For people with ankylosing spondylitis, a type of inflammatory arthritis that affects the spine, chronic back pain is all too familiar. Pain in the lower back, pelvis, and buttocks are hallmark symptom of AS, though the disease can affect your entire body.
Once you’re diagnosed — which research shows can take up to a decade or more after you start experiencing AS symptoms — your doctor will likely start you on a medication regimen that may include NSAIDs (non-steroidal anti-inflammatory drugs), progressing to disease-modifying drugs or biologics like TNF blockers that help control the disease’s symptoms and progression.
“The most important thing to do is to get established with a rheumatologist, a doctor who is specially trained to treat people who have ankylosing spondylitis,” says Grace Hsiao-Wei Lo, MD, assistant professor of medicine in the section of Immunology, Allergy and Rheumatology at Baylor College of Medicine in Houston, Texas. “There are good medications that can dramatically improve the quality of life for people who have AS.”
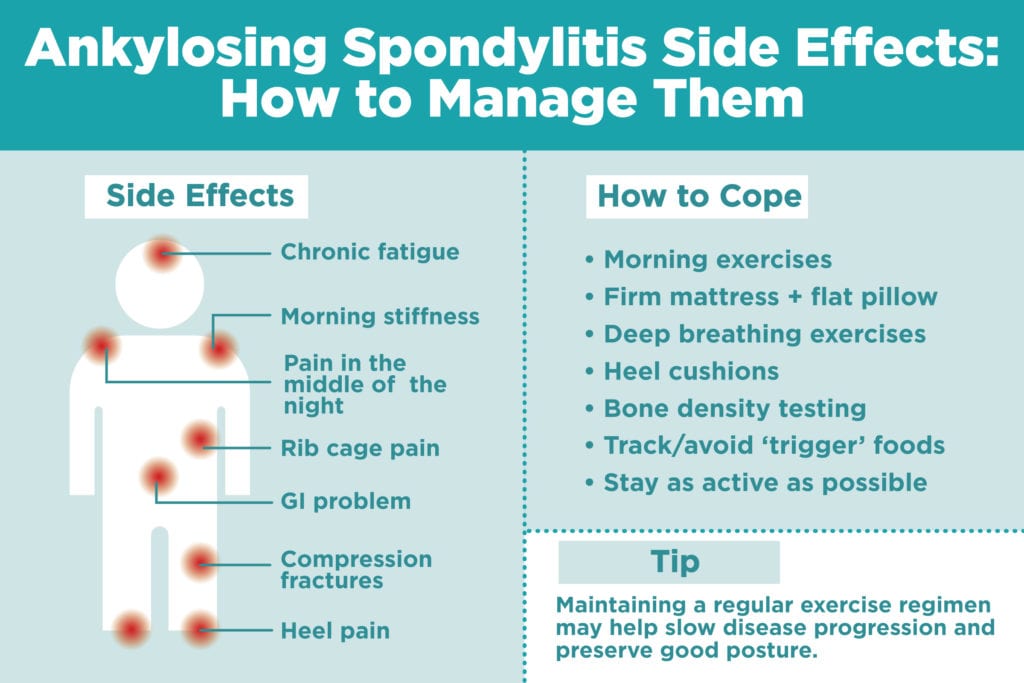
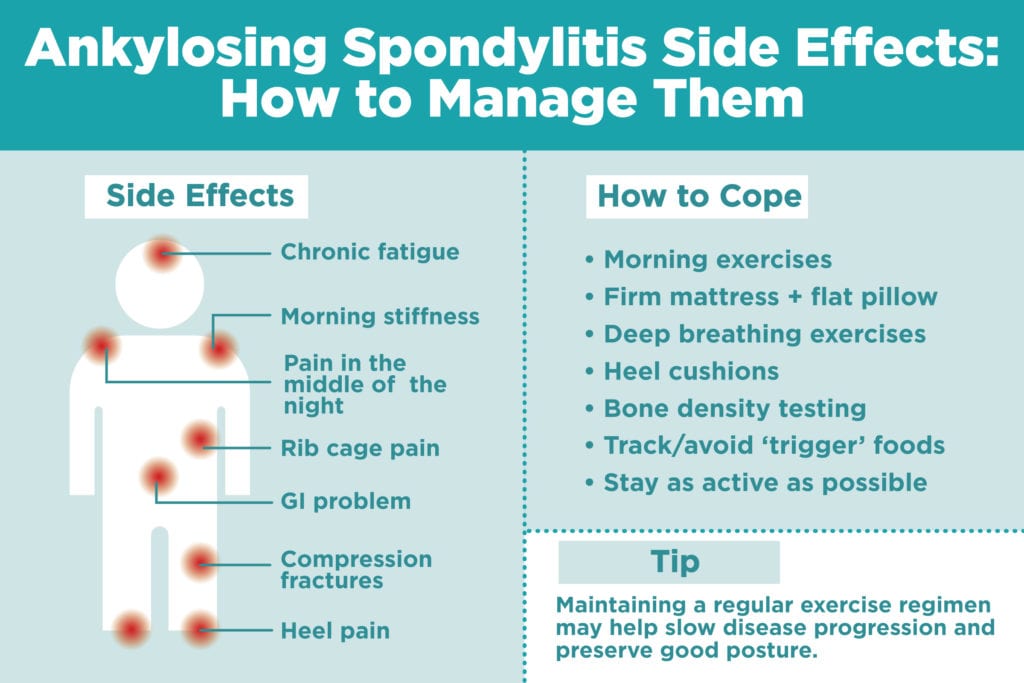
But once you are on appropriate AS medications, there are also lifestyle changes you can make at home to help prevent, manage and treat the symptoms and side effects of AS before they become even more debilitating. Here’s how to deal with each one.
1. Morning stiffness
You know the feeling: Your eyes flutter open, and the first thing you feel is stiffness throughout your body, making it hard to even get out of bed. “One of the hallmarks of morning stiffness with AS is that it gets better with exercise, so doing exercises can be helpful,” Dr. Lo says. “It is important to work on both flexion, as in bending to touch your toes, and extension, as in putting your hands on your hips and leaning back, exercises on a daily basis.” Here are six daily stretches for AS you can try.
If you’re too stiff to exercise first thing in the morning, move around a bit to loosen up first, and do your exercises in the middle of the day. In addition, “it is helpful to get specific instruction on these exercises from a physical therapist,” Dr. Lo says.
Maintaining a regular exercise regimen may help slow disease progression and preserve good posture.
2. Pain in the middle of the night
Pain that wakes you up in the second half of the night is common among people with AS; lying still for too long contributes to painful inflammation and stiffness.
If you’re having trouble sleeping, make sure you have a firm mattress and a pillow that’s flat (or no pillow at all).
In addition, “people like using heating pads because it is comforting,” says Karmela Chan, MD, a rheumatologist at Hospital for Special Surgery in New York City. Exercise may also improve nighttime sleep, she says. Plus, you may want to talk to your rheumatologist about your medications to make sure they’re providing you with the relief you need to get a good night’s sleep.
3. Rib cage pain
As ankylosing spondylitis progresses, the bones of the spine and rib cage can fuse together, which can lead to pain when you breathe. “Decreased motion of the spine and the chest wall restricts how much the lungs can expand, causing restrictive pulmonary disease,” Dr. Lo says.
Deep breathing exercises can help maintain the chest expansion of your rib cage to prevent this fusion — if it gets worse, a respiratory specialist can help you learn how to breathe through your diaphragm. And, of course, keep taking your meds to slow this progression. “Sometimes patients will have to try more than one anti-inflammatory to see which one works best for them,” Dr. Chan says.
4. Chronic fatigue
Let’s face it: It can be hard to feel like exercising when you’re tired all the time. Dr. Lo advises checking in with your doctor if your fatigue is becoming problematic. “One reason that there is fatigue in AS because AS is an inflammatory problem; treating the underlying problem with medications can sometimes help with the fatigue,” she says. “Additionally, sometimes people can become anemic if they have an ongoing inflammatory problem, so again, it is important to discuss this problem with your rheumatologists and check some basic blood tests.” In addition, don’t push yourself too hard throughout your day. These tips for dealing with fatigue in inflammatory arthritis can help too.
5. Neck stiffness
AS can affect your entire trunk, all the way up to your neck. You want to try to preserve that range of motion using stretching exercises, so you maintain the ability to turn your head. “Working on flexion, extension, as in nodding, lateral rotation, as in shaking your head, and lateral flexion exercises, tilting your head side to side, can be helpful,” Dr. Lo says. Dr. Chan agrees: “The more exercise patients engage in, the less stiff they will be.”
Make sure you don’t slump over at your work space, which can also contribute to stiffness and poor posture.
6. Eye inflammation
Unfortunately, the National Institutes of Health reports that ankylosing spondylitis affects the eyes in up to 40 percent of patients. “AS can cause something called acute anterior uveitis — it usually manifests as a painful red eye. You might have some blurry vision with it, light can be bothersome, and some people can even have headaches,” Chan says. “You need to see an ophthalmologist right away if this happens — and if you don’t have an ophthalmologist, your rheumatologist might be able to help you get to an ophthalmologist ASAP.”
To prevent vision loss or other complications, your eye doctor should give you prescription eyedrops to treat the inflammation. Read more about uveitis symptoms and treatment here.
7. Heel pain
“Patients with AS can have Achilles tendonitis and plantar fasciitis, which can be very uncomfortable,” Dr. Chan says. Plantar fasciitis, an inflammation of connective tissue at the base of the heel, is very common in people with inflammatory arthritis.
Wear supportive, soft-soled shoes (luckily, there are tons of cool sneaker options) and special heel cushions. Although it may hurt to walk, exercise is once again an important treatment — but you don’t have to go it alone. “Physical therapy can be very helpful,” Dr. Chan says, so reach out to a professional for help. Here are more tips for managing arthritis foot pain.
8. Compression fractures
With ankylosing spondylitis disease progression, spinal fractures become more likely. “In AS, the spine can eventually become ankylosed, which means the bones that make up the spine become fused. Instead of acting as many bones that allow bending of the neck and back, eventually, they just act as one bone,” Dr. Lo says. “Once ankylosis has occurred, then sudden movements that previously were easy can then lead to fracture because there is much less mobility in the spine.” People with AS also tend to have weak bones that make them fracture even more easily, so talk to your doctor about having a bone density test. You also want to make sure you’re getting enough calcium and vitamin D for bone health.
If you’re having surgery for an unrelated problem to your ankylosing spondylitis, Dr. Lo notes it’s important to tell your surgeon that you have AS, particularly if it affects your neck, to prevent fractures. “When the anesthesiologist tries to put the tube down the throat of a person with AS who has neck involvement, this can lead to a fracture of the neck and this can be life threatening,” she says. “It is important to inform the anesthesiologist when a patient with AS has an elective or emergent surgery to avoid the sudden movement of the neck that is usually needed to protect the airway.”
9. Intestinal issues
The inflammation that causes AS can also affect the gut. Studies show up to 10 percent of people with AS also have inflammatory bowel disease (IBD). “Ankylosing spondylitis is an autoimmune disease, and there are some autoimmune diseases that also affect the intestinal tract, for example Crohn’s disease or ulcerative colitis,” Dr. Lo says. “In this case, it is critical to get diagnosed properly by a gastroenterologist.” Many of the medications used to treat ankylosing spondylitis overlap with those used to treat inflammatory bowel disease, she says; but you should talk to your doctor if you’re on NSAIDs to manage AS pain, which can worsen IBD.
“It is important to also make sure that your rheumatologist and gastroenterologist are in communication with one another, and that collective decisions are made to best treat a given patient,” Dr. Lo says. Although there’s no one diet that has been proven to help AS or IBD, talk to your doctor or a registered dietitian to help determine if there are any “trigger” foods for you. Eating a well-rounded, Mediterranean-style diet with lots of fruits and veggies, whole grains, beans and legumes, and fish may help promote maintaining a healthy weight and may reduce inflammation as well.
10. Heart problems
Although this is more rare, AS can take its toll on the cardiovascular system. “We think of chronic inflammation as a risk for developing coronary artery disease,” Dr. Chan says. Dr. Lo says there is also an increased risk for aortic regurgitation (a leaky aortic valve).
Talk to your doctor to discuss how the medications you take could affect your risk; an in addition, practice good heart health habits. “Take care to alter the risk factors that are within your control, such as weight, smoking, diet, and exercise,” Dr. Chan says.
Keep Reading
- 6 Stretches for Ankylosing Spondylitis You Should Do Every Day
- Seeing a Rheumatologist for Ankylosing Spondylitis: What to Know Before Your First Visit
- VIDEO: Ankylosing Spondylitis: Misconceptions and Delays in Diagnosis





