Back pain of any kind can be frustrating and debilitating, and figuring out what’s causing the back pain isn’t always easy. Part of the challenge is that some back-related conditions, like ankylosing spondylitis and sciatica, share some symptoms in common.
Online tools like PainSpot — which can help you determine what might be causing your pain by asking a series of questions that helps differentiate different types of pain from each other — might help you narrow down potential back pain conditions, but ultimately you’ll need to see a doctor. This is especially important if you suspect you could have a type of inflammatory back pain like ankylosing spondylitis, which can be progressive and often requires different treatment from other common causes of back pain, like sciatica.
“Not all back pain is created equal,” explains Stuart D. Kaplan, MD, Chief of Rheumatology at Mount Sinai South Nassau and a partner at Rheumatology Consultants, LLP. “There are different types of back pain that are very different in their etiology [cause] and in their treatment.” It’s important to try to diagnose and treat back pain properly as soon as possible to avoid unnecessary pain and disability, as well as other long-term complications.
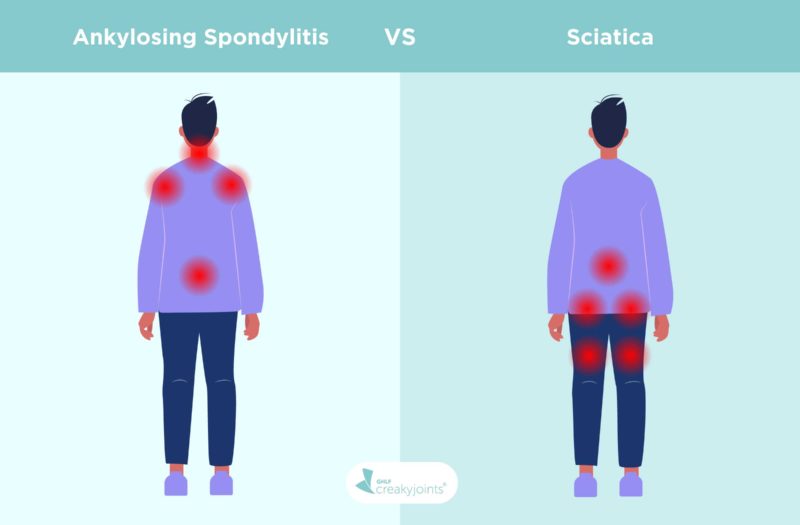
If you’re wondering whether your back pain could be from inflammatory arthritis like ankylosing spondylitis or from sciatica, one way to start narrowing things down is to consider the type of pain you’re experiencing. Sciatic pain is often described as a shooting or burning pain that moves down your leg. It’s also fairly common. According to the Cleveland Clinic, around two in five U.S. adults experience sciatica at some point in their lifetime. Ankylosing spondylitis pain, however, often makes your lower back and pelvis feel achy and stiff. It’s an inflammatory form of arthritis that can also affect joints beyond your lower back, so if you’re also experiencing pain and stiffness in other places — such as the neck, shoulders, hips, ribcage, or feet — that may be something to consider.
If either of these types of pain sound familiar, read on to learn more about other differences between ankylosing spondylitis and sciatica, including how these conditions are diagnosed and treated.
Ankylosing Spondylitis vs. Sciatica
If you suspect you might be dealing with either ankylosing spondylitis or sciatica, you can learn more about the symptoms of each, the key differences, the treatments, the outlook, and the risk factors.
Ankylosing spondylitis (AS) is a form of arthritis that falls under the umbrella of axial spondyloarthritis (axSpA), which is an inflammatory form of arthritis that is associated with chronic lower back pain. Ankylosing spondylitis results from having an over-active immune system that causes inflammation of the spinal vertebrae, which tends to result in back and neck pain. It may also cause pain and stiffness in other joints, like your hips, shoulders, and feet. AS can cause bony growths on the spine. Over time, these growths can cause parts of the spine to fuse together, which limits mobility. Although ankylosing spondylitis can affect people of any sex, Dr. Kaplan notes that it is slightly more common in men than in women.
Sciatica can also cause back pain, but in a very different way than ankylosing spondylitis. Sciatica is nerve pain from damage or irritation to the sciatic nerve, which branches from the lower back through the hips and buttocks and down through the legs. According to the Cleveland Clinic, the sciatic nerve is the longest and thickest nerve in the body, made up of five nerve roots. Samar Gupta, MD, FACR, a rheumatologist at Michigan Medicine, explains that sciatica can often be attributed to an inciting injury. “One example would be somebody picking up a heavy weight, and the posture not being right. It’s a mechanical issue, not an inflammatory disease,” he says.
When it comes to back pain, mechanical issues are anything that disrupts how the components of your back fit together and move. Some examples include throwing out your back while lifting something heavy or pulling a muscle while exercising. An inflammatory disease, on the other hand, is when your immune system is mistakenly attacking the joints — in the case of ankylosing spondylitis, the immune system is attacking the joints of your spine.
Another different between ankylosing spondylitis and sciatica: AS pain is chronic; once it starts, it may ebb and flow but never really go away. Doctors become more suspicious of AS when you’ve had back pain that came on gradually and has lasted for at least three months. Sciatica pain often goes away with treatment.
Do You Have Ankylosing Spondylitis or Sciatica?
Although ankylosing spondylitis and sciatica both present as back pain for many people, there are other distinct symptoms associated with each. Determining which set of symptoms you’re experiencing may give you a better idea of which ailment you’re dealing with, though of course, you’ll need to consult a doctor to get an official diagnosis.
The type of pain you feel is likely a clue as to what condition you’re dealing with. Ankylosing spondylitis pain tends to be duller and makes you feel stiff around the lower back and hips. Pain from sciatica is often a sharp, shooting pain that radiates down one side of your buttocks and leg.
The back pain and other symptoms caused by AS tend to have some subtle but unique traits and characteristics. Some of the more common ankylosing spondylitis symptoms include:
- Pain and stiffness in the lower back and hips
- Pain and stiffness in other joints, such as your neck, shoulders, or feet
- Pain between the base of your spine and your pelvis
- Pain that is worse in the morning that gets better as you move around
- Pain that improves after a hot shower
- Alternating buttock pain
- Difficulty breathing
- Fatigue
- Loss of appetite
- Abdominal pain, diarrhea, and other GI symptoms
- Skin rash
- Uveitis (eye inflammation)
Sciatica symptoms include:
- Sharp, burning pain that radiates from your lower spine down through your buttocks and the back of your leg, usually only on one side.
- Pain that is more felt in your lower leg compared to your lower back
- Pain that worsens when you cough or sneeze
- Pain that gets worse as the day goes on
- Numbness, tingling, or muscle weakness in the affected leg
- Difficulty controlling your bowels or bladder (if this is the case, you should seek immediate medical care)
One important distinction that can help you determine what you’re dealing with is the onset of the pain: Did it come on quickly, or has it slowly gotten worse over time?
Dr. Gupta notes that with sciatica, there tends to be a clear incident that triggered the pain. “[A person with sciatica may have] twisted their back, or bent in the wrong way,” he says. “Sciatica is very acute, like they were fine yesterday and today they’re feeling horrible. But ankylosing spondylitis comes on insidiously, they kind of have this little backache; now it’s getting worse.”
Does Ankylosing Spondylitis Cause Sciatica?
Although both conditions can cause back pain, one ailment doesn’t really cause the other one to occur, except in very unusual cases.
“Ankylosing spondylitis causing sciatica is not impossible, but it’s a very rare occurrence,” explains Dr. Gupta. “The vice versa is not true — sciatica doesn’t cause ankylosing spondylitis.”
He notes that sacroiliitis — inflammation of the sacroiliac joint, which is where the spine connects with the pelvis and is a common feature of ankylosing spondylitis — causing symptoms of sciatica have been reported in a handful of cases.
There isn’t necessarily any specific cause of ankylosing spondylitis, though genes are thought to play a role. There is one known genetic marker in particular, called the HLA-B27 gene, that is associated with an increased risk of ankylosing spondylitis. (However, you can also have AS without having this gene.)
Research suggests that AS can be triggered by something in your environment, such as an infection. As with other inflammatory conditions, AS is likely caused by a combination of genetic and environmental factors.
Understanding Sciatica
How Common is Sciatica?
Sciatica is a fairly common condition. According to the Cleveland Clinic, about 40 percent of U.S. adults experience sciatica sometime in their life. Some people, however, are more at risk of experiencing sciatic pain because of their lifestyle and other health conditions.
Outlook for Sciatica
Although sciatica can cause intense pain, it isn’t necessarily something that requires serious medical intervention. Dr. Gupta says the majority of sciatica cases resolve within 90 days. That said, Dr. Gupta also notes the importance of seeing a doctor if you suspect you could have sciatica, as it can cause permanent nerve damage if left untreated.
“If the back pain is the more prominent feature and if it is not improving with more conservative measures, go see a doctor,” he says. “And then consider a rheumatology referral to make sure there is nothing happening beyond run-of-the-mill sciatica.”
Risk Factors for Sciatica
There are certain medical conditions and lifestyle habits that increase your risk for developing sciatica.
- Previous Injury: Having a slipped disk in your back can cause pressure on the sciatic nerve. Similarly, other back injuries can cause you to develop sciatica.
- Weight: People who are overweight can also be at risk for sciatica because of the stress put on the spine.
- Job: There’s reason to believe that a labor-intensive job that requires you to twist your back or carry heavy loads might increase your risk for sciatica. That said, the Mayo Clinic also notes that there isn’t conclusive evidence of this link.
- Diabetes: Having diabetes increases your risk of nerve damage, which can make it more likely for you to have sciatica.
- Osteoarthritis: According to the Cleveland Clinic, as osteoarthritis breaks down the cartilage that cushions your bones, your body can grow bone spurs to try and repair the loss. It’s possible for these bone spurs to form in your spine and press on your sciatic nerve.
- Weak core: Having well-developed back and core muscles helps support the spine, which in turn decreases your risk for sciatica.
- Age: Age-related changes in the spine can be a common cause for sciatica, according to the Mayo Clinic.
- Smoking: Nicotine can damage spinal tissue and weaken bones, meaning people who smoke may be more likely to develop sciatica.
How Sciatica Is Diagnosed
If you suspect you may have sciatica, the best thing to do is to see a health care provider. They may do a physical assessment, which could include:
- Walking: You may be asked to walk on your toes or heels to see if the pain worsens, which can indicate sciatica.
- Straight Leg Test: According to the University of Maryland School of Medicine, the straight leg raise test can be used to help determine if someone has sciatica. If your doctor asks you to do this, you’ll lie with one leg down, while the other leg is kept straight up and raised by the examiner. If raising the leg between 30 and 70 degrees causes pain to occur and radiate down the leg, that can indicate that you may have sciatica. Your health care provider may also perform this test with you sitting down and stretching the sciatic nerve by extending the knee. If you feel pain that radiates to below the knee, this could be a sign of sciatica.
In some cases, such as instances where sciatica doesn’t resolve within a normal timeframe, your doctor may order additional tests. These could include:
- Spinal X-rays: If your sciatica pain doesn’t lessen after a certain amount of time, your doctor may order X-rays to see if there are bone spurs that are pressing on a nerve.
- MRI: Similarly, your doctor may have you do an MRI to get a detailed image of your bone and soft tissues, which can allow them to see things like herniated disks.
- Electromyography (EMG): Your health care provider may want you to get this test, which measures electrical impulses produced by the nerves and responses of your muscles. With regards to sciatica, it can confirm nerve compression caused by things like herniated disks.
- Myelogram: This test involves a dye being injected into your spinal canal through your lower back. It allows for the doctor to get a clear look at whether there is anything pressing against your nerves or spinal cord.
How Sciatica Is Treated
If your health care provider diagnoses you with sciatica, there are a number of treatment options they may recommend.
- Ice/Heat therapy: The Mayo Clinic recommends applying an ice pack to the painful areas for about 20 minutes multiple times throughout the day. After a few days of this, you can try using a heating pad on the lowest setting. You can try alternating warm and cold packs to see if this provides any relief.
- Physical therapy: Your health practitioner may recommend physical therapy to treat your sciatic pain. A physical therapist can perform and teach gentle stretches or exercises that will help build your core strength, which can help relieve your sciatic pain. They may also recommend light exercise, like walking or swimming.
- Medications: Some of the medications used to treat sciatica can include muscle relaxants, anti-inflammatory drugs, or painkillers, according to Dr. Kaplan.
- Spinal injections: It’s possible that your doctor might recommend getting epidural injections of a corticosteroid medication in the area around the nerve root that is causing you trouble. This can help suppress inflammation around the irritated nerve and reduce pain.
- Surgery: In severe cases, your doctor may consider surgery to treat sciatica. A severe case would be if you experience loss of bladder or bowel control or significant weakness, or if no other therapy/treatment has improved your condition. A surgeon may be able to remove the bone spur or portion of the disk that’s causing pain, but as Dr. Kaplan notes, surgery is a last resort.
Understanding Ankylosing Spondylitis
How Common Is Ankylosing Spondylitis?
Estimates vary depending on which studies you look at, but AS is not as rare as you might think. According to the Spondylitis Association of America, spondyloarthritis (which includes ankylosing spondylitis as well as other forms of arthritis) affects 3.2 million Americans, or about one in 100. And these numbers may be an underestimate, since AS tends to be misdiagnosed or people experience significant delays in getting a proper diagnosis.
Risk Factors for Ankylosing Spondylitis
There isn’t one specific cause of ankylosing spondylitis, but there are some groups who are more at risk for developing the disease than others.
- Sex: Ankylosing spondylitis has historically been considered a disease that predominantly affects men. However, more recent data suggests that while AS is more commonly diagnosed in males than in females, it does affect females and is more evenly distributed among the sexes than previously thought.
- Age: Symptoms of ankylosing spondylitis usually begin between before age 45 and commonly start in the teens, twenties, and thirties.
- Family history: People who have the HLA-B27 gene in their family are at greater risk of developing ankylosing spondylitis. That said, it is possible for people who don’t have this gene to develop the disease. And on the flip side, people who do carry the gene don’t always develop ankylosing spondylitis.
How Ankylosing Spondylitis Is Diagnosed
If you are concerned that your back pain might be caused by ankylosing spondylitis, you should see a doctor. You may need to start with a general practitioner for initial testing, who would likely refer you to a rheumatologist, which is a doctor who treats musculoskeletal disease and systemic autoimmune conditions. There are several things that your health care provider might do in order to diagnose you with ankylosing spondylitis.
- A physical exam. The doctor will look for signs of spine fusion, inflammation, and limited range of motion in your spine and your other joints.
- Image testing. Your rheumatologist may order imaging tests, such as X-rays and MRIs, to get a better look at what’s happening with your spine as well as your other joints.
- Assess personal and family medical history. Your health care provider will likely ask you some questions about your own medical history as well as your family history. They will ask about the nature of your back pain and other symptoms: when they started, what makes them feel worse or better, etc.
- Blood work. A doctor may order blood tests to get more information about whether you are at risk of developing ankylosing spondylitis. These may include testing for the HLA-B27 genetic marker and looking for elevated levels of inflammation in the blood — erythrocyte sedimentation rate (ESR, or sed rate) or C-reactive protein (CRP).
Read more here about how ankylosing spondylitis is diagnosed.
Outlook for Ankylosing Spondylitis
Ankylosing spondylitis can cause pain that can be debilitating and have a big impact on patients’ sleep, mood, ability to work, and overall quality of life. It is not a life-threatening condition.
“The outlook for AS is very good if addressed early in the disease course,” Brett Smith, DO, rheumatologist with Blount Memorial Physicians Group in Alcoa, Tennessee, previously told CreakyJoints. “With appropriate comprehensive treatment, including physical therapy and exercise, NSAIDs, and biologics, many people have preserved function and minimal pain.”
That being said, some of the comorbidities associated with AS can be concerning. People with AS may be more likely to develop certain heart problems and osteoporosis. They may also be at risk for other inflammation-related conditions, such as inflammatory bowel disease (IBD), psoriasis, and uveitis (eye inflammation), as well as mental health conditions like depression.
How Ankylosing Spondylitis Is Treated
There’s no cure for ankylosing spondylitis, but there are different types of medication that can help relieve symptoms, reduce inflammation, and possibly slow the progression of the disease. Treatment for AS may include:
- NSAIDS. Short for nonsteroidal anti-inflammatory drugs, these are considered first-line treatments for AS. Medications in this category include over-the-counter drugs such as ibuprofen or naproxen, as well as prescription versions of NSAIDs. If they don’t work well enough to reduce AS symptoms, then doctors typically recommend advanced therapies, such as biologic drugs.
- Biologics. Biologics are medications (given by injection or IV infusion) that target specific parts of your immune system to reduce inflammation.
- Steroids. Corticosteroids are not recommended for long-term use because they can cause many different side effects, but they are sometimes recommended to help manage painful flares, or periods of increased disease activity.
- Exercise regularly and attend physical therapy. In addition to following a treatment plan from your doctor, regular exercise and physical therapy can help you manage pain from ankylosing spondylitis. If you experience stiffness and pain in the morning, doing flexibility and range-of-motion exercises when you wake up may help. You can also try deep-breathing exercises, balance exercises, and aquatic exercises.
- Get enough sleep. Getting a good night’s rest can help you manage your AS symptoms. However, pain from AS can make it very challenging to get high-quality sleep; many people with AS report “painsomnia” that interrupts their sleep. Make sure to tell your doctor if you are having difficulty sleeping. You may need adjustments to your medication regimen or try complementary practices, like meditation, to help improve your sleep.
Track Your Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain.
Back pain: What you can expect from steroid injections. Harvard Health. August 16, 2020. https://www.health.harvard.edu/pain/back-pain-what-you-can-expect-from-steroid-injections.
Interview with Samar Gupta, MD, FACR, a rheumatologist at Michigan Medicine
Interview with Stuart Kaplan, MD, Chief of Rheumatology at Mount Sinai South Nassau and a partner at Rheumatology Consultants, LLP
Performing Straight Leg Raise Test for Sciatica. University of Maryland School of Medicine. Department of Emergency Medicine. June 29, 20201. https://umem.org/educational_pearls/1582/.
Sciatica. Cleveland Clinic. March 25, 2020. https://my.clevelandclinic.org/health/diseases/12792-sciatica.
Sciatica. Mayo Clinic. August 1, 2020. https://www.mayoclinic.org/diseases-conditions/sciatica/symptoms-causes/syc-20377435
Spondy What? Spondylitis Association of America. https://spondylitis.org/.