CreakyJoints Community Question
Thanks for participating! Your answer has been recorded.
Check out relevant CreakyJoints content below.
![]()
Is getting your arthritis to go into remission a goal for you?
If you have inflammatory arthritis such as rheumatoid arthritis, psoriatic arthritis, or ankylosing spondylitis, chances are that you and your rheumatologist have talked about the possibility of going into remission.
Remission means different things to different patients — some people think of remission as having no symptoms; others might consider themselves in remission even if they have occasional arthritis flares but feel well most of the time.
As a general rule, remission in diseases like rheumatoid arthritis is considered to be “inactive disease” — as measured both by blood and imaging tests as well as patients’ self-reported symptoms. “Low disease activity,” on the other hand, is a state where symptoms are under control and where you feel like you can maintain a good quality of life.
You can use our ArthritisPower app to track your symptoms and disease activity and share your results with your doctor. This information can be very helpful when discussing remission with your doctor.
Decades ago, remission wasn’t conceivable for most patients, but thanks to advances in treatment, a proliferation in treatment options, and a more aggressive “treat to target” treatment philosophy among rheumatologists, getting to remission is a possibility for many patients. “Treat to target” generally means picking a disease management goal (such as low disease activity or remission) and working with your doctor to adjust your treatment plan as needed in order to hit that target.
According to a 2017 paper about sustained remission in RA, the goal of treatment has transformed in recent decades from managing symptoms to preventing disability and long-term damage to early and persistent remission.
“With changes in the therapy approach, the course of the disease nowadays can be truly modified. These existing advantages have transformed the view on the ultimate course of RA as a chronic disabling disease to a potentially curable condition by possibility to switch off autoimmunity and induce immune tolerance,” according to the paper’s authors.
Whether or not achieving remission is a goal for you, of course, is very personal. It may depend on how long you’ve been living with inflammatory arthritis, how you feel about the risks and benefits of medication side effects, whether you’ve already sustained joint damage from your arthritis, and what other risk factors or comorbid diseases you have. For example, 2018 research presented at the annual meeting of the American College of Rheumatology found there were a few factors that made RA remission within a year of getting diagnosed more likely:
- Being at a healthy weight
- Not smoking
- Using methotrexate
If remission is a goal, be proactive in bringing it up with your doctor instead of waiting for them to address it. While it takes time to accept that you have a chronic disease, starting aggressive treatment sooner increases the likelihood that remission is possible for you (more on this below).
While you may hear stories about people going into remission without medication, this is quite rare. Patients cannot rely on lifestyle or dietary changes alone to reverse the course of disease, though of course these are helpful as part of the right medication plan.
This article has good information about how to talk about remission with your rheumatologist. Here are three takeaways from it that arthritis patients can use to explore remission as part of shared decision-making with their doctor.
- Don’t put off seeing a rheumatologist if you suspect you could have arthritis.
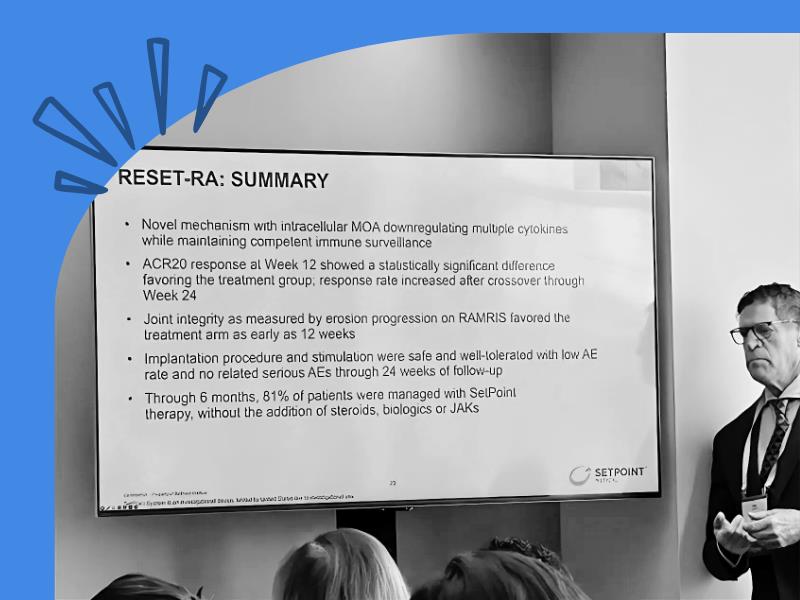
“Remission is most easily achieved among patients with a relatively short duration of RA, usually less than two years. Patients with a long duration of disease may have pain that will not respond well to immunosuppressive treatment, and for them, low disease activity may be a more appropriate target,” says Daniel Solomon, MD, MPH, professor of medicine at Harvard Medical School and chief of clinical sciences in the division of rheumatology at Brigham and Women’s Hospital in Boston.
- Talk openly with your doctor so you can set a treatment target together.
“People have varying risk thresholds. Some are comfortable with low disease activity and are not willing to increase their medication to get further benefit. Others are willing to escalate their care until they are in remission, if possible,” says Liana Fraenkel, MD, MPH, adjunct professor of medicine at the Yale University School of Medicine and director of patient centered population health services at Berkshire Health Systems in Pittsfield, Massachusetts.
- Report how you’re doing to your doctor, not only in terms of pain but how you function in daily life.
Remission or low disease activity isn’t just about what your bloodwork shows or how many swollen or tender joints your doctor can count. How your disease affects your daily functioning is important too. Have there been changes in doing things that used to be difficult, such as opening jars or getting dressed? How are you functioning at work? Can you get done what you need to during the day? How tired are you? If a certain activity used to bring on a flare, is that getting less or more severe?
For more information on this topic, you might be interested in reading the following articles:
![]()
Track Arthritis Symptoms Like Sleep with ArthritisPower
Consider joining ArthritisPower, the first ever patient-led, patient-generated research registry for people with autoimmune arthritis and related conditions. You can make a difference in the fight against autoimmune arthritis and related conditions. Here’s how:
- Track your symptoms and treatments: Keep tabs on your health with tracking tools on your PC or smartphone.
- View your data over time: Empower yourself with personal data to better understand your symptoms.
- Share your information with your doctor: Get customized reports that summarize all the information you have logged.
- Make a difference: Speed the arrival of personalized medicine by helping researchers better understand how different treatments work for different people.