Key Takeaways:
- Patients and rheumatologists agree on the importance of adding or switching medications to prevent long-term joint damage and other RA complications.
- For doctors, treat-to-target is a dominant factor in treatment-switching decisions.
- For patients, trade-offs, risk and benefits, and pros and cons are common factors in treatment-switching decisions.
- People with RA look for information from peers to make decisions about medication and disease management.
If you live with rheumatoid arthritis (RA), a chronic inflammatory disease that causes joint pain and swelling, fatigue, and a host of other symptoms, you’ve likely had to change, add, or adjust medications in your treatment plan.
While taking medication (namely disease-modifying antirheumatic drugs, or DMARDs) to reduce inflammation and disease activity is usually necessary to manage RA symptoms, it’s not always easy to find the right treatment. Finding what works for you requires many considerations. What provides effective symptom relief while minimizing side effects? What’s the best option given your medical history, past treatments, personal preferences? Trial and error is often required.
Another factor that affects whether or how often RA patients switch medication is if their rheumatologist is following is a “treat-to-target” approach. This is a treatment strategy that entails frequent monitoring and tuning treatment regimens (like switching or adding DMARDs) to get a patient to a predetermined goal, such as low disease activity. The strategy is part of the American College of Rheumatology’s latest treatment guidelines for RA.
Yet despite these recommendations, studies have found that fewer than half of people with RA are following a treat-to-target approach. Researchers at Yale-New Haven Medical Center, Carnegie Mellon, and a team of other research partners, including the Global Healthy Living Foundation (GHLF), set out to better understand why. They collaborated with experts who study the science of decision-making, focusing on something called “the mental models approach to risk communication.” A mental model describes how a group of people think and feel about a specific idea.
The researchers wanted to dive more deeply into how patients and rheumatologists each approach treatment decisions for RA. Their goal is to help improve communication and increase understanding — so doctors can have more insight into patients’ thoughts and concerns, and so patients can learn more about why their doctors are making certain recommendations.
“We don’t expect to change or escalate a patient’s immunosuppressant medication all of the time — sometimes a patient has an infection, or just started a medication last week, or there’s an insurance problem,” says Liana Fraenkel, MD, MPH, Professor of Rheumatology at Yale School of Medicine and Section Chief of Rheumatology at Berkshire Medical Center. But it happens at such a low rate compared to when it would be recommended for patients’ symptoms and disease activity that the research team wondered why.
“If patients were thinking the way the rheumatologists were thinking, then changes would happen more frequently,” says Dr. Fraenkel, who is the lead author on two recent and related studies on this topic.
In one study presented during ACR Convergence 2021, the annual meeting of the American College of Rheumatology, the research team interviewed 14 rheumatologists and 30 rheumatoid arthritis patients one at a time to explore all the factors that influence their decisions when it comes to starting or changing RA treatment. Then they did a separate, larger survey of RA patients to test their findings further. Participants were mostly non-Hispanic white females (average age 57).
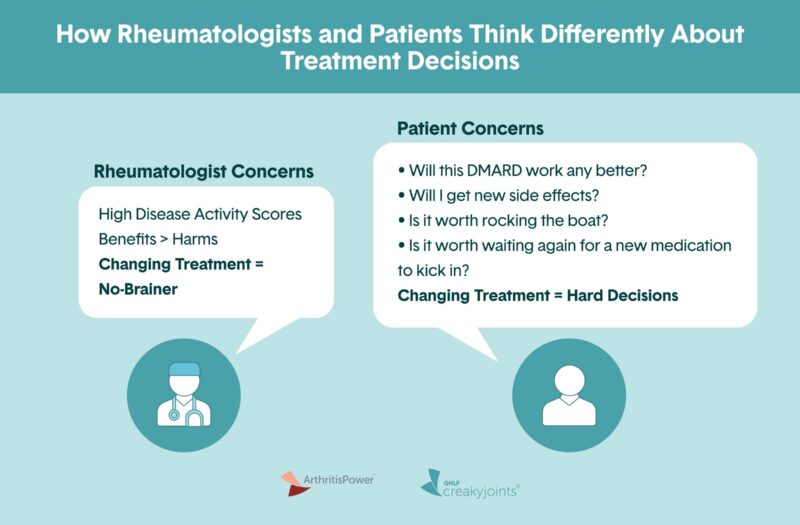
Patient vs. Physician Mental Models
A mental model is essentially how a group of people thinks and feels about a specific idea, including all the factors that influence how they make decisions about that idea. “It can include their childhood, culture, education, peer pressure, what their neighbor thinks, social media feeds – everything,” says Dr. Fraenkel.
When researchers compared the mental models of rheumatologists and patients, they found a few common factors in treatment decision-making — notably, the importance of adding or switching medications to prevent long-term joint damage and other disease complications.
Not surprisingly, there were key differences in the mental models of rheumatologists compared to those of RA patients.
“For physicians, treat-to-target is a dominant decision, which means there is no decision, so for us it’s very easy,” explains Dr. Fraenkel. “You have ‘A’ and I recommend ‘B.’ I can measure this; I have a number; it is clear to me what’s going on; I just recommend that you escalate care.” In other words, doctors use objective measures like disease activity numbers or blood tests to determine whether to escalate treatment.
But for patients, treatment decision-making was more complex, with additional factors like fear of side effects, medication fatigue, and skepticism about whether the treatment will work.
Physicians’ mental models
For rheumatologists, treat-to-target is a “no-brainer; it’s pretty straightforward,” says Dr. Fraenkel. “You measure disease activity and, if disease activity is due to inflammation and not at target, you discuss how to change medication so you can reach that target.”
Doctors also discussed many other factors related to treat-to-target beyond disease activity, including:
- Disease trajectory, or how the disease has changed over time
- Decision inertia, or the preference to stay with the status quo rather than make a change
Patients’ mental models
“Many patients don’t know what treat-to-target is — they just think of it as adding or switching their medications,” says Dr. Fraenkel.
Instead, RA patients shared other factors important to them in decision-making, beyond numbers like disease activity scores or blood work results, including:
- Preference sensitivity, which means considering tradeoffs when making a treatment decision, such as, “Will this DMARD work any better than my current one?” “Will I get new side effects?” “Is it worth rocking the boat?” “Is it worth waiting again for a new medication to kick in?”
- Importance of being informed by their health care provider and by peers about their personal experiences with a particular medication
- Medication fatigue or feeling exhausted by the trial-and-error cycle of starting or changing medications
“Deciding whether to escalate care is not a slam dunk choice for the vast majority of people with RA,” says Dr. Fraenkel. “As physicians, we need to get out of that mindset and appreciate that there are trade-offs and support patients through those trade-offs. That to me is one of the most important findings; it’s a big deal.”
The Value of Patient-to-Patient Advice
Another key (and humbling) finding from the research, says Dr. Fraenkel, was that RA patients said that their doctors can’t always provide them with all the information they need to make treatment decisions. While they respect their rheumatologist and emphasized the importance of getting good information before starting a medication, they also wanted to hear from their peers about their personal experience and valued those insights.
“For hesitant patients, the physician is necessary but not sufficient,” says Dr. Fraenkel. “I can tell them about the studies and science, but I’m not in a position to tell them another piece of information that is just as important: what it’s like in the real world on this medication.”
Dr. Fraenkel says these findings will change the way she works with and communicates with her patients, and she hopes other rheumatology providers will follow suit. “Even if you know in your brain that DMARDs are good and important, your heart may have a hard time changing,” she says. “Just telling patients over and over that [DMARDs] are good for you is not going to help. We need to do something else.”
Found This Study Interesting? Get Involved
If you are diagnosed with rheumatoid arthritis, or another rheumatic or musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
Hsiao B, et al. Rheumatologists’ and patients’ mental models for treatment of RA explain low rates of TTT [abstract]. Arthritis and Rheumatology. November 2021. https://acrabstracts.org/abstract/rheumatologists-and-patients-mental-models-for-treatment-of-ra-explain-low-rates-of-ttt/.
Hsiao B, et al. Understanding heterogeneity in patients’ conceptualization of treatment for rheumatoid arthritis: a cluster analysis [abstract]. Arthritis and Rheumatology. November 2021. https://acrabstracts.org/abstract/understanding-heterogeneity-in-patients-conceptualization-of-treatment-for-rheumatoid-arthritis-a-cluster-analysis/.
Interview with Liana Fraenkel, MD, MPH, Professor of Rheumatology at Yale School of Medicine and Section Chief of Rheumatology at Berkshire Medical Center.