If you have psoriatic arthritis (PsA), you’re probably aware that about 85 of people with PsA also have psoriasis (an inflammatory condition of the skin). As if dealing with joint pain, fatigue, and scaling, burning, and itching skin isn’t enough – you may also experience symptoms that go beyond your skin and joints. That’s because the chronic inflammation underlying your PsA can go to work body-wide, affecting organs, tissues, and body systems beyond the skin and joints.
Reporting these symptoms to your doctor as soon as possible can help fend off more serious problems and lead to more effective relief for your PsA. It’s also essential to note: If you have psoriasis, these symptoms may be the earliest clues that you may have PsA.
Symptoms of Psoriatic Arthritis We Don’t Always Talk About
Here’s a closer look at some of the PsA symptoms that can fly under the radar and what you should know about them.
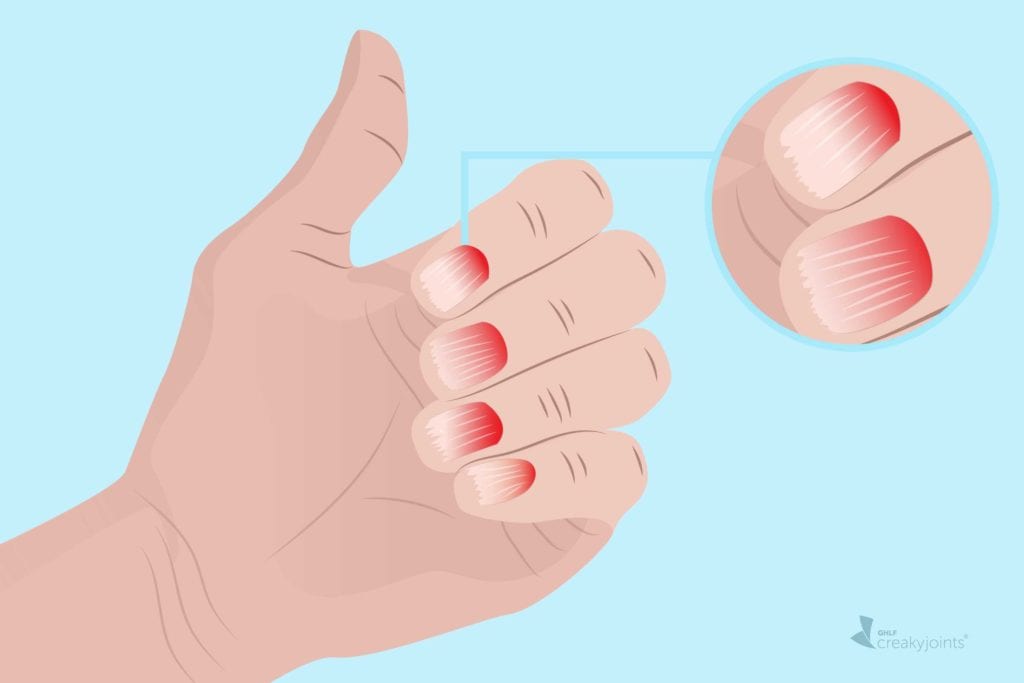
Nail Problems
If you have psoriasis and have not yet been diagnosed with psoriatic arthritis (PsA), or if you have unexplained joint pain without skin issues, it’s worth checking your nails. Nail pitting is one of the earliest and most common signs of PsA, affecting about 80 percent of all people with psoriasis. “It looks almost like you poked your nail with a safety pin,” says Emily Carroll, MD, an internist focusing on rheumatological diseases at New York’s Mount Sinai Hospital. Onycholysis, which is the splitting, easy breaking, or cracking of the nail bed, is another nail sign.
In fact, nail issues are such a telltale sign of PsA that, according to Dr. Carroll, “when someone is coming in with new joint pain and we’re trying to figure out why they have it, and they don’t have obvious skin manifestations, I will look at the nails…sometimes that is the only skin sign.”
This is what happened to Eddie Applegate, a TV-commercial traffic manager in Atlanta. “I was having joint pain and rashes on my face and hairline,” says Eddie, who has been living with PsA for 20 years. “I went to an urgent care doctor who looked at my nails and saw the pitting, and that helped him confirm the diagnosis of PsA. He also looked at the rash on my face and said, ‘That’s psoriasis’ — a dermatologist had earlier misdiagnosed it as acne.”
Eye Issues
When it comes to PsA, “red eyes, changing vision, and especially painful eyes are concerning,” says Dr. Carroll. Those are symptoms of a condition called uveitis, or inflammation of the uvea, which is the middle layer of the eye. Left untreated, it can lead to vision loss, so it’s important to see an ophthalmologist.
Adds Dr. Carroll, “If uveitis occurs even though a person with PsA is already taking methotrexate, this might be a reason to go to a stronger treatment, such as a biologic.”
PsA can also be associated with less serious eye problem, including:
- Pink eye (redness, crusting, swelling)
- Dry eye syndrome (gritty, burning sensation)
- Swelling of the sclera (the white part of the eye)
Ashley Krivohlavek, 39, has had psoriasis since she was 12 years old and was diagnosed with psoriatic arthritis (PsA) when she was 30. She says that dry eyes are “especially tragic” for her, mainly because of the blow to her vanity.
“When I was a kid, I got made fun of in school for glasses. Eventually, I started wearing contacts and was happy, but about two years after my PsA diagnosis, my ophthalmologist said, ‘You have extremely dry eye, and I don’t know if you’ll be able to wear contacts,” recalls Ashley. “The arthritis had already taken so much — I couldn’t play bass or piano anymore. I like to travel, and that wasn’t in the cards either — and now this.”
Ashley had been able to wear contacts for special occasions until about six months ago, when she wore them to a wedding but found removing them so painful that she feared she had scratched her cornea. “My doctor told me I had zero chance to wear contacts ever again,” says Ashley, who now keeps her eyes lubricated with over-the-counter eye drops and may explore stronger options with her doctor.
Shortness of Breath
Unfortunately, people with PsA are at higher risk of atherosclerosis, heart attack, and stroke, says Dr. Carroll. “One reason is that PsA is seen more commonly in people who have metabolic syndrome, a cluster of conditions including high cholesterol, high blood pressure, and obesity,” she explains. “But even beyond that, the inflammatory nature of PsA alone raises risk.”
The same inflammation that attacks joints also attacks blood vessels, leading to narrower arteries and plaque buildup. So, if you experience shortness of breath when doing everyday activities, tell your doctor and have it checked out. It could be a sign of heart disease.
Luckily, Ashley, who does arthritis advocacy work through the Global Healthy Living Foundation and helps her dad run their asphalt manufacturing business in Tulsa, OK, has no heart issues, but she says, “I’ve been very diligent about checking my heart health because of the inflammation from PsA. I got tested recently, and my endocrinologist says everything looked great.”
Eddie’s PCP does an EKG at least once a year: “He wants to make sure we get ahead, especially because I have a family history of heart disease.”
Swollen Digits
Even before any joint problems have been detected, PsA may reveal itself with fingers or toes so swollen they look like sausages. Known as dactylitis, it affects about half of people with PsA at some point during the course of the disease and is often a signal of joint damage. “When I was first diagnosed and not on a good treatment plan, my fingers would swell so badly, I couldn’t put bracelets or rings on,” says Ashley. “The swelling in my toes was so bad that wearing anything other than big, bulky athletic shoes was really difficult.”
If you notice symptoms — your entire finger or toe (not just the knuckle) might be so swollen you won’t really be able to use it, and it may feel warm and painful — see your doctor right away. Prompt treatment, such as with biologics or JAK inhibitors, can help ensure dactylitis doesn’t become a chronic problem. “Finding the right treatment plan really did help a lot,” says Ashley, who started managing her PsA with a biologic two years ago. “It has given me my life back.”
Back Pain
Although PsA is known for causing peripheral arthritis — inflammation and stiffness in the hands, wrists, feet, knees, and ankles — it can also attack elsewhere.
“One of the things people don’t really talk about is the spine in PsA,” says Ashley, who underwent physical therapy for her spine last summer. “Even my rheum, when I brought it up, said PsA doesn’t really do that.”
However, a study in Annals of the Rheumatic Diseases found that about 43 percent of people with PsA also have back symptoms — also known as axial PsA or spondylitis. “It’s the worst because walking hurts, lying down hurts. It just feels very tight and almost burning, like there’s stuff rubbing together,” says Ashley.
If you’re experiencing back pain, tell your rheumatologist — certain imaging tests can help them make an accurate diagnosis and adjust your treatment accordingly.
Not Sure What’s Causing Your Pain?
Check out PainSpot, our pain locator tool. Answer a few simple questions about what hurts and discover possible conditions that could be causing it. Start your PainSpot quiz.
Jadon, D, et al. “Axial Disease in Psoriatic Arthritis Study: Defining the Clinical and Radiographic Phenotype of Psoriatic Spondyloarthritis.” Annals of the Rheumatic Diseases. April 2017. doi: https://doi.org/10.1136/annrheumdis-2016-209853.
Jha, S, et al. “Nail Pitting: A Key Clinical Sign of Psoriatic Arthritis.” Rheumatology 58, no. 12 (December 1, 2019): 2250–2250. https://doi.org/10.1093/rheumatology/kez183.
Zhu, T, et al. “Cardiovascular Risk in Patients with Psoriatic Arthritis.” International Journal of Rheumatology. 2012. doi: https://doi.org/10.1155/2012/714321.