Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
If you’re immunocompromised, you can now get a third dose of an mRNA COVID-19 vaccine (Pfizer or Moderna) in the United States, thanks to a recent important change in recommendation from the U.S. Centers for Disease Control and Prevention (CDC).
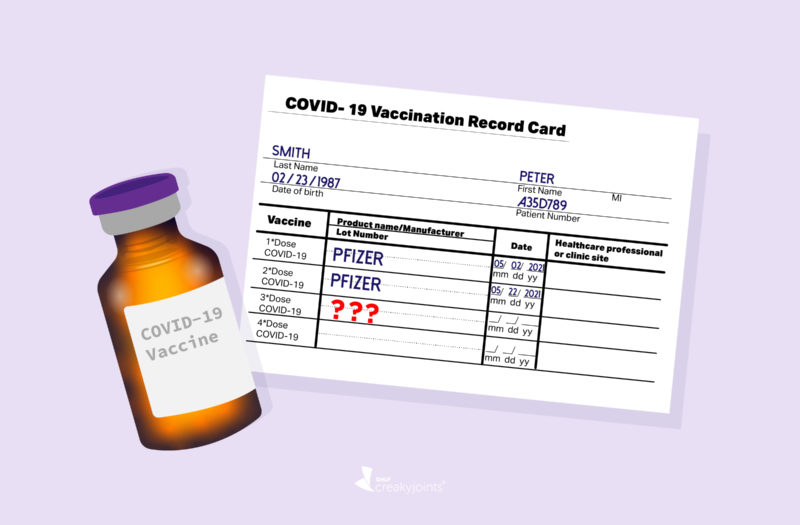
The main takeaway: People who are immunocompromised and received a two-dose mRNA COVID-19 vaccine (Pfizer or Moderna) can now get an additional third dose as part of the vaccine series. This applies to immunocompromised people 12 and older who received the Pfizer vaccine, and people 18 and older who received the Moderna vaccine. Right now, immunocompromised people who received the Johnson & Johnson vaccine cannot get an additional vaccine dose under these recommendations, though this may change as more research becomes available.
Many people in the CreakyJoints and Global Healthy Living Foundation (GHLF) community acted swiftly to get the third dose. In a recent poll of our GHLF COVID-19 Patient Support Program, which includes immunocompromised and high-risk patients, among 2,652 respondents, 53 percent said that they have already received the third dose. Among those who have not yet received it, 91 percent said they planned to.
Read more here about what it was like for those in our community who received the third COVID-19 vaccine dose.
We know there are many questions about who qualifies for an additional COVID-19 vaccine dose, which vaccine to get, what to expect with side effects, and more. Here are answers based on what we know so far — we will update this resource as more information becomes available.
Who Is Considered Immunocompromised and Should Get the Additional Vaccine Dose?
The CDC includes a list of medical conditions and treatments that it considers “moderately and severely immunocompromised.” This includes people who have:
- Been receiving treatment for cancer (tumors or blood cancers)
- Received an organ transplant and are taking medication to suppress the immune system
- Received a stem cell transplant within the last two years or are taking medication to suppress the immune system
- Moderate or severe primary immunodeficiency (e.g., DiGeorge, Wiskott-Aldrich syndromes)
- Advanced or untreated HIV infection
- Active treatment with high-dose corticosteroids or other immunosuppressant or medications, including therapies such as methotrexate, rituximab, mycophenolate, and certain biologic medications
People with inflammatory and autoimmune conditions often take many different medications that can be considered immunosuppressive or immunomodulatory (meaning, it has an effect on the way the immune system functions).
Researchers have been studying how different types of immunosuppressive medications affect the immune response to the COVID-19 vaccine, and studies show that the response can vary widely by type of medication. For example, the treatment rituximab (Rituxan) — used for rheumatoid arthritis and certain other rheumatic conditions — has a significant impact on the immune response. Methotrexate, mycophenolate, and high-dose corticosteroids also diminish the immune response. But other biologics don’t seem to have as much of an effect.
That said, the American College of Rheumatology recommends that rheumatology patients on immunosuppressive and immunomodulating therapies get the third vaccine dose.
It is not recommended to get antibody testing to see how you may have responded to the previous doses of the vaccine. Ask your doctor if you have any questions about whether your medications or medical conditions make you eligible for an additional vaccine dose.
The CDC said it is not necessary to show proof of your medications or medical condition to get the third COVID-19 vaccine dose. Additional screening questions will be asked at the vaccination site to make sure you have an immunocompromising condition or treatment.
Why Is a Third Dose Needed for the Immunocompromised?
The CDC made this change in the vaccine regimen for immunocompromised people for three main reasons:
- They are more likely to get severely sick from COVID-19 (though risks and complications can vary widely — remember, being “immunocompromised” is a very broad definition)
- They are likely to have a reduced antibody levels from the original COVID-19 vaccine series compared to non-immunocompromised people
- They may be more likely to transmit the virus to others
Immunocompromised patients are more likely to have breakthrough infections and complications from those breakthrough infections. Research shows that about 40 to 44 percent of hospitalized breakthrough cases in the U.S. are in immunocompromised people, according to CDC data.
The studies that have looked at antibody levels in people who have received two doses of the Pfizer or Moderna vaccine have shown varying results based on the type of immunocompromising condition. For example, people taking medication after an organ transplant to prevent rejection tend to have a much lower antibody response than people taking other immunosuppressive therapies, say, for autoimmune conditions. But on the whole, studies show that vaccine effectiveness in immunocompromised people after receiving the second dose ranges from 59 to 72 percent, compared with 90 to 94 percent in people who are not immunocompromised.
The good news is that recent research has shown that a third vaccine dose can help boost the immune response. In a study recently published in the New England Journal of Medicine, organ transplant recipients were randomized to get a third dose of the Moderna COVID-19 vaccine two months after their second dose or a placebo. More than half (55 percent) of those who got the additional dose had a robust antibody response one month later compared to only 18 percent in the placebo group.
A separate study from France, 101 organ transplant patients received a third dose of the Pfizer COVID-19 vaccine. The proportion of people with antibodies increased from 40 percent before the third dose to 68 percent four weeks later.
In summarizing the research available so far, the CDC says that among immunocompromised people who had no detectable antibody response to the original two-dose vaccine from Pfizer or Moderna, 33 to 50 percent developed a response after a third dose.
However, keep in mind that a third dose is not a bulletproof shield against COVID-19 and your response will depend on your medical condition and medications. It’s important to still follow precautions like wearing a mask indoors and avoiding crowds (more on this below).
A Third COVID-19 Vaccine Dose vs. a Booster Shot: What’s the Difference?
The additional third dose for the Pfizer and Moderna vaccines that is now recommended for immunocompromised people is NOT the same as a booster shot, and it’s important to understand the distinction.
Additional or Third Dose
An additional dose of a vaccine is given when the initial immune response following a primary vaccine series is likely to be insufficient. Different studies in various groups of immunocompromised patients (from organ transplant recipients to people with autoimmune conditions) have shown that that immunocompromised people have a slightly lower antibody response to the COVID-19 vaccine, which means they are not as protected against COVID-19 as the general population.
The CDC emphasized that the additional dose is now part of the usual COVID-19 vaccination regimen for severely immunocompromised people.
Booster Dose
A booster shot, on the other hand, is given when an initial sufficient immune response to a primary vaccine series wanes over time. Also known as a durability booster, this would be available to the general population. It’s possible that immunocompromised patients could get both a third vaccine dose as part of the regular vaccine series and a booster dose in the future.
Though the CDC and FDA have yet to determine if and when booster shots will be recommended, they noted that COVID-19 vaccine booster shots would likely first be given to at-risk adult populations. This includes:
- Adults age 65 and older
- Long-term care facility residents
- Health care workers
Which Vaccines Will Be Given as Third COVID-19 Vaccine Doses?
As of now, the emergency use authorization for the additional dose only applies to people who received an mRNA vaccine, which includes:
- Pfizer (available to people ages 12 and older)
- Moderna (available to people 18 and older)
This means that if you are immunocompromised and received the Johnson & Johnson vaccine, it is not recommended that you get an additional dose of any other vaccine at this time. That’s because “there is not enough data at this time to determine whether immunocompromised people who received the Johnson & Johnson’s Janssen COVID-19 vaccine also have an improved antibody response following an additional dose of the same vaccine,” according to the CDC.
CDC and FDA officials indicated they are actively studying this issue and expect to have an update for people who receive the Johnson & Johnson vaccine soon. The J&J vaccine has been used far less than the Pfizer and Moderna vaccines, but it’s not known how many immunocompromised people are affected by this.
Does Your Third COVID-19 Vaccine Dose Have to Be the Same as Your First Two?
Ideally, yes. The CDC recommends that people try to match the version of their additional vaccine dose to their initial vaccine dose. (If you got Pfizer for your first two vaccines, you should get Pfizer for your third.) But if that’s not feasible, the CDC said mixing-and-matching the mRNA vaccines is permitted for the third dose.
Do You Need to Adjust Your Immunosuppressive Medication Regimen Around the Third Dose?
The American College of Rheumatology recently updated its COVID-19 vaccine guidance for getting the third dose and possibly temporarily stopping certain medications to help improve your immune system’s response to the vaccine. The main takeaways are:
Hold immunomodulating or immunosuppressive medications (except for glucocorticoids and most biologics) for 1-2 weeks after the third vaccine dose, assuming disease activity allows. Because holding these medications for a week or two should not put most patients at risk for a flare, experts recommend this to help your body mount a robust response to the vaccine
Discuss holding most biologics, including TNF inhibitors and interleukin inhibitors, with your doctor. The ACR task force assigned to updating the guidance was mixed about whether to advise for or against holding certain biologics. Data suggests that people on these medications do not have a dramatically reduced response to the COVID-19 vaccine. Some doctors may recommend you temporarily hold them out of an abundance of caution; maybe there’s a chance doing so could increase your response slightly. Others may recommend that you continue to take them because stopping them could impact your risk of a flare and there is unlikely to be a big impact on vaccine response.
Discuss timing around rituximab with your doctor. This medication gets rid of B cells circulating in your blood to reduce inflammation, but B cells are needed to generate an immune system response to vaccines. Because of this, experts recommend getting the third vaccine dose close to your NEXT rituximab dose (when B cells would be highest) in order to garner a better response to the vaccine.
You can read more here about the updated ACR COVID-19 vaccine guidance for people with autoimmune or inflammatory rheumatic disease.
Whether or not you should temporarily stop your medication depends on many factors, including how well-controlled your underlying condition is.
Don’t make any changes to your medication regimen before or after getting the third COVID-19 vaccine dose without first asking your doctor.
Will You Have Side Effects from the Third COVID-19 Vaccine Dose?
Initial studies suggest that side effects from the third dose will be similar to those from the first two doses. The CDC says that fatigue and pain at the injection site were the most commonly reported side effects, and overall, most symptoms were mild to moderate.
The CDC says there is “limited information about the risks of receiving an additional dose of vaccine, and the safety, efficacy, and benefit of additional doses of COVID-19 vaccine in immunocompromised people continues to be evaluated.”
The most common COVID-19 vaccine side effects, which have been reported to be more frequent and more severe following the second dose, include:
- Pain in the arm where you got the shot
- Swelling in the arm where you got the shot
- Fever
- Chills
- Fatigue
- Headache
So far, the side effects from the third COVID-19 vaccine dose have varied among immunocompromised patients.
CreakyJoints asked community members who received their additional dose what the experience was like. Rebecca G. said she “ran a fever, had body aches, and got a terrible headache with nausea,” while Krista K. said she “just generally felt yucky and very tired.”
It’s important to be aware of the risks of serious side effects, though these are rare.
Experts will be monitoring the rollout closely and the CDC’s vaccine monitoring app called V-safe will be amended so users can share information about symptoms and side effects after receiving the third dose.
In an Israeli survey of 4,500 people who received a third dose of the Pfizer vaccine, 88 percent of respondents said that in the days after receiving the third shot, they felt “similar or better” to how they felt after the second shot. Thirty-one percent reported experiencing some side effect; soreness at the injection site was most common, Reuters reported.
“I suspect that the side effects from the third dose will be very similar to those seen with earlier doses,” says infectious disease physician Amesh A. Adalja, MD, a Senior Scholar at Johns Hopkins Center for Health Security. “People should see what symptoms develop and have some acetaminophen or ibuprofen handy. They also may not want to schedule anything too strenuous the day after the vaccination.”
Where Do You Get the Third COVID-19 Vaccine Dose?
You should be able to get the third vaccine dose wherever other mRNA (Pfizer and Moderna) vaccines are available. The CDC recommends you:
- Search vaccines.gov
- Text your ZIP code to 438829
- Call 1-800-232-0233 to find locations near you
You can also contact your local pharmacy to see if vaccination walk-ins or appointments are available or contact your state or local health department for more information.
Though you will need to show proof of prior vaccination, the CDC notes that people will not be required to show proof of a medical condition in order to receive a third dose. They simply have to attest to their immunocompromised status.
Staying Safe and Continuing to Take Precautions
Though a third COVID-19 vaccine dose will likely help immunocompromised people garner more protection against the coronavirus, that doesn’t mean you should let your guard down when it comes to other precautions. The CDC still urges immunocompromised people to practice mitigation efforts, even after receiving their additional COVID-19 vaccine dose. This means:
- Wearing a mask in public settings
- Maintaining a social distance of six feet from those who do not live with you
- Avoiding crowds and poorly ventilated indoor spaces
- Washing or sanitizing your hands frequently
- When spending time with loved ones, remember that outdoors is safer than indoors
Additionally, per the CDC’s recent recommendations, fully vaccinated people who have a known exposure to someone with suspected or confirmed COVID-19 should be tested three to five days after exposure and wear a mask in public indoor settings for 14 days or until they receive a negative test result. If you are exposed to COVID-19, talk to your health care provider about getting monoclonal antibody treatment, which was recently approved to treat and prevent COVID-19 post-exposure in immunocompromised people.
Encourage family members, coworkers, friends, and community members to get vaccinated if they’re eligible and haven’t done so. Here’s how to talk to loved ones about getting the vaccine.
As the Delta variant spreads and daily COVID cases increase, it is important to be vigilant in your efforts to remain safe and protected. Getting the third COVID-19 vaccine dose is an important step if you’re immunocompromised.
Get Free Coronavirus Support for Chronic Illness Patients
Join the Global Healthy Living Foundation’s free COVID-19 Support Program for chronic illness patients and their families. We will be providing updated information, community support, and other resources tailored specifically to your health and safety. Join now.
ACIP Presentation Slides: August 13, 2021 Meeting. Advisory Committee on Immunization Practices. U.S. Centers for Disease Control and Prevention. August 13, 2021. https://www.cdc.gov/vaccines/acip/meetings/slides-2021-08-13.html.
Brosh-Nissimov T, et al. BNT162b2 vaccine breakthrough: clinical characteristics of 152 fully vaccinated hospitalized COVID-19 patients in Israel. Clinical Microbiology and Infection. July 7, 2021. doi: https://doi.org/0.1016/j.cmi.2021.06.036.
Coronavirus (COVID-19) Update: FDA Authorizes Additional Vaccine Dose for Certain Immunocompromised Individuals. U.S. Food & Drug Administration. August 12, 2021. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-additional-vaccine-dose-certain-immunocompromised.
COVID-19 Vaccine Clinical Guidance Summary for Patients with Rheumatic and Musculoskeletal Diseases. American College of Rheumatology. May 24, 2021. https://www.rheumatology.org/Portals/0/Files/COVID-19-Vaccine-Clinical-Guidance-Rheumatic-Diseases-Summary.pdf.
COVID-19 Vaccines for Moderately to Severely Immunocompromised People. U.S.Centers for Disease Control and Prevention. August 13, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/immuno.html.
Haidar G. Immunogenicity of COVID-19 Vaccination in Immunocompromised Patients: An Observational, Prospective Cohort Study Interim Analysis. medRxiv. June 30, 2021. doi: https://doi.org/10.1101/2021.06.28.21259576.
Hall VG, et al. Randomized Trial of a Third Dose of mRNA-1273 Vaccine in Transplant Recipients. The New England Journal of Medicine. August 11, 2021. doi: https://doi.org/10.1056/NEJMc2111462.
Immunocompromised Individuals. U.S. Food and Drug Administration. August 12, 2021. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-additional-vaccine-dose-certain-immunocompromised.
Interim Public Health Recommendations for Fully Vaccinated People. U.S. Centers for Disease Control and Prevention. July 28, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated-guidance.html.
Interview with Amesh A. Adalja, MD, a Senior Scholar at Johns Hopkins Center for Health Security
Kamar N, et al. Three Doses of an mRNA Covid-19 Vaccine in Solid-Organ Transplant Recipients. The New England Journal of Medicine. August 12, 2021. doi: https://doi.org/10.1056/NEJMc2108861.
Possible Side Effects After Getting a COVID-19 Vaccine. U.S. Centers for Disease Control and Prevention. August 6, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/expect/after.html.
Rabinovitch A. Israeli survey finds 3rd Pfizer vaccine dose has similar side effects to 2nd. Reuters. August 8, 2021. https://www.reuters.com/business/healthcare-pharmaceuticals/israeli-survey-finds-3rd-pfizer-vaccine-dose-has-similar-side-effects-2nd-2021-08-08/.
Tenforde MW. Effectiveness of SARS-CoV-2 mRNA Vaccines for Preventing Covid-19 Hospitalizations in the United States. medRxiv. July 8, 2021. doi: https://doi.org/10.1101/2021.07.08.21259776.