in the air you inhale passes through the alveoli walls and into the bloodstream. At the same time, carbon dioxide gas (a waste product) moves out and gets exhaled. The exchange of gases brings in oxygen your body needs to function, and removes waste.
When you have COPD, less air is able to flow in and out of your lungs — which means less oxygen gets into your body and it becomes harder to get rid of carbon dioxide. The two most common conditions that contribute to COPD are emphysema and chronic bronchitis. Emphysema damages and destroys the air sacs, which impairs airflow out of your lungs. With chronic bronchitis, the bronchial tubes become inflamed and narrow, and thick mucus forms in the airways, making it hard to breathe.
COPD gets worse over time, and there is no cure. As COPD progresses, shortness of breath may prevent you from doing even the most basic activities, like walking or cooking. People with COPD are also at an increased risk of developing heart disease, lung cancer, and other conditions.
How Inflammatory Arthritis Raises Your Risk of COPD
Researchers don’t know for sure, but they suspect the same chronic inflammation that targets your joints in diseases like rheumatoid arthritis may also play a role in the development of COPD. Many of the same markers of inflammation found in RA are elevated in COPD. And exacerbations — or flare-ups — occur in both diseases.
What experts do know: Cigarette smoking is the leading cause of COPD and its main risk factor. The more years and packs you smoke, the higher your COPD risk. If you have asthma and smoke, your risk of COPD is even higher. Smoking also increase your risk of developing RA.
While most people who have COPD smoke or used to smoke, up to 25 percent of patients who have COPD have never smoked. Long-term exposure to other lung irritants — such as secondhand smoke, air pollution, chemical fumes, or dusts — also may contribute to COPD. A rare genetic disorder called alpha-1 antitrypsin deficiency can also be a factor.
Warning Signs of COPD
Early on, COPD may cause mild or no symptoms. As the disease progresses, signs include:
- Shortness of breath, even while doing everyday activities
- Chronic cough or a cough that produces a lot of mucus
- Wheezing or squeaky sound when you breathe
- Tightness in your chest
- Blueness of your lips or fingernail beds
- Frequent colds or other respiratory infections
- Swelling in your ankles, feet, or legs
- Unintended weight loss
If you experience any of these symptoms, or think you might be at risk for COPD, talk to your doctor. Though there is no cure, effective therapies are available to manage symptoms, reduce your risk of complications and flare-ups, and improve your quality of life.
How Doctors Diagnose COPD
Your doctors will consider your symptoms, family and medical history, and any exposure you’ve had to lung irritants, particularly cigarette smoke. They may order tests to diagnose your condition, such as:
Spirometry: The most common lung function test, it measures the amount of air you can inhale and exhale, how fast you can breathe air out, and how well your lungs deliver oxygen to your blood. All you have to do is take a deep breathe and blow as hard as you can into a tube connected to a small machine called a spirometer. Spirometry can detect COPD even before you have symptoms of the disease. It can also be used to track the progression of disease and check how well treatment is working.
Chest X-ray or CT scan: These tests help detect emphysema (a main causes of COPD), as well as rule out other lung problems or heart failure that may be causing symptoms.
Arterial blood gas test: It measures oxygen levels in your blood and can help show the severity of your COPD.
How to Help Prevent COPD and Keep Your Lungs Healthy
COPD is a major cause of disability, and the fourth-leading cause of death in the United States, according to the National Heart, Lung, and Blood Institute. About 16 million people are diagnosed with COPD, and many more may have the disease and not know it.
To help prevent COPD or slow the progression of the disease:
Stick to your RA treatment plan. Keeping your RA disease activity under control can help reduce inflammation in your body. (You can use our ArthritisPower app to track your symptoms and disease activity and share your results with your doctor.)
Stub out cigarettes for good. Smoking is why most people develop COPD in the first place; it can also make your COPD and RA worse. For help quitting, talk with your doctor or go to smokefree.gov.
Avoid exposure to secondhand smoke. Smoke from other people’s cigarettes may also contribute to lung damage. Take care to protect yourself against other irritants — such as chemicals, dust, and fumes — in your home and at work.
Get vaccinated. Respiratory infections are common in RA and COPD, and complications could be severe. Talk with your doctor about getting flu and pneumonia vaccines. (Learn more about the importance of vaccines when you have arthritis.)
Tell your doctor about any breathing problems. Sometimes people think they’re short of breath or less able to do normal activities because they’re “just getting older.” Shortness of breath can be an important symptom of lung disease. Report any COPD symptoms right away — lung issues that are detected earlier are easier to treat.





