Finding the right treatment plan for your psoriatic arthritis (PsA) is not always a simple or straightforward process. For one thing, PsA, a type of inflammatory arthritis that typically affects both the skin and the joints, can cause a wide range of symptoms that affects each patient differently. Certain medications are more effective for some types of symptoms than others — say, clearing psoriasis skin plaques vs. treating joint pain and swelling.
What’s more, each person living with psoriatic arthritis has their own unique needs and preferences when it comes to finding a treatment that helps improve their quality of life. Some people may find fatigue to be a big problem; others may be more concerned about their ability to be physically active. And the ideal treatment plan should be convenient so you’ll stick with the medication.
As more treatment options become available for psoriatic arthritis, it’s critical to understand more about what patients want from their treatment. This can help health care providers and patients to partner on personalizing the treatment plan to make sure it not only improves PsA symptoms and prevents disease progression and complications, but also helps improve quality of life so that patients feel satisfied overall.
A new study from the Global Healthy Living Foundation (GHLF) and CreakyJoints conducted in partnership with RTI International explored these issues by asking psoriatic arthritis patients which PsA symptoms they perceived to be most bothersome and which aspects of their quality of life they most wanted to see improved. The study also asked how patients felt about medications and their potential to relieve PsA symptoms as well as their preferences for mode and frequency of treatment. Initial findings from the study were presented during the European E-Congress of Rheumatology 2021.
Psoriatic arthritis patients (332) from our ArthitisPower research registry completed the survey. Most had experience with advanced therapy for PsA (about 75 percent had used at least one biologic medication currently or in the past). The patients were mostly female (80 percent) and white (94 percent), so the results may not be representative of all patients with PsA. The average age of participants was 54 and the average time since PsA diagnosis was nine years. Note that while psoriasis often starts in adolescence or young adulthood, psoriatic arthritis typically begins affecting people between the ages of 30 and 50, according to Medline Plus.
Here is what we learned.
PsA patients are most bothered by joint pain-related symptoms and less bothered by psoriasis symptoms
As part of the survey, people were given a list of 11 common psoriatic arthritis symptoms and asked to choose the one symptom that bothered them the most, as well as the one symptom that bothered them the least. The psoriatic arthritis symptoms they could select from were:
- Joint pain
- Joint swelling
- Lower back or spin pain
- Sausage fingers or toes
- Morning stiffness
- Tender or painful tendons or ligaments
- Fatigue or tiredness
- Psoriasis patches on skin and scalp
- Nail pitting
- Itching because of psoriasis patches
- Skin pain and discomfort related to psoriasis patches
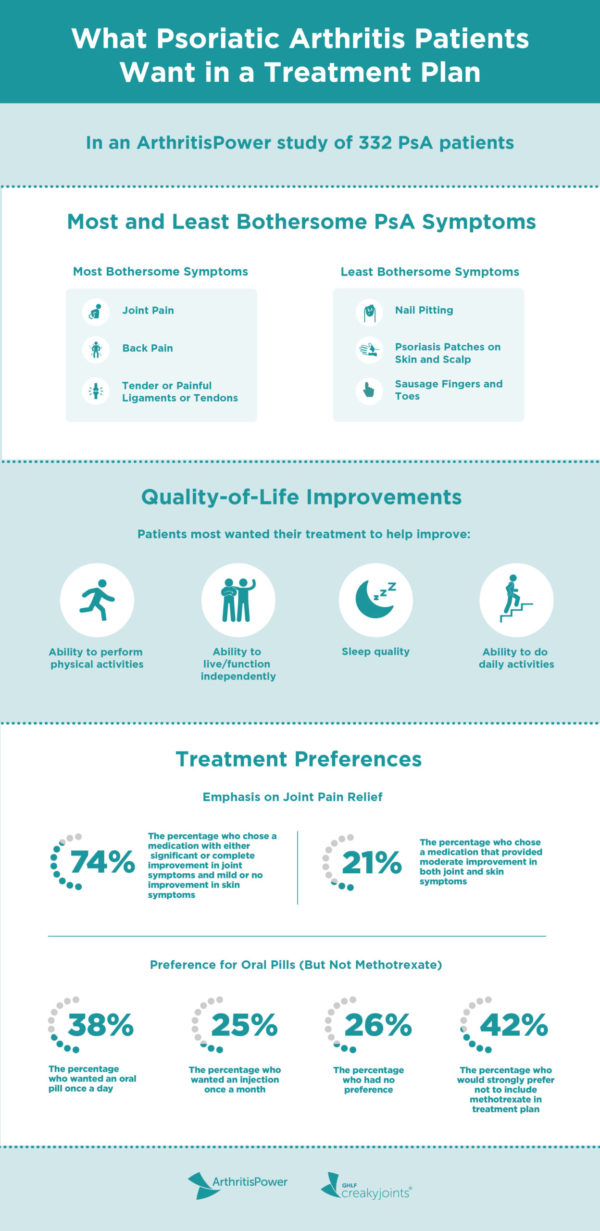
Overall, patients reported that they were most bothered by joint pain-related symptoms. This includes joint pain, which was found to be the most bothersome symptom; lower back or spine pain; and tender or painful tendons or ligaments.
Fatigue and joint swelling were considered half as bothersome in relation to joint pain, but still more bothersome than other symptoms listed.
The symptoms ranked the least bothersome were more appearance-related than pain-related. Nail pitting was deemed least bothersome, followed closely by psoriasis patches on skin and scalp.
PsA patients want their medication to improve joint pain symptoms
The study included other evidence to support the theory that pain-related symptoms are more bothersome for PsA patients than other symptoms.
As part of the survey, participants were asked to choose between five hypothetical medicines that traded off different levels of improvement in skin and joint symptoms. Most patients (74 percent) chose a medicine with either significant or complete improvement in joint symptoms and mild or no improvement in skin symptoms, while 21 percent chose a medicine that provided moderate improvement in both joint and skin symptoms. This further suggests that pain-related symptoms are the most bothersome and have the greatest impact on patients’ daily lives compared to non-pain-related symptoms, like nail pitting, skin plaques, and swollen fingers.
Being able to perform physical activities is extremely important to PsA patients
Participants were given a list of nine ways PsA impacts their quality of life and asked to choose the one that was most important to improve through treatment as well as the one that was least important to improve. They included:
- Sleep quality
- Ability to perform physical activities (exercising, walking, climbing stairs)
- Emotional well-being
- Ability to do daily activities (housework, chores, etc.)
- Ability to live/function independently
- Ability to work or do school activities
- Ability to participate in social activities
- Ability to participate in leisure activities
- Unpredictability of disease flareups
Patients said they most want to improve their ability to perform physical activities. This is not surprising, as the joint pain-related symptoms that patients deem bothersome likely affect their ability to be active. Patients also want to improve their ability to live and function independently.
Patients least wanted to improve their ability to participate in leisure activities and social activities.
PsA patients prefer medication in the form of an oral pill taken once a day
The treatment plan portion of the survey allowed people to share how and how often they prefer to receive PsA treatment. Patients were asked to rank four different ways of taking their psoriatic arthritis medication — oral tablet once a day, oral tablet twice a day, an injection every two weeks, or an injection once a month — from most preferred to least preferred. When it came to their first-choice treatment:
- 38% said oral tablet once a day
- Less than 1% said oral tablet twice a day
- Less than 1% said oral tablet twice a day
- 25% said injection once a month
- 26% said they had no preference
Convenience and ease were the main factors in patients’ preferred treatment choice. The top three reasons patients listed for choosing a one-a-day oral treatment were: it’s fast and easy to take (68 percent); it’s easier to travel with (49 percent); and it’s easier to remember (34 percent.)
PsA patients prefer a treatment plan that does not include methotrexate
In this section, patients were also asked about their experience with the disease-modifying antirheumatic drug (DMARD) methotrexate (MTX) and whether they want it as part of their treatment plan. The majority of patients said they would strongly prefer (42 percent) or somewhat prefer (18 percent) a PsA treatment that did not include methotrexate. Of the patients who have already used methotrexate, 15 percent were somewhat dissatisfied with their experience and 32 percent were very dissatisfied.
Methotrexate is an immunosuppressive drug that is commonly prescribed to people with psoriatic arthritis, as well as rheumatoid arthritis (RA). Despite methotrexate’s ability to reduce symptoms and help prevent disease progression, many inflammatory arthritis patients say they ultimately stop taking MTX because of side effects (such as nausea and fatigue). Indeed, side effects were among the reasons patients in were unhappy with methotrexate. When given the opportunity to share why they were not happy with this treatment:
- 58% said dislike of short-term side effects
- 53% said lack of efficiency
- 44% said fear of long-term side effects
Health care providers should consider patient experience and preference when developing a PsA treatment plan
“It’s important to understand how people living with PsA experience common symptoms, such as pain, stiffness, and fatigue, as well as their goals for treatment so that we can develop new management strategies that reflect their preferences,” lead author Alexis Ogdie, MD, Associate Professor of Medicine and Epidemiology and rheumatologist at the University of Pennsylvania, said in a press release.
Dr. Nowell agrees, adding that “understanding what patients are worried about and what matters to them is important,” and health care providers should seek to treat the individual patient as well as the general disease.
If you feel your current treatment plan is not adequately easing symptoms or improving your quality of life, talk to your doctor.
Track Your Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and log your medications to track side effects and impact on disease activity. Learn more and sign up here.
This study was supported by AbbVie, which is a corporate sponsor of the Global Healthy Living Foundation.
Interview with W. Benjamin Nowell, PhD, Director of Patient-Centered Research at the Global Healthy Living Foundation
New ArthritisPower Data Highlights Contradiction Between Patients Expressing Satisfaction with Treatment Despite Breakthrough Symptoms. Press Release. June 2, 2020.
Nowell WB, et al. Real-World Patient Experience and Treatment Preferences in Patients with Psoriatic Arthritis. Annals of the Rheumatic Diseases. Volume 80, Supplement 1. 2021.
Psoriatic Arthritis. Medline Plus. https://medlineplus.gov/genetics/condition/psoriatic-arthritis