Gout is a type of inflammatory arthritis that happens when levels of uric acid — a normal byproduct of metabolic reactions in your body — become too high. When levels of uric acid get so high that your body can’t easily dissolve and excrete it (via urine), uric acid starts to crystallize. Uric acid crystals deposit themselves in the joints where they cause severe inflammation. The big toe is a well-known site of gout attacks, but gout can strike many different joints throughout the body.
Gout is one of the oldest recorded diseases, with accounts dating back to ancient Egypt. This incredibly painful arthritis affects millions of U.S. adults today just as it did in historic times, as described memorably by Dr. Thomas Sydenham in the 17th century:
“The victim goes to bed and sleeps in good health. About two o’clock in the morning he is awakened by a severe pain in the great toe; more rarely in the heel, ankle or instep…The pain, which was at first moderate, becomes more intense…So exquisite and lively meanwhile is the feeling of the part affected, that it cannot bear the weight of bedclothes nor the jar of a person walking in the room.”
Fortunately, today gout is one of the most treatable forms of arthritis — some rheumatologists say it can be cured. But for too many patients with gout, the disease goes untreated or undertreated. In one recent study, for example, only 37 percent of people with gout were taking the uric acid-lowering medication allopurinol; among gout patients with frequent flares, only half were taking it.
Improperly treating gout can cause the disease to become more progressive. Over time, gout can begin to affect more joints throughout the body and cause problems like gout tophi and permanent bone damage.
Find out more here about how gout develops, how gout progresses through different stages, and how to treat gout to prevent symptoms, lower uric acid levels, and prevent long-term gout complications.
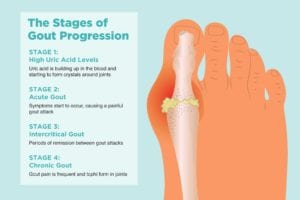
Stage 1: High Uric Acid Levels
Also called asymptomatic hyperuricemia, in this beginning stage of gout, uric acid is building up in the blood and starting to form crystals around joints, most often in the foot.
Uric acid is created when your body breaks down substances called purines, which are produced in your body and can also be found in certain foods and drinks. While eating high-purine foods can contribute to high uric acid levels, many experts believe that the role of diet in the development of gout is over-emphasized. Chronically high levels of uric acid happen when your kidneys aren’t able to efficiently get rid of uric acid, which can happen for a number of reasons, including:
- Overweight
- Kidney disease
- Taking diuretics
- Drinking alcohol in excess
- Diabetes
- Underactive thyroid
- Genes/family history
- Eating a high-purine diet
“In this first stage of gout, the person has no joint pain, no red or swollen joints, just an elevated uric acid blood test,” says Theodore R. Fields, MD, FACP, rheumatologist at the Hospital for Special Surgery in New York City. “This is the time that the uric acid, or urate, crystals are collecting in the joints and can cause inflammation later on.”
But high uric acid isn’t enough for a diagnosis of gout itself. “Most people with hyperuricemia never develop clinical gout,” says Alireza Meysami, MD, FACR, FACP, rheumatologist at the Henry Ford Health System in Michigan.
Stage 2: Acute Gout
At this point, that sudden, unexpected nighttime attack of gout symptoms might occur.
“This is when the person has pain, redness, and swelling of a joint, most commonly in the big toe, the foot, the ankle or the knee, but gout can start in other joints as well,” says Dr. Fields. “This is when the urate crystals are released into the joint fluid and cause an inflammatory reaction, bringing in many white blood cells and releasing inflammatory chemicals that cause the pain, redness, and swelling.”
If you think you’re experiencing a gout attack, see your primary care doctor or a rheumatologist to begin treatment for the disease. It’s important to see a doctor during a gout flare because your doctor may want to remove fluid from the affected joint and look at it under a microscope to check for the presence of uric acid crystals. Identifying uric acid crystals in joint fluid helps confirm a gout diagnosis.
Stage 3: Intercritical Gout
After a first gout flare, 75 percent of people will have a second within a year; but some people can go years before another attack, says Dr. Fields. The in-between stage is “where a person has already had a gout flare but is presently not having any joint pain or swelling,” he says. “Almost all gout patients will go through this phase, since it is the nature of gout to have flares and then quiet down for a period of time before the next flare.”
Even though it may seem like nothing is happening, this is the point in which patients should begin long-term treatment. Lowering uric acid levels with medication can prevent future gout flares and long-term complications that go with them.
Stage 4: Chronic Gout
This stage is also called “tophaceous gout” because the uric acid deposits can form nodules called “tophi,” often at the bunion point of the big toe or at the elbow. But tophi can form anywhere in the body. “This stage is where a person can have some joint pain from gout just about all the time,” Dr. Fields says. “It usually takes many years of uncontrolled gout for someone to get into this stage.”
During this stage, progressive joint damage develops, so patients with gout should be treated before this starts happening. “Treatment delays can make gout worse,” Dr. Meysami says.
How to Know If Your Gout Is Progressing
As you become more familiar with gout symptoms, you may be able to sense that a gout attack is coming on. “Worsening of pain, swelling, redness, and warmth of the affected joint during the attack is the sign of progression of that attack,” Dr. Meysami says.
In addition, the disease overall may progress with “recurrent or more frequent gout attacks with longer duration, the involvement of more joints, and the presence of tophi,” Dr. Meysami says.
If you have more than one gout flare a year, it’s really important to get on a regular gout medication, says Dr. Fields.
What Makes Gout Get Worse
Without treatment, gout will usually progress. In addition, certain factors may trigger gout flares. “Anything that makes urate levels go suddenly up or down can set off gout,” Dr. Fields says.
Diet
This may include eating foods high in purines, which get broken down into urate, such as red meat and shellfish. Foods high in fructose can also increase the body’s production of urate. Alcohol decreases the excretion of uric acid in urine, which can cause uric acid levels to increase. Specifically, “beer not only has the effect of alcohol on uric acid in the urine, but also has protein that breaks down to purine and then urate, so it increases urate in two ways,” Dr. Fields says.
Although you may want to limit foods high in purines to prevent flares, both doctors we interviewed said that diet alone isn’t enough to control gout. “Strict dietary purine restriction is rarely recommended, as it lowers mean serum [blood] urate levels by only about 1 mg/dl, which isn’t enough for most patients,” Dr. Meysemi says.
Gout was once called the “disease of kings,” but it was misunderstood to be simply caused by rich food and drink. “Gout is a genetic disease — in which your body either puts too much urate into the urine or makes too much urate — and not a dietary disease,” Dr. Fields says. “Watching your diet can definitely help with gout flares, but to counteract a genetic tendency to gout you almost always need medication.”
So if you notice that certain foods bring on gout symptoms, avoid them. “The consumption of alcoholic beverages or rich foods can trigger gout attacks in some patients, and the individual patient should avoid triggers known to cause attacks,” Dr. Meysemi says.
Obesity
However, one of the risk factors for gout is obesity. In fact, gout has become more prevalent recently possibly to due to rising levels of obesity. “Weight loss in someone who is obese will have a greater urate-lowering effect than a purine-free diet,” Dr. Meysemi says. To that end, a healthy diet and exercise can help you lose weight and reduce your chances of disease progression.
Stress and Injury
Emotional stress can also bring on a gout attack. So can physical trauma to the foot (such as might occur during running), which may release some crystals and cause an inflammatory reaction.
“We don’t discourage people with gout from running or other exercise,” Dr. Fields says. “But if someone has a gout flare in the foot, ankle, or knee, we suggest they stay off the foot as much as possible, since further trauma to a joint with a gout flare can prolong the flare.”
Starting a treatment regimen can also unintentionally set off a flare; but other medications can also be given to help mediate this risk.
How Gout Treatment Prevents Disease Progression
Fortunately, in part because of its long history, gout is one of the most well-understood and most medically treatable forms of arthritis. “The progression of gout is preventable by starting appropriate treatment as soon as possible,” Dr. Meysami says. “Uric acid-lowering agents, such as allopurinol [a medication that’s been used since the 1960s], can decrease uric acid levels and prevent gout attacks.”
During flares, gout patients can take NSAIDs (non-steroidal anti-inflammatory drugs) or corticosteroids to calm the attack. Local steroid injections may also be given. A medication called colchicine (Colcrys) is also often used to stop acute attacks, but it’s given now at a much lower dose in order to avoid side effects, including stomach upset.
After a flare ends, long-term treatment can begin. “Almost all people with gout will need medication to control their urate,” Dr. Fields says. “To get a good outcome, people with gout need to get their blood urate level below 6.0 mg/dl and keep it there. By doing that, the body will gradually pull the urate crystals out of their joints, and the flares can stop.” Tophi will also gradually disappear.
Medications called xanthine oxidase inhibitors limit the amount of uric acid your body produces. These include allopurinol (Zyloprim and Aloprim) and febuxostat (Uloric). Colchicine, which decreases the inflammatory response to gout, may also be given along with allopurinol at the start of long-term treatment after a flare subsides.
Another class of drugs called uricosurics help your kidneys remove uric acid from the body. These include probenecid (Probalan) and lesinurad (Zurampic). An infused drug called pegloticase (Krystexxa) can help the body eliminate uric acid in people whose gout hasn’t been well controlled with other medication. New medications, including a biologic currently FDA-approved for rheumatoid arthritis, are on the horizon for gout treatment as well.
Your doctor will review your medical history for any contraindications for gout medications. You may be directed to stop taking diuretics (water pills), as these can contribute to uric acid buildup.
In addition to weight loss, diet, and physical exercise, talk to your doctor about any other home remedies for gout — but you’ll almost always need meds as well. For example, “cherry juice may slightly lower urate level but in general is not advised [alone], since if someone is having trouble with gout they should be on a medication such as allopurinol, which is much more potent,” Dr. Fields says.
Can Gout Be Cured?
“‘Cure’ is a very strong word, but we can certainly treat the gout and put it in remission by giving the treatment as mentioned,” Dr. Meysami says.
Whether to use the word “cure” may be a matter of semantics: A patient’s gout tendency may never go away but can be well-controlled. “Treatments for gout are extremely good, and the vast majority of gout patients can expect to be ‘cured,’” Dr. Fields says. “‘Cured’ is in quotes since it means that gout flares can completely disappear, but the person would need to stay on their medicine.”
Gout progression, though, certainly isn’t inevitable, which is close to the best news any gout patient can hear.
Keep Reading
If you enjoyed reading this article, you’ll love what our video has to offer.