If you’re one of the 10 percent of people worldwide coping with migraine, you’re likely used to managing symptoms like head pain, light or sound sensitivity, nausea and vomiting — but are you also paying attention to your bone health?
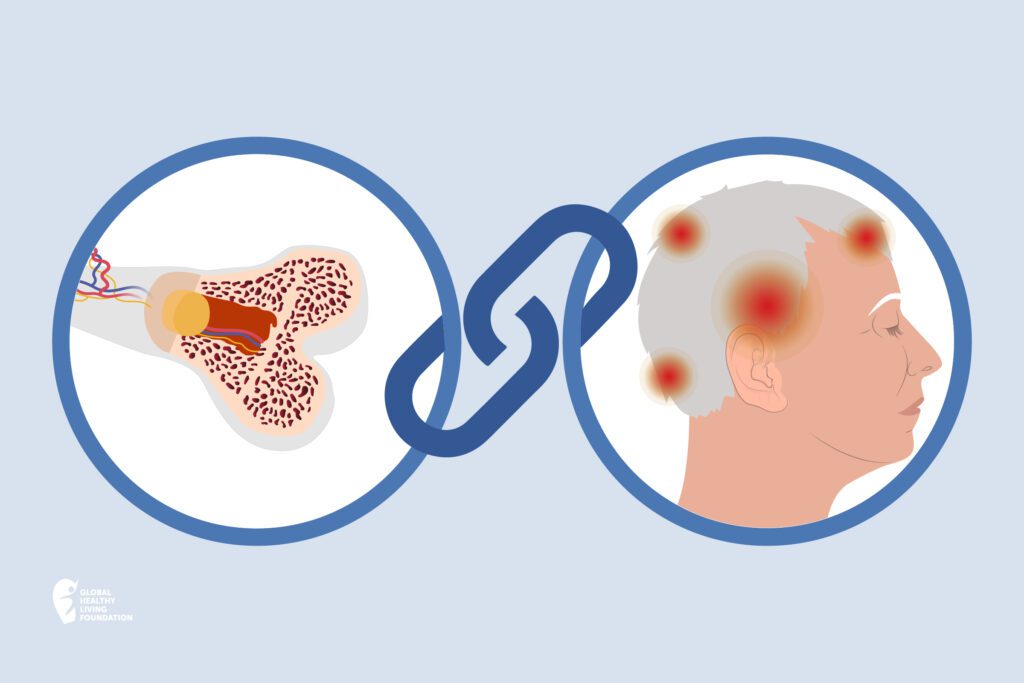
While migraine is a neurological disorder and osteoporosis is a bone condition, there is some overlap. “If someone has a history of osteoporosis, they have an increased risk of migraine, explains Jan Lewis Brandes, MD, MS, Vice President of the National Headache Foundation.
Learn more about the link between migraine and osteoporosis — and what you can do to best manage both conditions.
The Link Between Migraine and Osteoporosis
According to a Taiwanese nationwide population-based study, the overall incidence of migraine was 1.37-fold higher in those who had osteoporosis compared to those who didn’t. Osteoporosis causes bones to become weak, brittle, and break more easily. And it’s common, impacting more than 200 million people across the globe.
A number of factors may tie these two conditions together:
Hormones
“We know that [the hormone] estrogen protects bones, and typically, if estrogen levels are stable, that’s usually protective in migraine,” says Brandes. But when estrogen levels drop, like with menopausal women, it can impact both migraine and osteoporosis risk.
In fact, research shows that postmenopausal women are more likely to develop osteoporosis due to estrogen deficiency.
A recent review also found that a decline in estrogen levels can trigger a migraine — and women who get migraines tend to have an increased sensitivity to changes in estrogen levels.
Migraine Medication
“Sometimes we use steroids in particular situations to treat migraine,” says Brandes. These drugs may be used to treat severe migraine attacks in a hospital setting, or to treat a sustained migraine.
While these medications are typically prescribed as a short-term migraine treatment, long-term steroid use has been tied to an increased risk of osteoporosis.
Researchers are looking into whether the use of anti-CGRPs, another migraine treatment, may also decrease bone loss and impair bone fracture healing, though more studies are needed to understand the long-term consequences of anti-CGRPs.
Osteoporosis Medication
“Ironically, some of the medicines for osteoporosis can also aggravate migraine,” adds Brandes.
Headaches are a rare side effect of bisphosphonates, the gold standard osteoporosis treatment. In particular, research shows intravenous bisphosphonates may bring on a headache within one to three days after infusion. Though taking painkillers like acetaminophen or non-steroidal anti-inflammatory drugs can help alleviate headache pain.
Lifestyle Habits
Numerous lifestyle habits can impact both migraine and osteoporosis, notes Brandes. That includes:
- Smoking
- Being sedentary
- Malnutrition
Osteoporosis Risk Factors
While a history of migraine can increase your risk of developing osteoporosis, other risk factors may also play a role in the onset of osteoporosis. And many of the risk factors for both migraine and osteoporosis overlap.
Risk factors can be broken into two groups: uncontrollable and controllable. By familiarizing yourself with the many risk factors tied to osteoporosis, you can have an informed conversation with your health care provider about your personal risks and what you can do to better protect your bones.
Uncontrollable risk factors for osteoporosis include:
- Gender: Osteoporosis is more common in women, especially in premenopausal women.
- Ethnicity: Osteoporosis is more common in Caucasian and Asian women.
- Age: The older you get, the higher your risk of developing osteoporosis.
- Family history: If an immediate family member (like a parent) has osteoporosis, your risk of developing the condition increases.
Controllable risk factors, or those you can modify, include:
- Medications: Ask your doctor if any of the medications you take for migraine or other conditions may increase your risk of osteoporosis.
- Diet: Low calcium and vitamin D intake may increase your risk of osteoporosis.
- Inactivity: Being sedentary can weaken your bones.
- Weight: Being underweight (or having a small body frame) can affect bone health.
- Smoking: Smoking cigarettes makes you more prone to osteoporosis and bone fractures.
- Alcohol: Excessive alcohol consumption impacts how the body absorbs calcium and vitamin D, both of which are critical for healthy bone development.
Osteoporosis Symptoms
Osteoporosis is sometimes referred to as a “silent” condition. That’s because it often has no symptoms.
As it progresses, it can lead to symptoms like:
- Back pain
- Sudden back pain
- Joint pain
- Changes in posture
- Stooping or loss of height
But most people don’t realize they have osteoporosis until they fracture or break a bone. That’s why it’s so important to learn about osteoporosis and take steps to protect your bones.
Tips to Manage Migraine and Protect Your Bones
Because both migraine and osteoporosis are so prevalent amongst women, according to Brandes, one of the main things you can do is talk to your doctor about monitoring your estrogen levels, especially as you enter menopause, and take estrogen therapy as needed.
Making certain lifestyle changes can also help manage migraine and protect your bones.
Stay Active
Exercise is probably the last thing you’ll feel like doing during a migraine attack. But when you’re feeling well, studies have shown that staying active can help reduce future attacks. Exercise also helps improve sleep and reduce stress, two common migraine triggers.
Regular exercise also helps build muscle, strengthens bones, and improves balance to reduce the risk of fall-related fractures. “Weight bearing exercise appears to make a significant difference,” emphasizes Brandes.
Eat a Nutritious Diet
Eating a variety of fruits and vegetables, whole grains, lean proteins, and healthy fats can help promote overall health and prevent malnutrition, which according to Brandes, can play a role in both migraine and osteoporosis.
While there’s no one diet to promote bone and joint health, studies have found that adequate calcium and vitamin D intake can help promote bone health. Women ages 50 and under and men ages 70 and under should aim to get 1,000 mg of calcium each day and increase intake to 1,200 mg each day once women reach age 51 and men reach age 71. The recommended vitamin D intake is 400-800 IU a day for most adults under age 50, and 800-1,000 IU a day for those 50 and up.
Diet can also play a role in migraine. Research shows that certain foods can trigger a migraine episode, including chocolate and aged cheeses, so it’s best to avoid those. Keeping a migraine diary to record details around each attack can help you pinpoint your personal migraine triggers.
Maintain a Healthy Weight
Research shows that obesity can increase both the prevalence of migraine and the frequency of migraine attacks. However, a meta-analysis published in 2017 found that association drops after the age of 50.
Meanwhile, that same meta-analysis found that those who are underweight may have an increased risk of migraine compared to those at a normal weight. And being underweight is known to weaken bone health and increase your risk of osteoporosis.
Aim for a BMI between 18.5 – 24.9 to lower your risk of migraine attacks and osteoporosis.
Quit Smoking
Smoking can contribute to weakened bones and increase fracture risk. What’s more, many people who smoke also partake in other habits that affect bone health, like decreased activity levels and poor diet.
Meanwhile, smoking can lead to nicotine headaches. Nicotine, the addictive ingredient in cigarettes, can increase sensitivity of your brain’s pain receptors and decrease blood flow to your brain, which can contribute to headaches. Nicotine can also reduce the effectiveness of pain relievers used to help alleviate headache pain. Research also shows that smoking can trigger a migraine attack.
Quitting smoking is one of the best things you can do for your health. Findings from one study show that quitting may help increase bone mass previously lost due to smoking. Ask your doctor if you need help with quitting. You may benefit from the use of a smoking cessation aid
Limit Alcohol Intake
Research shows that chronic, excessive alcohol consumption increases osteoporosis risk, including a decrease in bone density and weakened bones. What’s more, excessive alcohol consumption has also been linked to other unhealthy habits that impact bone health, including smoking and poor eating habits.
Alcohol causes dehydration and can trigger migraine attacks just like not drinking enough water.
If you do drink, be sure to so in moderation: That means one drink a day for women, and two for men. And choose your alcoholic beverage wisely.
When to Talk to Your Doctor About Bone Health
There are often no symptoms of osteoporosis until a bone breaks. “We really want to avoid that,” says Brandes. That’s why routine screening is recommended.
Osteoporosis screening is easy and only takes five to 10 minutes. Early detection can help you take proper steps to prevent fractures and keep bones healthy.
Routine screening for osteoporosis should be done:
- After age 65 for women, 70 for men, or sooner depending on your personal risk factors
- Every one to two years, or more often depending on your health
- After a bone fracture in those over age 50
- When taking a new medication associate with low bone mass or bone loss
Talk to your doctor at your next health exam about getting screened for osteoporosis.
This article was made possible with support from Amgen.
If you enjoyed reading this article, you’ll love what our video has to offer.
Evaluation of Bone Health/Bone Density Testing. Bone Health and Osteoporosis Foundation. https://www.bonehealthandosteoporosis.org/patients/diagnosis-information/bone-density-examtesting/.
Exercise for Your Bone Health. National Osteoporosis and Related Bone Diseases National Resource Center. https://www.bones.nih.gov/health-info/bone/bone-health/exercise/exercise-your-bone-health.
Gelaye B, et al. Body composition status and the risk of migraine: A meta-analysis. Neurology. May 2017. doi: https://doi.org/10.1212/WNL.0000000000003919.
Healthy Eating Plan. National Heart, Lung and Blood Institute. https://www.nhlbi.nih.gov/health/educational/lose_wt/eat/calories.htm.
Interview with Jan Lewis Brandes, MD, MS, Vice President of the National Headache Foundation.
Ji, MX, et al. “Primary Osteoporosis in Postmenopausal Women.” Chronic Diseases and Translational Medicine. March 2015. doi: https://doi.org/10.1016/j.cdtm.2015.02.006.
Kacena, M, et al. “No Pain, No Gain: Will Migraine Therapies Increase Bone Loss and Impair Fracture Healing?” EBioMedicine. October 2020. doi: https://doi.org/10.1016/j.ebiom.2020.103025.
Kristoffersen, ES, et al. Migraine, obesity and body fat distribution – a population-based study. The Journal of Headache and Pain. 2020. doi: https://doi.org/10.1186/s10194-020-01163-w.
Reddy, N, et al. The complex relationship between estrogen and migraines: a scoping review. BMC. 2021. doi: https://doi.org/10.1186/s13643-021-01618-4.
Rozen, T. “Migraine Headache: Immunosuppressant Therapy.” Current Treatment Options in Neurology. September 2002. doi: https://doi.org/10.1007/s11940-002-0050-0.
Side Effects of Bisphosphonates (Alendronate, Ibandronate, Risedronate and Zoledronic Acid). Bone Health and Osteoporosis Foundation. https://www.bonehealthandosteoporosis.org/patients/treatment/medicationadherence/side-effects-of-bisphosphonates-alendronate-ibandronate-risedronate-and-zoledronic-acid/.
When (and Why) Should I Start Screening for Osteoporosis? The Cleveland Clinic. https://health.clevelandclinic.org/when-and-why-should-i-start-screening-for-osteoporosis/.
Wu, CH, et al. Increased migraine risk in osteoporosis patients: a nationwide population-based study. SpringerPlus. 2016. doi: https://doi.org/10.1186/s40064-016-3090-8.
Zaeem, Z, et al Headaches: a Review of the Role of Dietary Factors. Curr Neurology and Neuroscience Reports. 2016. doi: https://doi.org/10.1007/s11910-016-0702-1.