NO ONE ASKED TO BE PART OF THIS CLUB, BUT HAVING THE RIGHT SUPPORT CAN MAKE A BIG DIFFERENCE IN YOUR ABILITY TO LIVE BETTER WITH PSORIATIC ARTHRITIS.
The Psoriatic Arthritis Club podcast series delves deep into the ups and downs of living with PsA. Through intimate conversations with fellow patients and insights from leading experts, the series offers valuable information on how to manage symptoms, collaborate with health care providers, advocate for better care, and emotionally cope with the disease. Along the way, listeners will also pick up life hacks, tips, and tricks to live better with psoriatic arthritis.
THE PSORIATIC ARTHRITIS CLUB EPISODES
Check out episodes of The Psoriatic Arthritis Club below and wherever you listen to podcasts. Be sure to subscribe for access to future episodes. Tell your family and friends to listen, too, so they understand what PsA is all about.
NEW: SEASON 3
Episode 1
Balancing Treatment Goals in PsA and axSpA with Dr. Khattri

In this episode, Dr. Khattri, a triple board-certified dermatologist, rheumatologist, and internist, discusses the complexities and goals of achieving remission in Psoriatic Arthritis (PsA) and Axial Spondyloarthritis (axSpA). Dr. Khattri explains the concept of minimal disease activity, and the various measures to assess disease activity. The discussion also highlights the importance of patient-clinician collaboration, regular assessments, and addressing comorbidities for holistic care. Dr. Khattri emphasizes shared decision-making and tailoring treatment plans to patient needs and expectations.

Managing PsA and axSpA Comorbidities: From Heart Disease to Hidradenitis Suppurativa
Managing PsA and axSpA may require learning to spot and manage other health issues. Here’s how to work with your care team to prevent comorbidities from compromising your quality of life and path to remission.
Episode 2
Busting Psoriatic Arthritis and Psoriasis Myths with Jody Quinn

Psoriatic arthritis (PsA) and psoriasis (PsO) are often misunderstood, leading to widespread myths that can make managing these conditions even more challenging. In this episode, patient advocate Jody Quinn joins host Shelley Fritz to set the record straight. From the misconception that PsA is just mild joint pain to the belief that only older adults are affected, Jody shares her personal journey and lived experiences to debunk these common myths.
Whether you’re living with PsA or supporting someone who is, this episode offers valuable insights to help you navigate the condition with confidence.
SEASON 2
Episode 1
Ashley’s Journey: From Reluctance to Resilience in Managing PsA

Ashley Krivohlavek discusses her journey to find the right PsA treatment, including her initial fears of starting treatment, concerns through seven treatment changes, and balancing side effects with quality of life.

Episode 1 - Ashley's Journey: From Reluctance to Resilience in Managing Psoriatic Arthritis
Narrator 00:00
Be inspired, supported, and empowered. This is the Global Healthy Living Foundation Podcast Network.
Ashley Krivohlavek 00:06
They really want you to stay on those biologics for x number of months to make sure that they’re working and stuff. So I was really trying a biologic once a year, basically, and moving through, ticking them off one by one. Oh my gosh, I’ve changed so many biologics. I think I’ve counted seven different ones in the last nine years, six or seven different ones, and then I finally hit on one in the last year and a half two that has kept me steady.
Angela Degrassi 00:42
Finding the right treatment for psoriatic arthritis is certainly a winding road filled with trial and error hesitations and moments of hope. If you or someone you love lives with psoriatic arthritis, this experience might sound all too familiar. Have you tried multiple treatments? Were you ever hesitant to switch due to worry over safety concerns, side effects, or fear of switching from a pill to an injection? We’ve asked these questions to members of our psoriatic arthritis patient community to learn more about their treatment journey and how they worked with their health care provider to navigate the hope, fear, and challenges that come with finding the right treatment for you. A treatment that brings relief and improves quality of life.
Ashley Krivohlavek 01:33
My name is Ashley Krivohlavek and I am in Tulsa, Oklahoma. I am 39. I’ve been living with psoriatic arthritis for about nine years now. And I just graduated with a certificate, a master’s certificate in population health. I am working on the submission a patient perspectives submission for American College of Rheumatology. And I am taking the summer off, I guess for right now. And we’ll see what comes next.
Angela Degrassi 02:06
Hi, I’m Angela Degrassi, and I’m the host of The Psoriatic Arthritis Club, a podcast from CreakyJoints and the Global Healthy Living Foundation. We’re back for a second season to further explore the ups and downs of managing and treating PsA, which for the uninitiated is an abbreviation for psoriatic arthritis. We’re going to talk about things like what’s working and what isn’t. We’ll be sharing insights from patients and leading rheumatologists. So let’s get going. Hi, Ashley. It’s always great to talk to you. Welcome to the show.
Ashley Krivohlavek 02:38
Hi, Angela. It’s so exciting to be a part of this. I am so excited to do this.
Angela Degrassi 02:45
I am always happy to talk to you, Ashley. And I want to share with our listeners a little bit more about you. So in addition to making a submission for the American College of Rheumatology Patient Perspective program, just completing a master’s program and job hunting, there is so much more about you and so much more work that you’ve done. You have been featured in WebMD, Women’s Health.com, Reader’s Digest, just to name a few. You also sit on the Global Healthy Living Foundation’s Patient Governor Group, which I am also a part of as well. And you Co-Chair the Central Region Advocacy Board for the National Psoriasis Foundation. This year, the National Psoriasis Foundation named you Advocate of the Year, so congratulations on that.
Angela Degrassi 02:45
Aw, thank you. It was such a surprise. I honestly did not know it was coming until it was already done. I didn’t know I was even in the running. So wow, it was a nice surprise.
Angela Degrassi 03:48
Well, congratulations. And that’s a great accomplishment. You’ve also worked with the Arthritis Foundation and with the Arthritis National Research Foundation. You also recently wrote an op-ed in support of step therapy reform in Oklahoma and spoke with local lawmakers about copay accumulator reform. There’s no doubt that you are a very busy patient advocate.
Ashley Krivohlavek 04:09
Yes, I try to stay busy, it is passion work, is what is, it’s a labor of love.
Angela Degrassi 04:16
We can tell.
Ashley Krivohlavek 04:17
It does keep me quite busy, but I am so proud to be doing it.
Angela Degrassi 04:20
So Ashley, I know you as an advocate, but I also hear that you are a voracious reader and love to read not only medical studies and research that could help you manage your condition but also enjoying literary classics like Great Expectations. This makes me wonder if someone were to write a book chronicling your psoriatic arthritis journey what title would best capture the essence of your experience?
Ashley Krivohlavek 04:50
Probably Great Expectations is great title. I guess life is like a box of chocolates.
Angela Degrassi 04:57
Good one.
Ashley Krivohlavek 04:58
You just never know what you’re going I’m gonna get day to day with this.
Angela Degrassi 05:01
So that’s a good one. You never know what you’re going to get. So what was that like for you? Can you tell us? What were those symptoms that you experienced that first prompted you to take action and talk to your doctor about what was going on?
Ashley Krivohlavek 05:16
Yeah, when you look back, probably there was a lot of lead up to the diagnosis, but you just don’t realize it’s always like weird little quirky things. And so I do remember though, I went to bed one night, and then the very next day, I woke up and I was swollen, I was sore. I couldn’t move very well, like it was just a lot, a lot of like the classic symptoms of psoriatic arthritis, and I have family history of autoimmune. So I kind of in the back of my head had the idea that I probably should be seeing a rheumatologist at this point. So it took a while to get into the rheumatologist. I think it was about a month, maybe two. And I got diagnosed shortly after we ran a lot of tests. And they had called the inflammatory arthritis because they weren’t sure yet. So they started me on like Plaquenil. And, and then we finally figured out it was psoriatic so. It just felt very like sudden it was one day, I was fine. I went to bed. And then the next day, I woke up and had all of these symptoms, and they just have not abated.
Angela Degrassi 06:30
You describe that well, and it’s a story we’ve heard from other people, too, you start to have the symptoms, and then there’s a long wait to see a rheumatologist and get that first appointment. And then you finally receive your diagnosis. Let’s let a medical professional weigh in. I want to introduce you to another guests that we have with us today. Dr. Ruderman is the Associate Chief of Clinical Affairs in the Division of Rheumatology at Northwestern University’s Feinberg School of Medicine. Dr. Ruderman will be our guest in our third episode, and will provide his insight as a medical professional. Dr. Ruderman, what do you think of Ashley’s story, and what have other patients told you about the onset of their PsA? And are there any classic symptoms that people might experience that would convince them that something’s really wrong, and they should seek medical attention?
Dr. Ruderman 07:21
You know, that story is not all that unusual. But it isn’t always that rapid, but it can be. And I talked to a lot of people who, as you said, Ashley, things are going on, and you’re not so sure, but then all of a sudden, there’s a big change. And that’s what prompts you to seek help and get help. Unfortunately, it can take a long time to see a rheumatologist there aren’t enough of us. And that is a challenge. But one of the things that struck me in your story was the idea that you woke up in the morning and you just couldn’t do very much. And that’s one of the symptoms that I think should make people push their primary doctor who or their dermatologists if they’re seeing a dermatologist for psoriasis, to say, I need to see a rheumatologist because for us that kind of symptom, that kind of stiffness in the morning is one of the key hallmarks of inflammatory arthritis as opposed to osteoarthritis, which is just wear and tear that you may get as you get older. And in your situation, it was not clear that it was psoriatic arthritis up front, but in many ways, just knowing that it’s inflammatory is going to take us down a path to get you to the right approach into the right therapy. And so those kinds of symptoms, whether it’s sudden or not, and sometimes it’s sudden and sometimes it isn’t, but you know, I tell people if it takes you an hour or two or three to get going in the morning, that’s not right. And that should prompt you to talk to your doctor to help get you to see rheumatologist to figure out what’s going on and what we can do about it.
Angela Degrassi 08:46
Thanks for that insight. It’s evident that the journey to a diagnosis and effective treatment for inflammatory arthritis can be challenging, especially considering the scarcity of rheumatologists. Ashley, did you have both joint and skin symptoms at the beginning?
Ashley Krivohlavek 09:01
So when I was 12, I was diagnosed with psoriasis and it was mainly on my scalp. So I knew that I had psoriasis but I don’t remember them ever talking about the potential for the psoriatic arthritis at that time, and I just I thought, okay, well, I’ve kind of got this under control. Like I had the idea that I would be living with psoriasis for the rest of my life, but it was kind of like in a remission state I didn’t have and still do not have a lot of skin activity. So when I woke up with all the joint stuff, it was like I had a lot of people in my family that had rheumatoid or like lupus. So those were my first suspects. And then as we kind of went along, now I remember sitting in the doctor’s office and they go down a long list of like family and medical history with you and they were like psoriasis I was like, yeah, no. And that was it. Wait, yeah, actually, I do have psoriasis. I had not been kind of like a part of my every day. So I didn’t really think about it anymore. Like it had been in remission. And I never really had a ton of skin activity. So when they listed that, and I was like, oh, wait, yes, I actually do have psoriasis. They started doing the antibody testing. And then that’s when we found out it was that.
Angela Degrassi 10:29
What was it like starting treatment for your very first time?
Ashley Krivohlavek 10:33
It was hard, it was really hard. I have stomach issues. So oral medications is really what they want you to start with. And because one they’re cheaper, and two, that’s what most patients want to take is just a pill and I was very much on board with that. But I had so many stomach issues that I finally was just like, I don’t think I can do this. The rheumatologist and I we made the collective decision to get on a medication that would be injectable and started with a DMARD injectable DMARD and from there just kind of gradually added things biologics to the mix as well. And they’ve always been injectables or infusions for me because of said digestive issues.
Angela Degrassi 11:23
Yeah, so getting started on those meds must have been a really challenging time. For those of us that don’t know, can you tell us what a DMARD is?
Ashley Krivohlavek 11:32
So it is a disease modifying anti-rheumatic drug.
Angela Degrassi 11:37
When you started your first DMARD and biologic, did you have any hesitancy due to safety concerns?
Ashley Krivohlavek 11:45
Oh, my gosh, yes. When they give you like the printout sheet of all of the stuff that you can do, you can’t do or you can’t take this with this there’s interaction, it was so scary, I really didn’t know, I hesitated a lot. Before I really got on anything that was especially biologics, I fought really hard not to be on them for as long as I possibly could just because I was the list of things. The interaction is so long, and I was just very worried too about my future with because I was looking at with these medications for somebody that’s younger, you’re looking at decades on these medications. And so do you want to start that right now, you know, at such a young age? There were just a lot of variables to it. And what ultimately got me to doing it was one I was not functional, I wasn’t able to do anything. My symptoms were not being managed well and I was tired all the time, the fatigue was just overwhelming. So I wasn’t like a productive member of society at that point. And I saw what non-treatment can do to joints and deformities, because my maternal grandfather had rheumatoid and walked with a cane my entire life. And so I saw the deformities and how if you don’t do treatment, this could be a future for you. So it was very much like, okay, I don’t want to go that route either.
Angela Degrassi 13:33
So seeing some advanced disease activity, in someone else kind of gave you the nudge to get started on that treatment.
Ashley Krivohlavek 13:41
Absolutely. He didn’t have those options. Biologics were not around when he was doing, you know, going through. And I don’t even know if they were using a lot of DMARDs. I just saw what it was doing what it could do. And it was not a future I wanted to see myself go down. It was quite, that was more scary to me. At the end of the day, than laundry list of things that could potentially go wrong with being on a biologic or DMARD.
Angela Degrassi 14:12
Right. And has the same treatment worked for you over the years, or has there ever been a time where you change treatments?
Ashley Krivohlavek 14:20
Oh my gosh, I’ve changed so many biologics.
Angela Degrassi 14:23
I can imagine. Tell us about what that was like. What made you come to that decision where you said okay, this isn’t working time to try something new? And did you have those conversations with your rheumatologist?
Ashley Krivohlavek 14:34
My rheumatologist I almost feel very sorry for them because I’m very much like okay, I want to go and look at symptoms so I track symptoms with Arthritis Power. I use that app.
Ashley Krivohlavek 14:39
I am always happy to hear people say that, that’s awesome, Ashley.
Ashley Krivohlavek 14:57
It truly is. I mean, not because this is Global Healthy Living, but it was really truly just something that was useful to me. And so I would track symptoms and I would say, okay, I got infusion this day, and for three days afterwards, I was fatigued and literally slept like 16 hours out of a day or something, you know, and I really did want to quantify all of the symptoms. So I would go in with a laundry list of things for my rheumatologist to go over. And they’re just wanting like a quick 10-15 minute like, how are you feeling? No, I came in, like armed, so much information, and would really drive me is if the combination of my symptoms were not being managed, and labs were not going down or even near normal, it just didn’t make sense to keep staying on a very expensive medication that’s obviously not working. And so my goal always was to be one of those patients where I could just go in for 10-15 minutes and be like, yeah, everything’s good. Let’s keep up the momentum. So what really drove me was the combination of symptoms in my labs, and I went through with biologics, I think I’ve counted seven different ones in the last nine years, six or seven different ones. And then I finally hit on one in the last year and a half to that has kept me steady.
Angela Degrassi 16:30
So that’s a lot of big changes in just a few years.
Ashley Krivohlavek 16:33
Yeah. And they really want you to stay on those biologics for x number of months to make sure that they’re working and stuff. So I was really trying a biologic once a year, basically, and moving through, just ticking them off one by one.
Angela Degrassi 16:51
And has there ever been a time when you felt complacent in your treatment, or a time where you were not feeling your best, but perhaps not quite ready to change your treatment? Because the thought of changing might have felt a little too daunting?
Ashley Krivohlavek 17:05
So like, every time that I’ve had to do it, yes. Because along with changing medication, you don’t know how you’re going to react to it. And so that’s daunting. And then the prior authorizations, I mean, that among itself is a full time job, just trying to get those taken care of, the back and forth between your insurance company and the doctor’s office and the pharmacy. But I knew that once I hit on one, I would stay on it for as long as possible. So a good example of this is recently I went from this particular medication that I have been on for about at this point, it was about a year, year and a half was infused. And it just became very daunting to have to go to the infusion center every month. And so I decided, maybe we should try the injectable version. And so even though it’s the same medication, you still have to go through the prior authorization. And then you have to go through the specialty pharmacy and the doctor’s office. And it can be like almost a two month process before you’re approved. So I started that journey in January, and I finally got approved and started with injectables in March. And it was weird because I really wanted to make sure that like I would be getting full benefit from injectables that I was getting from infusion. But this change was more because of a desire to look for my lifestyle not wanting to go into the doctor’s office, you know, every month for infusion, so it was really just about my comfortability not that it didn’t work or it wasn’t working. And so I almost felt guilty about that, because it was like it’s fine as it is it’s just harder for me. And it’s harder for the scheduler because rheumatologists are so busy. It was difficult to keep at a four week mark. So anyway, I made the decision. And I mean, I’ve been on it for three ish months now. And so far, so good. So let’s just keep our fingers crossed on that.
Angela Degrassi 19:19
We’re happy to hear that my fingers are crossed for you. Let’s talk about flares. Flares are a hallmark of rheumatic disease. Do you experience flares? And what are they like?
Ashley Krivohlavek 19:32
Yes, flares are always going to be a part of my life, even though I think probably I think everybody’s late definition of remission is different. I would probably say that I don’t have like every day activity with my joint anymore and my labs are really getting close to being average, which is new for me. So when I do have flares and almost like triggers, like, Is this the one? Is this the one that’s gonna pull me out of remission? It’s very scary.
Angela Degrassi 20:07
Can you tell when you’re about to have a flare? Are there any warning signs or symptoms that you know, oh, I know what’s coming?
Ashley Krivohlavek 20:15
Yeah, I get a really dull ache in my fingers, particularly. And then I start really wanting to sleep. Fatigue is like a huge thing for me. So those would be my two things. And also, I don’t know if anybody else has this, but I get this weird like sensation in my knees, almost like a numbing sensation. And when I get that, then my fingers start in, and then the fatigue kind of sets in. And so it really does start with the weird knee numbness type thing in my knees. And that’s really my first indicator that something’s coming. But right now, the only time that I really have issues is if it’s raining, you know, weather type stuff? Or if, of course, stress will do. Stress does with every day.
Angela Degrassi 21:06
Yes, yes, stress is a big one. Can you tell us if you have any hacks or tips that you can share with people that might help with flares or dealing with your symptoms?
Ashley Krivohlavek 21:19
Yeah, so what I have to remember, and this is the biggest hurdle, like, it’s the easiest thing, but it’s also the hardest thing is to remember that it shall pass. And then you need to absolutely take care of yourself, truly listen to your body. So if your body’s like you’ve hit the wall, you need to go take a nap. That’s exactly what I need to do. And I communicate that to people around me. And the other thing that has truly helped me get through flares has been my support network, I have so many people in the same community that we just rally around each other, somebody who’s having a flare, and we’re like, okay, what can we do? Can we send you food? Can we send you some groceries? Or, you know, whatever else do you need? Do you want to just text? Or do you want to call? So community has been huge for me. And if these aren’t like, yes, put some Biofreeze on your joint and call it a day. But they truly do help to have that kind of like outlet. And a lot of times now for me it is just a mental hurdle. Like there’s nothing really at this point that I can do in terms of doing all of the medication type stuff. And you know, a doctor would tell you or rheumatologist would be like, here, it takes him steroids for your flare. And if you don’t want to go that route, it’s really just like trying to mentally get through the pain and the like swelling and all of the other things.
Angela Degrassi 22:51
I’m so happy to hear you have that support group I really am. It’s great to know that you have people that know what you’re going through, how did you connect with those people that are in your support system?
Ashley Krivohlavek 23:04
Oh my gosh, so through trial and error, but the first was through Twitter, I was on Twitter, I was very active for a very long time there. And I met so many amazing people. And I met them really through doing CreakyChats and supporting each other through posts and stuff like that. And then meeting people to a just different advocacy avenues. And I’m the co chair for another committee. And it’s people that are locally in my region. So it’s nice to have people that are local to me as well. And that’s where we really connect with people who is really through social media seems so weird, because you always hear the negatives about social media. But I now have people that I am talking to you regularly every single day. And I’m so proud of them.
Angela Degrassi 23:59
That’s really fantastic. And we are going to wrap up this episode by asking you one last question, what’s a secret that you would only tell members of the psoriatic arthritis club or those who may become part of the club?
Ashley Krivohlavek 24:12
Oh, it’s a club, you don’t want to be a part of if you can help it, but since you’re already a member, you know, welcome. I’m truly sorry that you’re going through this, but we will get through it together. We’re very strong together and you can’t do it alone. And I want everyone to feel like they’re included and that they have a support. And truly that is been a huge transition for me. As I’ve gone through the many, many stages of psoriatic arthritis and treatments. That community is there. So welcome, and let’s do this.
Angela Degrassi 24:54
Those are really comforting words. Thanks so much for sharing your time with us today, Ashley. You really are an expert and I’m really happy I got the chance to talk to you.
Ashley Krivohlavek 25:03
Thank you so much Angela, and Global Healthy Living Foundation for all of the opportunities that you have afforded me. I’m truly blessed to work with so many amazing people. And I’m so excited to be a part of this podcast. So thank you.
Angela Degrassi 25:21
We feel the same way. Thanks, Ashley. I always appreciate talking to you. And to our listeners. That’s it for The Psoriatic Arthritis Club. Thanks so much for listening, and we hope that Ashley’s story will resonate and help you discover inspiration on your disease journey. And if you haven’t already, make sure to check out our first season where we share more incredible stories that inspired and touch the hearts of our community. You can find all episodes on our platform. This podcast was made possible with support from AbbVie. For more information and stories from other PsA patients like you subscribe to The Psoriatic Arthritis Club or visit PsoriaticArthritisClub.org. You can also visit CreakyJoints.org for the latest information and news about living better with PsA. If you like what you’ve heard, be sure to rate our podcasts, write a positive review and spread the word by sharing with your friends and family. It’ll help more people like you find us.
Narrator 26:22
Be inspired, supported, and empowered. This is the Global Healthy Living Foundation Podcast Network.
Episode 2
Jonathan’s Journey: Confronting Fears and Finding a Treatment Path


Jonathan Arora talks openly about his journey from diagnosis to treatment. He addresses his initial hesitation due to concerns about drug safety and side effects, offering insights into overcoming these fears and finding community.











Episode 2 - Jonathan's Journey: Confronting Fears and Finding a Treatment Path
Narrator 00:00
Be inspired, supported, and empowered. This is the Global Healthy Living Foundation Podcast Network.
Jonathan Arora 00:09
There was a lot of emotions actually getting to that point, with most insurance companies getting the approvals filling out the forms. I was very lucky with this particular biologic, the company behind them, they have an amazing care team that reached out and was able to help me with that. So a lot of mixed emotions. We had all the hope that this treatment would be the right one, there was happiness, relief, anticipation, a little bit of anxiety as well. What if this doesn’t work the way that we expect it to? What’s going to be the plan, but you know, you kind of take that one day at a time.
Angela Degrassi 00:46
Seeking the optimal treatment for psoriatic arthritis can be filled with uncertainty, decisions, and glimmers of hope. If you or a loved one is dealing with psoriatic arthritis, these mixed emotions may be all too recognizable. Have you fretted over trying new treatments had fears over safety, side effects, or the thought of transitioning from a pill to an injection? In our second episode, we continue to explore these questions with members of the psoriatic arthritis community delving deeper into their treatment experiences in collaboration with health care providers, we uncover the courage, confusion, and determination that define the pursuit of a treatment that manages your symptoms and enhances your overall well being.
Jonathan Arora 01:37
Hi, I’m John Arora. I am 38 years old. I’ve been living with psoriasis and psoriatic arthritis diagnosed since I was 13 years old. I am in the Toronto area in Canada. I am a huge basketball fan. I love to cook and I very much enjoy my career in cybersecurity.
Angela Degrassi 01:57
Hi, I’m Angela Degrassi. I’m the host of The Psoriatic Arthritis Club, a podcast from CreakyJoints and the Global Healthy Living Foundation where we explore the ups and downs of managing and treating PsA, which for the uninitiated, is an abbreviation for psoriatic arthritis. We’ll be sharing insights from patients and a leading rheumatologist. All right, John, let’s dive in. Thanks for taking the time to talk with me today. How are you?
Jonathan Arora 02:23
I’m good, Angela. Thank you. Thank you very much for having me.
Angela Degrassi 02:26
So a little more about John. John, you were diagnosed with psoriasis at the age of 12, and battled skin inflammation at varying degrees of severity. Since then, at some point in your young adult life, over 60% of your body was covered in the dry scaly, white patches of psoriasis. And then you receive that diagnosis of psoriatic arthritis at the age of 32. In addition to psoriasis, I understand you began treatment when you were 34 years old, using biologics which helped the symptoms of psoriasis and psoriatic arthritis stay under control. So John, I want to open up this conversation by asking what led you to seek a diagnosis? Can you tell us what symptoms you experienced? That prompted you to talk to your doctor?
Jonathan Arora 03:16
Yeah, absolutely. So I think one of the biggest symptoms was just the management of the scaly skin. At that time, I had been diagnosed with PsA. But none of the symptoms like the joint pain, and some of the other more common symptoms had yet to rear its head. So it was more of the coverage of scales on my body. And it was it was in talking with my wife, and it was her mother who also had psoriasis and possibly psoriatic arthritis, too. So there was kind of a shared bond between us. Up until that point, I had been a little hesitant and kind of out of the loop in terms of what treatments were available. So through the encouragement of my wife, we did a lot more research and credit to her she found a seminar on psoriasis and psoriatic arthritis that was being hosted in Toronto with one of the leading experts at the time. So when we went, it was a really great experience. So you know, after that conference, it really opened my eyes. And in terms of what the latest treatments were, there were patients there that were able to share their stories. So that was also very inspirational to to have folks that were fighting the same battle that I am sharing their treatment stories and you know, that really inspired me to say, okay, let’s do something about this. Let’s see if we can get my quality of life better. I don’t have to suffer with this anymore. So that was kind of the catalyst right there spread after that seminar that’d be attended.
Angela Degrassi 04:38
That sounds like it must have been really helpful and really important to get some really good information about treatment. And I imagine I know a lot of people have hesitancy to start a new medication, did attending that conference or seminar helped to ease any concerns you had about safety of taking these drugs?
Jonathan Arora 04:58
Absolutely. Absolutely. And that was kind of my number one hesitancy prior to going in. I had done some research myself on biologics and certain treatments. And you know, one of the things that concern me the most was the possibility of becoming immunocompromised and getting sick all the time, I was very passionate about my career and prided myself on going to work. And, you know, the idea of getting sick all the time really didn’t seem that good to me, in my mind, that was one of the big things also change, you know, the idea of having to depend on a medication that changed what that means my lifestyle and what I can do and how we can do things. So you know, going to that seminar and having people having the experts speak having other patients speak about their experiences actually doing a deep dive into some of the medications by learning that not all biologics are the same. So there are different biologics that treat certain types of psoriasis and psoriatic arthritis differently. So it really opened my eyes to a world that it’s not one size fits all. And it really laid a lot of the fears and got me excited about the prospect of beginning treatment and getting help versus have the more fear associated with it.
Angela Degrassi 06:15
And since you started treatment for that first time, are you still on that same drug? Or has there been a time where you’ve had to change?
Jonathan Arora 06:24
Yeah, I did have to make a switch. My first biologic was an oral biologic. So the decision was made with my care professional at the time that, you know, that was the kind of the best treatment for me. So the oral biologic worked, I would say for about two and a half years, it got me from I think my body was about 90%, or 85 to 90%, covered in psoriasis. And I was starting to have symptoms of psoriatic arthritis as well, you know, soreness in the knee, soreness in my joints. So as soon as I started taking that, oral biologic, it actually got me down, I would say to about 30% of my skin was covered and it took care of the joint pain and soreness. So that was great for about two and a half years. So right around I would say kind of the start of the pandemic in 2020. I was starting to notice a rebound in my skin condition and also psoriatic arthritis like the more traditional psoriatic arthritis symptoms in terms of soreness in my joints, my hands were getting very sore. It was to the point where it was starting to affect me picking up things lifting heavy, things became cumbersome soreness and my knees and my joints came back. So after working with my care professionals, and since I moved out of the Greater Toronto Area, I actually ended up switching to a new dermatologist and because my psoriatic arthritis was kicking up, I was referred to a rheumatologist as well. And the decision was made to switch me to an injectable biologic. So I’ve been on that since I believe, July of last year in July of 2022.
Angela Degrassi 07:56
Wow, that sounds like an incredible change. When you started that biologic for the first time. We’re glad you made the decision to do that. It seems like it must have had a pretty significant impact on your quality of life.
Jonathan Arora 08:08
It has been just amazing. And speaking with my dermatologist when I made the change, one of my fears was okay, I had done the oral biologic for two and a half years of work kind of okay, they were pretty good in the beginning. And towards the end, I started having a rebound of symptoms. So my concern was, okay, how much runway do I have with my new medication, and luckily, my dermatologist was very hopeful and positive about the change. He did explain that, again, certain drugs work different ways. And my condition had progressed to the point where the oral biologic I was on was really only used to treat mild to moderate psoriatic arthritis and psoriasis, whereas the injectable biologic that I’m on now treats, you know, moderate to severe, and he has multiple patients that have been on the biologic for five plus years. So it was such a relief to get on a new treatment that took care of the rebound and actually got me down, I would say I’m about 99% of my skin is now clear. And the joint pain has really gone down from where I would say on a scale of 10, from a daily seven to maybe some eights, and nines down. If I do have an odd day where there’s a bit of pain, it’s barely cracking a one now. So it’s been amazing to get on this new treatment and to have that assurance from a medical team that this is here for the long haul and I can kind of breathe a sigh of relief.
Angela Degrassi 09:37
That’s so fantastic. What a great feeling that must be to experience your condition going in a positive direction like that. What was going through your mind on the day that you started your first dose of that new treatment?
Jonathan Arora 09:51
There was a lot of emotions actually getting to that point with the you know, most insurance companies getting the approvals filling out the forms. I was very lucky With this particular biologic, the company behind them, they have an amazing care team that reached out and was able to help me with that. So a lot of mixed emotions, there was happiness, relief, anticipation, a little bit of anxiety as well, we had all the hope that this treatment would be the right one. But there was also a little bit of anxiety and fear. What if this doesn’t work the way that we expect it to? What’s going to be the plan, but you know, you kind of take that one day at a time. So yeah, I do remember an overwhelming feel of when we went to the clinic that did the injection training, my wife and I, and we went through the process. And when we got back to our car in the parking lot, it was just, wow, we’re done. Like I said, a lot of love, happiness, relief, a little bit of excitement in his patient for the future.
Jonathan Arora 10:50
Right? Do you still experience flares?
Jonathan Arora 10:53
Yes, I do. So one of the things that I think a lot of folks that have PsA, and psoriasis and other autoimmune conditions like this, and one of the things I’ve learned, and a lot of folks on social media, I do follow a bunch of folks online that that have chronic illnesses like PsA. And certain folks that have PsA, what’s been very kind of previous as a community, it was very comforting to know that other folks that are on similar treatments and have similar conditions, they still get flares, I still do get flares, but that’s okay, I’ll have a flare every now and again, where I’ll wake up and my hands are a little sore, I’ll feel a little tired, a little bit fatigued. But like I said before, on a scale of one to 10, where I was constantly in the seven to eight range. Luckily, with my experience with my treatment, you know, I’m barely cracking, I would say a two on kind of my worst days with flares. Unfortunately, they do happen, but but when they do, I’m kind of myself, I take it a little bit easier, just let myself know that it’s okay to relax a little bit, spend a little bit more time in bed, or relax a little bit more and, you know, take care of myself when it does happen.
Angela Degrassi 12:04
That’s great. Yeah, it seems like taking care of yourself. And being gentle with expectations is what you need to do when you are in that situation of experiencing a flare. You mentioned an online community, what’s it like talking to people about your condition?
Jonathan Arora 12:20
I would say really, really rewarding. You know, when I was diagnosed, the internet wasn’t what it is today at all. And I had been just living with this alone for a long time. So you know, kind of engaging with the communities now I participate in forums where folks will posts about psoriasis and psoriatic arthritis, and it’s really rewarding to be able to respond with kind words, your story, if they’re asking for advice, and just my hope is that I can give someone the push or help or guidance that, you know, that I got in that seminar. And also, you know, as a kid that had this, you know, if I can help anyone that’s feeling a little bit alone or frustrated with this condition, that is I got, you know, just the thought of that, that really just motivates me and kind of fulfills my cup, so to speak.
Angela Degrassi 13:13
That’s great. So it seems like having that community is an important part of your treatment and your disease journey. You also mentioned your wife, can you tell us a little bit about getting support from your friends and family? And what is that like?
Jonathan Arora 13:29
Absolutely. So I would say getting support from friends and family has been a big part in how I’ve been able to manage living with the condition. Early in my life, my family wasn’t too supportive of the diagnosis and no fault of their own. There really wasn’t a lot of medical information available at the time, the first GP that diagnosed me with psoriasis, and wasn’t psoriatic arthritis, yet, at the time, it was very kind of played off, like, oh, it’s just a skin condition. You know, here’s some creams. And if I was having a flare, or if I was, you know, having kind of a bad day with it, it was always just something regarded with my family growing up as well. Something you have to live with, unfortunately. So I would say support is very important. And that’s one thing I tried to advocate for. Like I said, it wasn’t until I met my wife, I really felt like I found, you know, a partner with this. And you know, I think it’s very lucky to find someone and meet someone that knew so much about my condition. So I didn’t have to explain it. She had a family member, her mother that had psoriasis, there was already that mutual understanding. So yeah, one of the things I tried to push for in the community is seek help ask family and friends for support. I know definitely myself. That’s one thing I shied away from, you know, in my young adult life, definitely in my 20s, you know, it was just something I didn’t feel comfortable talking about with my friends. So to me, that was one thing I would change if I went back, it would be to seek help and engage in communities. One thing that really bothers me, you know, growing up living with the condition is diagnosis where, oh, it’s just this, it’s something I’ll have to live with. You know, though, when I see posts like that on the online community that really kind of gets me going. And one thing I tried to advocate for is, you know, proper treatment, and you don’t have to listen to that just that one diagnosis, it’s your right to go get a second opinion from another medical professional, if you don’t agree with the advice that you’re given. And that’s one thing I wish I knew in my younger days was okay, I don’t like that diagnosis. But I thought I had to agree with it. You don’t have to agree with that, especially now with all the information that’s made available. There’s a whole community out here for you. So yeah, definitely getting the support and the backing of your friends and family, if you can, that will be an immense help.
Angela Degrassi 15:53
That sounds like solid advice. And we really hope that that can help someone find their community and find people to open up to how has your experience of having psoriasis and psoriatic arthritis changed over the years, you did mention at one point you had psoriasis plaques covering 90% of your body? I know that must have been a challenge, not just physically but emotionally as well. Do you look at this condition differently now compared to what you thought in your 20s?
Jonathan Arora 16:23
Absolutely. In my 20s, I would say I thought it was just this not horrible, but you know, very unpleasant thing I had to live with. And you know, and it affected my life in a lot of ways. Like you said, both emotionally and physically. Physically, I just remember hot days, in the summer, I had huge patches on my legs and my knees, I would not want to wear shorts. So it would be 80 degree weather outside. And I’ll still be in jeans, remembering my younger days, my friends would invite me up to like a cottage or on a trip where I know there would be swimming, I did not want to go, I didn’t want anyone to see me with those plaques. And I thought at the time, okay, this is going to be, kind of the rest of my life. And unless I get comfortable with showing my skin and maybe I will later on in life, maybe I won’t, I kind of thought that that was kind of that the hand that was dealt, so to speak. Now that I’ve had treatment, just feel very fortunate to have a treatment that works, to be able to not have to worry about any of those kind of emotional kind of hang ups I used to have about going out. And I just want to say that later on in my life before I got started treatment, I did get to a point where I say, hey, I don’t care, I’m gonna wear shorts, I’m gonna go out. And I just want to say to anyone feeling like that, if you’re comfortable with it, it’s okay to it. You know, I didn’t care about what anyone else said or thought of me. And if you can get to that point emotionally, that’s great. If you’re not, that’s okay. I live with that for a lot of time. But yeah, it’s just how I look at it now. It’s an unfortunate condition to have. But I’m very grateful that I have a treatment plan and a team of medical professionals with me, that support me, family that supports me that allow me to manage the condition and live you know, it’s a little cliche, but you know, kind of my best life.
Angela Degrassi 18:14
Yeah, great. You seem to be very resourceful to and having this condition for so many years. Now. Do you have any other advice that you would share with someone who might be newly diagnosed that might not have access to resources or a support system?
Jonathan Arora 18:32
Yeah, my advice would be first, it’s okay. It’s not your fault. First of all, and my first kind of advice would be I know getting a diagnosis like this is a shock. And I’m thinking back to when I was diagnosed with psoriatic arthritis, I kind of known that it was on the way. So I can only imagine getting a diagnosis like this out of the blue could be a shock. And I would say if you can, and this is your kind of first journey into reach out looking for resources. There is an amazing online community out there full of folks like you that have this condition and are fighting the same battles right now. And some of them are a little bit further along in the battles. So my advice would be you’re not alone. It might feel that way right now, but that’s not the truth. And folks like myself, and I know a lot of other folks in the community are very, very kind and loving and supportive. So you know, we’re out there, please reach out. Don’t get discouraged. And we’re here to help.
Angela Degrassi 19:29
Those are some great words of encouragement. Thanks for sharing that. Now. What is something you wish you knew when you were first diagnosed about advocating for yourself as a patient?
Jonathan Arora 19:39
One thing that comes to mind was the seminar that I attended. One of the best advice that I got from that seminar was to speak with not just your GP, but ask for referral to definitely a dermatologist or a rheumatologist. Looking back to when I was first diagnosed. One of the things that always surprised me was I was never passed on to that dermatologist or that rheumatologist. So to me, that would be kind of the best advice that I would pass on is, if you haven’t been referred to that kind of that next level to that specialist level, and you feel like you might benefit from it, look into that do some research, because I love my GP. But you know, I found with GPs, though, they’re gonna have varying levels of expertise into the condition. Again, if you’re ever feeling like something’s lacking, something’s missing, you can definitely advocate to get referred to a specialist. So I would say that’s probably the one advice that I was given in that kind of seminar that I would like to pass on.
Angela Degrassi 20:39
Yeah, that’s a great piece of advice. Looking back on your own journey, you realize that you weren’t automatically referred to a specialist. This sounds like a good time to introduce our other guest, Dr. Ruderman, who is a specialist, Dr. Ruderman is the Associate Chief of Clinical Affairs in the Division of Rheumatology at Northwestern University’s Feinberg School of Medicine. He’ll be our guest in our third episode, and we’ll provide his insight as a medical professional. Dr. Ruderman, what do you think of that advice that John shared with us?
Dr. Ruderman 21:09
You know John, that’s a great piece of advice. And I can’t agree more, you know, what I would say in response to that is, you know, your body and you know, how you feel, and if something’s not right, you know, that. And you’re absolutely right. GPs have different levels of expertise, they have different approaches on how much they want to think they should be able to handle on their own versus sending you out to a specialist. And you know, most of the time, if you have a good relationship with your GP, that’s going to work out fine. We often rely on them to tell us when we need to go to a specialist or whether it’s not something needs to get there. But if you’re not doing well, and they say I don’t know that you need to, you know, be your own advocate and push for that and say, you know, it wouldn’t hurt to just get an evaluation. And let’s make sure that we’re doing everything we can and that there’s not something else that we should be thinking about so that I feel better. I think that’s very appropriate. And I think that’s a great piece of advice.
Angela Degrassi 22:04
You highlighted the importance of listening to our bodies and recognizing when something feels off, we trust our GPs to guide us in our healthcare journey. And a good relationship with them can often lead to successful outcomes. Your perspective aligns perfectly with the idea of taking an active role in our health care. I’ve learned a lot so far. And I’m excited to ask this next question to John. John, you seem to be full of good advice. So now let’s talk about not so good advice. We hear this all the time that people share with friends and family that they have a serious autoimmune condition. And all of a sudden, everyone’s an expert. What is the craziest advice you ever received from a non expert about treating your condition?
Jonathan Arora 22:45
Oh, that is a good one. That is a good one. I love my armchair experts, I would say, “Have you ever tried opening a can of I forget what fish it was, it was a canned fish? And have you ever tried just putting direct fish oil on your skin?” So just going to the supermarket opening a can of mackerel or whatever, and spreading that on your skin? I remember that was at a party and an aunt of one of the party who had done that and it cleared up her skin?
Angela Degrassi 23:17
Well this episode now needs to come with a don’t try this at home warning. How would you respond to advice like that?
Jonathan Arora 23:25
Yeah. So that’s one of the things that has always kind of plagued me wherever I would go up at a social event and someone would come up and you know, you’ll get remarks about oh, what’s that? What’s wrong with your arm or what’s wrong with your leg and you get advice like that. And but when I was younger, it wouldn’t visibly make me annoyed. I’m not gonna lie. It’s not something you want to be called out about. You want to blend in with the crowd. You don’t want to feel like you’re special, or you’re different in any way. Later in life, you know, it’s one of those unfortunate things that that you have to deal with. And one of the things I’ve learned and adopted as far as my philosophy is, you don’t have to listen, you know, they can give you that advice. But you’re under no obligation to take that advice. Seriously. You’re under no obligation to try that advice. You’re also no under no obligation to make them feel good about giving the advice you know, people pleasing has been one of my things I’ve been trying to work out in my life and you can be polite, you can be not polite, it’s up to you. The one thing I found what works for me is you can politely excuse yourself from the conversation and but you don’t have to let that advice live in kind of your brain, you can make a conscious choice not to listen to that advice, and to me, that’s the best advice I would pass on to how to deal with that.
Angela Degrassi 24:32
I really liked that answer. Yeah. So hear that everyone. You don’t have to listen. And it’s your choice with how you respond. All right. So as we wrap up this episode, can you share a secret that you would only tell members of the psoriatic arthritis club or those who may become part of the club?
Jonathan Arora 24:51
One secret or one thing I would say is you deserve kindness. You deserve space to deal and handle with the condition and if you need to take a day off of work if you need to not go to a friend’s party or some kind of event that you feel like you have to go to because you’re not feeling up to it, you know, I spent a lot of time then that base up, oh, well, I have to go don’t want to not be normal and whatever. But you know, you deserve kindness and you deserve any kind of special care and extra care that you need. So my secret is, put yourself first, do what’s right for you, you know yourself better than anyone else. So be kind to yourself. Don’t be afraid to ask for help and put your needs first and pay attention to your needs are important.
Angela Degrassi 25:38
Thank you for that. John, you have a really valuable perspective. And I hope our conversation inspires a more inclusive dialogue about living with psoriasis and psoriatic arthritis.
Jonathan Arora 25:49
No problem. Thank you very much for having me.
Angela Degrassi 25:53
That’s it for The Psoriatic Arthritis Club. Thanks so much for listening. And we hope that John’s story will inspire you along your journey. And if you haven’t already, make sure to check out our first season where we’ll share more incredible stories that inspire and touch the hearts of our community. You can find all episodes on our platform. This podcast was made possible with support from AbbVie. For more information and stories from other PsA patients like you subscribe to The Psoriatic Arthritis Club or visit psoriatic arthritis club.org. You can also visit CreakyJoints.org for the latest information and news about living better with PsA. If you like what you’ve heard, be sure to rate our podcasts, write a positive review, and spread the word by sharing with your friends and family. It’ll help more people like you find us.
Narrator 26:43
Be inspired, supported, and empowered. This is the Global Healthy Living Foundation Podcast Network.
Episode 3
Dr. Ruderman on Collaborative Care and Individualized Management


This episode features rheumatologist Dr. Eric Ruderman discussing PsA management, patient-doctor collaboration, and individualized treatment. He delves into lifestyle factors and the latest PsA research and treatments.











Episode 3 - Dr. Ruderman’s Insights: Collaborative Care and Individualized Management Strategies for PsA
Narrator 00:00
Be inspired, supported, and empowered. This is the Global Healthy Living Foundation Podcast Network.
Dr. Ruderman 00:06
The most gratifying thing for me and one of the challenges, admittedly, that we have in this field is that I don’t have a great way to decide if any given medication that I recommend to a patient is going to work or not. It’s very much trial and error. We don’t have any way to test that in advance. But when it does work, that’s one of the most gratifying things people come in and they say, you know, we made that change a couple months ago, and four weeks, six weeks after that, I noticed I was feeling a ton better. I was able to do more, I was able to spend more time with my family. Those are the kinds of things that I find people can do.
Angela Degrassi 00:45
Hi, I’m Angela Degrassi, and I’m the host of The Psoriatic Arthritis Club, a podcast from CreakyJoints and the Global Healthy Living Foundation, where we explore the ups and downs of managing and treating PsA, which for the uninitiated, is an abbreviation for psoriatic arthritis. In this episode, we hear from Dr. Ruderman about an aspect that’s crucial to every patient’s journey, the relationship with their health care provider. Together, we’ll explore the most effective ways to work with your doctor, how to communicate your concerns, hesitations and hopes, and how to actively participate in decisions that could shape your treatment and ultimately your quality of life. Dr. Ruderman will also be answering questions from our patients from our first two episodes. Dr. Ruderman is a renowned Professor of Medicine and the Associate Chief of Clinical Affairs in the Division of Rheumatology at Northwestern Feinberg School of Medicine. His clinical focus is on rheumatoid arthritis, psoriatic arthritis, and spondyloarthritis. Dr. Ruderman, thanks for returning for the second season of the podcast. Can you tell our listeners a little more about yourself?
Dr. Ruderman 01:56
Sure. Hi, everybody. My name is Eric Ruderman. I am a rheumatologist at Northwestern Medicine in Chicago Northwestern University. I’ve been there for a bit more than 20 years. My practice is clinical rheumatology, and more specifically, I’ve had an interest in worked in psoriatic arthritis. For many years, we have run a combined clinic with a dermatologist and myself to manage psoriasis and psoriatic arthritis for the better part of 20 years now.
Angela Degrassi 02:24
Wow, that’s interesting. I can see how that background makes you a perfect guest for The Psoriatic Arthritis Club. So you mentioned you have dermatologists working alongside of you. What is the trickiest part about treating skin and joint symptoms?
Dr. Ruderman 02:38
Well, I think that the tricky part is recognizing that different aspects of disease are important to different patients. And the way we try to think about it is that the people who come to see us in that clinic are the people that I see in my practice, otherwise, have psoriatic disease. Some of them have joint symptoms. Some of them have tendinitis, some of them have bad skin disease, some of them have nail changes, some of them and may have back involvement. And regardless of what’s going on, it’s all part of the same disease. And one of the more challenging parts of the management is trying to work with the patient to figure out what issues are most important to them. For some people, it’s the skin disease. For some people, it’s the joint disease, part of my job as a physician and as a rheumatologist is to make sure that they’re thinking about all the implications. So somebody may say that joint disease doesn’t bother me too much. But I may say, well, but down the road, you’re going to regret that and say, Well, I wish we had done more, because you may be faced with damage to your joints that we didn’t address early enough. Similarly for skin disease. So it’s really a coordinated effort. And particularly in this clinic, it’s a coordinated effort between myself, the dermatologist and the patient to try to figure out what’s the best management strategy for that particular person taking into account all the aspects of disease that bother them the most.
Angela Degrassi 03:58
That’s great to hear. So it sounds like it’s really important that you collaborate with your patients based on what they find important based on the symptoms that they experience and really impact their life.
Dr. Ruderman 04:09
Absolutely. I mean, we talk a lot in medicine these days about shared decision making and collaborative care. But this is one of the places where it’s hugely important because there’s just so many different aspects to consider.
Angela Degrassi 04:21
And psoriatic arthritis is a condition that people live with for a very long time. It’s not uncommon for people to switch treatments several times throughout their life. How do you motivate patients to switch treatment when it’s no longer working? And what signs usually tell you that it might be time to make a change?
Dr. Ruderman 04:41
It’s a great question, Angela. It’s different for different patients. So number one, I don’t always have to motivate people. Many people say to me when they come in, this isn’t working for me, I’m not doing as well as I was or I’m having these issues that I wasn’t dealing with before. And maybe it’s time to make a change it depends on what aspects are going on. So we may have somebody who has pretty solid control of their skin disease and pretty good control their joint disease, and they come in and say, you know, my joints are still doing great, but my skin has been getting a lot worse in the last six months, what can we do? Or the opposite, they may say, my skin has been well controlled, but I’m having more and more joint pain. And for treatments that are intermittent, they may say, well, it’s not lasting as long as it did. And I’m starting to flare before I’m due for my next shot, or my next infusion or whatever it is that they’re being treated with. And so all of that gets kind of rolled into the discussion to say, okay, what’s not going well, what do we need to address? And can we do that by in many cases, tweaking what we’re doing now, if we adjust the dose of your medicine? Can we add something else to get that extra little bit? Or is it time to make a change altogether? And the challenge when you make a change is there are no certainties in this disease. And so I can switch to another medication that I would say, well, that’s likely to work better. But I don’t know that for sure. And there’s no good way to test that in advance until we start the medicine and see if it works. And so sometimes those are challenging decisions. And it really comes down to a real discussion between myself, the dermatologist, and the patient to figuring out what’s the best approach for them.
Angela Degrassi 06:18
Right. That sounds good. And I know that there’s so many things to be taken into consideration when someone is deciding what medication to take. What would you say to a patient who’s hesitant to try a treatment out of fear of side effects?
Dr. Ruderman 06:33
Yeah, that can be a challenge. And I think what helps is to talk through the potential side effects and to talk through the real risk of those side effects. So one of the problems is people may see a medication advertised on TV, for example. And you know, at the end of all those commercials, they list all of the really horrible things happen when you take the medicine. And the problem is they’re not listed in any sort of context. It’s what the narrator will say, and we have to warn you, if you take this medicine, you could have ABCDE, and F and possibly even death. And the answer sometimes is that well, those things are possible, but they’re really unlikely. And so one of the things we talk about is what’s the true risk of those side effects? How likely is it that any individual patient is likely to have any of those problems? And more importantly, can we identify that when it’s starting to happen, and that’s a big part of the discussion to say, here are the risks here are the possible side effects. But it’s not like all of a sudden, you’re gonna go from zero to 60, and then one day and be totally fine. The next day, you’re going to be flat in bed with all these problems. So a lot of times we talk about, well, what are the warning signs? What are the things we can look for? What can we monitor lab tests, things like that, to say, well, the side effects are maybe starting, and maybe we need to adjust the dose or thinking about switching meds. So it’s really a discussion about what’s the real risk? And how likely are these things to happen?
Angela Degrassi 07:53
Very good. We know that face time with your doctor can be short, and you can wait months for an appointment. And then it goes by very fast, what are some key things that you would like patients with PsA to know about making the most out of their limited time with their rheumatologist, so tell us if there’s anything they can do to prepare for an appointment, or any information that they can share with you that you find helpful.
Dr. Ruderman 08:18
I think they go hand in hand. And so I think to make the most of the appointment, and as you said, the appointments can be short, they may be far apart. So it’s often helpful for a patient to think about what’s going on the day before to take a few minutes and think about how have they been doing? What issues that they’ve been having? Are they having more symptoms that they weren’t having previously? What are those symptoms? Are they joints are they skin? Are they back problems? Whatever it is, think about any side effects they’ve been having. Think about the medicine that they’re taking. Is it continuing to work consistently? Or are they going up and down? Are they having flares? When they’re due for a dose? Does it work as well as it did previously? Those are the kinds of things that are helpful to come in with because then I know from the beginning, where are we starting from. What’s happening? What’s the current situation? Those are the questions I’m going to ask anyhow. But it’s often helpful if people think about in advance, because then you don’t forget about it. I mean, what happens a lot is we go through a whole visit and somebody says, oh, you know, I forgot to tell you that I’ve been having this particular issue. And then we gotta go back. And maybe that was important as we were making some decisions earlier in the visit, or worse, they leave and they remember something the next day and they say, I wish I told them that and then they’ll send me a message. But at that point, it’s not the same as sitting there in person and working together to address what’s going on. So I think mostly, it’s really about preparing ahead of time, but just thinking about what’s your current state? What’s happening? Is the medicine working? Are you having any side effects? Do you feel like your disease is being adequately addressed? Or do you feel like there are parts of it that aren’t being addressed and those are the things we want to focus on during the visit?
Angela Degrassi 10:01
That’s really helpful. I know that all of us are really susceptible to forgetting things, even if they are really important in the moment, you just might not be thinking about it. Actually, at GHLF, we have created an arthritis registry that’s also an app where patients can track their symptoms and treatments, then share reports with the rheumatologist. It’s called Arthritis Power. Would you find something like that helpful from your perspective as a rheumatologist? If someone came in that showed, for example, you know how well they were sleeping and you know, when they had a flare and what those symptoms were, if you saw items like that over time in a nice little report, would that be something that might be interesting to you?
Dr. Ruderman 10:46
That sort of thing is very helpful to know what’s been happening. Remember, I may see a patient every three months or every six months. And it’s hard sometimes, because even if they’re preparing for the visit, as we just talked about, recall isn’t great. And so people might think about how they’ve been doing in the last two weeks, but maybe two months ago, they actually had a bad time, and they didn’t get a chance to let me know, and things are settled down. But I need to be aware of that. Because it really affects how well I think they’re doing with their treatment. So an app like that, that tracks all that is great. I don’t know that it’s critical to say, well, on Tuesday, I was this on a Wednesday, was this on Thursday was this you know, that sort of very granular level. But the big picture level of you know, are you doing well? Are you having periods when you’re not doing well? Are you having periods when you’re doing better? And importantly, what’s different at the times when you’re not doing well? Did you miss a dose? Did you change a medicine recently, and it wasn’t working as well for you? Did you add a different medicine for another disease that might be interacting with what you’re taking for your arthritis, those are all really important and to get them down in an app like that is helpful. If you’re a note taker, that’s something you can just take notes on. But those pieces of information about what happens between the visits can be very useful in making the right decisions in terms of managing disease.
Angela Degrassi 12:03
Those are great questions to ask yourself to measure how you’re doing. Managing your condition is an individual journey and what works for one person, might not work for another. For example, take things like diet and exercise, are there lifestyle changes that you might suggest to patients with psoriatic arthritis that they might practice and their day to day life that could complement their treatment? And lifestyle changes could include anything that deal with nutrition, sleep, movement, or mental health?
Dr. Ruderman 12:30
Great question, Angela. I think that yes, all of those things come into play. Physical activity is hugely important. So people talk a lot about exercise, I try to focus more about being active. For some people exercise is kind of a scary word. And I don’t always necessarily focus on saying you have to get this many minutes or hours of exercise in a day or a week, but more that you’re staying active stay continuing to move, continuing to use your body. One thing I do find for some people, not everybody, but for some people, there’s a concern that if they are active, they may cause more damage to their joints. And I really try to stress with people that there’s very little that you can actually do physically, that’s going to make your psoriatic arthritis worse, it may make symptoms a little bit worse. And you may have to modify the kinds of activity you do if it’s aggravating some of your symptoms, or if it’s aggravating one particular joint, but you’re not going to really cause damage to that joint that you need to fear that being active is something you will regret later and it actually is more helpful than harmful. Other things, sleep is really important. Getting good regular quality sleep certainly impacts a lot of the disease certainly impacts a lot of the pain that people have. Diet is a little bit more challenging. I think it’s important to get a good balanced, healthy diet that certainly keeps you healthy in many ways. There are aspects of diet that may impact psoriatic arthritis or other types of arthritis. The challenge is that that is probably very individual. And there is a lot of work going on right now trying to understand the role of diet and psoriatic arthritis and whether certain foods make things worse, certain foods make things better. I try to steer people away from a particular diet that you know, has been said works for everybody because nothing ever works for everybody. And so if there are foods that make your symptoms worse, then it makes a lot of sense to stay away from those things. If there are foods that seem to make you feel better, those are fine. Weight loss. Getting to a good healthy weight is very important. And there is some research and some data in psoriatic arthritis that says losing weight can improve symptoms. It makes some sense the more weight you lose, the less stress you’re going to put on your joints, so they won’t bother you as much. But I don’t focus on it to the point of making people feel bad about their weight. I don’t want people to feel like they’re not doing what they need to do, but I think it can become an important part of the overall management of your disease and managing all the symptoms that you have.
Angela Degrassi 14:58
Right and we know that being active is something that people want to get back to getting back to activities they might have done before. But we also know that PsA comes with symptoms such as fatigue and joint pain. What would you say to someone that has concerns or challenges with those symptoms that get in the way of activity?
Dr. Ruderman 15:17
That’s a great question. And I think the first thing I tell people, especially if they haven’t been very active, is to start slow. I can’t tell how many times I’ve had patients come in and say, I started a new exercise program, but I quit after three days, because the next day I was miserable, and I couldn’t get out of bed. And then when I break down and say, w3ell, what will you do and all of a sudden, you’re doing an hour of vigorous exercise a day when they weren’t doing anything before. And it makes sense that they’re going to feel worse. So if you haven’t done a lot of exercise, if that’s not part of your routine, it’s important to add it. But it may be as simple as don’t start walking five miles a day, if you’ve never been walking, start by walking around the block twice, and make sure that goes okay. And then a little longer the next day and try to build up to where you need to be fatigue is a challenge. And there’s no question that people have a lot of fatigue, especially when their diseases very active. One of the things that definitely impacts fatigue is the amount and the quality of sleep that you get. And physical activity actually helps that so people who are more active, get better sleep at night, and they’re potentially less fatigued the next day, it can sound a little counterintuitive. The more you do, the less fatigued you are. But in fact, that’s what happens in the real world. The more active you are, the better you sleep at night, not necessarily so much in hours, but the quality of your sleep, and you’re going to have less fatigue the next day and be able to do more the next day. So I think the keys are staying active, don’t do too much too quickly. So whatever changes you make, do them slowly and focus on a balance between activity during the day and getting good solid sleep at night.
Angela Degrassi 16:51
That’s really great advice. I like that. What are some changes that you’ve seen in patients who have started medication for their first time, and what has this medication allowed them to do?
Dr. Ruderman 17:03
You know, it depends on the medication. The most gratifying thing for me and one of the challenges admittedly was that I don’t have a great way to decide if any given medication that I recommend to a patient is going to work or not. It’s very much trial and error. We don’t have any way to test that in advance. But when it does work, that’s one of the most gratifying things and people come in and they say, you know, we made that change a couple months ago, and four weeks, six weeks after that, because it’s never overnight. But after a few weeks, I noticed I was feeling a ton better, I was able to do more, I was able to spend more time with my family, I was able to go to my kids soccer games that I couldn’t do before because I just didn’t feel up to it. Those are the kinds of things that I find people can do, it’s not so much saying they don’t come back and say, oh, I suddenly ran a half marathon last week when I wasn’t able to walk six months ago. But more like I can do the kinds of things in my life that I really want to do every day. And I just didn’t feel up to it because arthritis and now that it’s controlled, I can get back to those things.
Angela Degrassi 18:06
And those are gains that we know are really important to people is just really being able to live their life and participate in their usual daily activities without pain and without major fatigue.
Dr. Ruderman 18:19
Absolutely. These days, you know, when I see somebody for the first time, or when I start working with them to try to find good treatment for them, I can tell them that my goal is to make you feel like you don’t have this disease. I mean, you still do. I mean once you’ve got psoriatic arthritis, it’s with you. It’s not we don’t have a cure yet, we can’t make it go away. But my goal is to get you to a point where you don’t feel like it’s part of your life anymore, that it’s well controlled with the medication and you’re back to what you used to do before the arthritis got in your way.
Angela Degrassi 18:51
I imagine that must be something really comforting for a patient to hear in your office. I really like that thank you for sharing. Are there any other therapies or non pharmaceutical treatments that you would recommend to a patient with PsA?
Dr. Ruderman 19:07
It depends on what else is going on in their life. But I think for some people and not for everybody, but for some people physical therapy can be very helpful, particularly for people who’ve been relatively sedentary or had challenges doing the things they want to do because their arthritis has been so active. A lot of times people come in and ask me about physical therapy. And the first thing I’ll tell them is I don’t want to do that until we can get your disease under control, because then you’re pretty much wasting your time you’re spending time with a therapist trying to do all this exercise, but you’re hurting so you can’t really do it. So our first focus is getting disease under control as much as we can. But at that point for many people who’ve been pretty sedentary haven’t been terribly active. Sometimes spending some time with a physical therapist is what it takes to get them moving again. Some people do it very well on their own and they say you know I don’t need that I’m okay I know the kinds of things I need to do. Well, I’ve done it before I’m gonna get back to it. But for many people working with a physical therapist is a good way to kind of get back to the kinds of activities that you used to do, but haven’t been able to do for some time. And sometimes it takes the barriers out of the way to getting there.
Angela Degrassi 20:14
Great. So physical therapy, that is something that you would suggest to someone with PsA. Thank you. So we have one more question. What is something that you wish all PsA patients knew about living with this condition?
Dr. Ruderman 20:29
That’s a really good question.
Angela Degrassi 20:30
I hope I didn’t stump you.
Dr. Ruderman 20:32
No, no, I guess probably my answer to that question is, they need to know that everybody’s individual, and perhaps in many ways more so for this disease, that a lot of the other things I see in rheumatology, where the problem is just joints here, it’s joints, it’s skin, it’s tendons, it’s lower back, it’s nails changes. And I think people say, well, how do people usually respond? Or am I responding the way most people do? And the answer is, there are no most people, everybody’s individual. And I want people to know that they need to think about their disease, they need to think about how it affects them personally, what issues they struggle with, and focus on addressing those rather than trying to think about what’s the one treatment that’s going to work for everybody, because there is no treatment that works for everybody. And I think the corollary to that is once you understand that, I need people to sometimes be patient, because not every treatment is going to work when we first started. And sometimes it may take two or three tries. I wish it didn’t I wish we had a good way to decide upfront which treatment is right for which patient but because we don’t, sometimes it takes two or three tries to get it right, we almost always do. And that’s another thing I want people to know is that stick with it, it’s unlikely that you’re going to be faced with a situation where you just can’t get better. But sometimes it may take a little while to find the right balance for you the right medication or combination of medicines that are going to get your disease under control, and make you feel better and get back to your life.
Angela Degrassi 22:04
That’s so true. We’ve had patients tell us that they blame themselves when a treatment stops working. Can you reiterate that it’s not their fault if a treatment doesn’t work?
Dr. Ruderman 22:14
Absolutely not. I mean, that’s the problem. We don’t know how to decide which treatment is going to work for any individual patient. We have clinical trials, whenever any drug is approved, there’s a clinical trial. And the outcome of the clinical trial typically says, well, you know, 60% of people who were on the medicine did better and only 10% of the people were on placebo. So that sounds great but that’s 60%. It’s not 100%. So not everybody is going to respond to every medicine. And it’s not your fault, not anything you did wrong. It’s just the response is individual and what works for one person may work less well for somebody else. And it really just becomes a challenge to sort of work through the options and come up with the ones that are going to work for you.
Angela Degrassi 22:55
Before we conclude our other guests on the podcast that you may have heard in episode one and two, Ashley and John, both have questions for you, Ashley, go right ahead.
Ashley Krivohlavek 23:05
So doctor, I am wondering if there is any upcoming research or treatments that are being pursued specifically for the inflammation aspect in the joints for psoriatic arthritis. And I’m not looking for an overall body suppression. I’m looking for something very targeted to the psoriatic arthritis.
Dr. Ruderman 23:29
That’s a great question. Ashley. Honestly, though, I do think it goes hand in hand. And when you have psoriatic arthritis, you don’t just have inflammation in your joints. It is your whole body it is a systemic disease. And while there are some medications that specifically work on joints, many medications work on the way that disease affects you more globally. And that’s not always a bad thing, if there are medications that have few or a reasonable amount of side effects. So there are a lot of upcoming therapies. And one of the nice things about a lot of the treatments we’ve had, the ones that have come aboard in the last 10 or 15 years is that they seem to work very well for both skin disease and for joint disease. A lot of the research now is focused on trying to find the right treatment for the right person, there are some things that work better for joint symptoms and some things that were better for skin disease and trying to identify which of those are going to be better for anybody in particular. And so there are new targets coming out new things to target to try to treat the disease. There are new ways of choosing the right treatment for the disease. And increasingly, we’re beginning to look at combinations of treatment, but not just in the way we’ve done it in the past, which is to say, well, this drug isn’t working. So we’ll add this other drug and see if now things are better. They’re much more tailored combinations, thinking about using combinations of medications that work together to give you a better response than either one would individually. So I think those are the things things that are coming in line. And we’ve made huge strides in managing this disease in the last 20 years. And I think the next 10 or 20 years, it’s going to be a whole new world as well.
Angela Degrassi 25:10
Ashley, always ask such great questions. And that was a really good answer. Now, our guest John has a question that may be a common concern among patients who may experience a decline in effectiveness of their treatment plan. John, what is your question for Dr. Ruderman?
Jonathan Arora 25:26
Hi there, the question I have for you is for patients that maybe on a treatment plan that is, you know, losing its effectiveness, maybe the symptoms are coming back or, you know, worsening and you know, there is a concern, there may need to be a medication switch. What is your strategy in handling that situation? And what’s kind of your plan treatment wise to address that?
Dr. Ruderman 25:50
That’s a great question, John. And I think that the way I approach it, first and foremost, is to recognize that there’s no right answer. So if somebody’s not doing well, there are a number of things we can do. And there’s no single thing, that’s the best thing for everybody, or even for any individual patient. There are always options. There are always choices. And so if I have a strategy, the strategy is to engage the patient to talk to them about what isn’t going well, what would they like to see improved, and then talk through options. Sometimes the option is to add something else on to what they’re taking now. For example, if I have somebody who has had bad psoriasis in the past, but their skin disease is very well controlled on the current regimen and their current medication, but their joints are doing worse, before I switch altogether, we talk about what can we add, that’s going to get their joints under control while still maintaining control of their skin disease. If the joints and the skin aren’t doing well, then we start to talk about well, what could we change to, to address everything. So there are always choices. And the choices range from making minor changes to try to add something on, to saying, well, we need to start all over and try another medication to see if that works better for you. It’s always important to go into that with eyes open. And there are times when it’s clear, you have to make a change, things are just not going well. You’re just not feeling well. And we need to come up with a different option, a different medication. But sometimes you’re almost there, you’re 90% better. And then I do worry. And we have this conversation, I do worry that if we make a switch, perhaps you’ll actually do worse because the new medication may not be as good as what you’re on. And those are the scenarios where maybe adding something or making slight changes in dose might be more effective or more appropriate than making a wholesale change of medicine. So I guess the best strategy is conversation and making sure that we’re making decisions that really are the right decision for that particular person.
Angela Degrassi 27:51
Dr. Ruderman I really love how you always interject with some kind of collaboration with the patient. So I think that really means a lot to a lot of people that their individual circumstance and their past medication history and symptom history is always taken into consideration. It’s really great to hear and also very comforting.
Dr. Ruderman 28:12
I’ve enjoyed talking to you, Angela and I think that what you said is absolutely right. The treatment of psoriatic arthritis and psoriasis in general is a collaborative effort. And part of that collaboration is myself as the rheumatologist, the dermatologist who’s involved in the patient, and no single one of us is really driving the decision making the three of us have to really coordinate to make sure that we come up with the best approach.
Angela Degrassi 28:38
Thank you for all those fantastic answers. That’s it for The Psoriatic Arthritis Club. Thanks so much for listening, and we hope you enjoyed hearing from our guests Dr. Ruderman. And if you haven’t already, make sure to check out our first season where we share more incredible stories that inspired and touched the hearts of our community. You can find all episodes on our platform. This podcast was made possible with support from AbbVie. For more information and stories from other PsA patients like you subscribe to ThePsoriaticArthritisClub or visit PsoriaticArthritisClub.org. You can also visit CreakyJoints.org for the latest information and news about living better with PsA. If you like what you’ve heard, be sure to rate our podcasts, write a positive review, and spread the word by sharing with your friends and family. It’ll help more people like you find us.
Narrator 29:29
Be inspired, supported ,and empowered. This is the Global Healthy Living Foundation Podcast Network.
SEASON 1
Episode 1
Lauren’s Story: A Personal Trainer Who Won’t Push Through the Pain


Imagine exercising for a living, then being diagnosed with a condition that makes picking up weights almost too painful to bear. When Lauren was diagnosed with PsA, she had a lot of concerns about what it would mean for her professionally (as a trainer) and personally (as a mom). “As a personal trainer, I have to live the lifestyle that I preach,” says Lauren. “If I am flaring, it is hard, and I have to really listen to my body.”











Episode 1: Lauren’s Story: A Personal Trainer Who Doesn’t Want to Push Through the Pain
DK – Deanna Kizis
LS – Lauren Scholl
ER – Dr. Eric Ruderman
DK – Hi, I’m Deanna Kizis and I’m hosting The Psoriatic Arthritis Club, a new podcast from CreakyJoints and the Global Healthy Living Foundation. It’s about the ups and downs of managing PsA, which for the uninitiated, is an abbreviation for psoriatic arthritis.
So before we get started, I have a confession to make. Even though I was diagnosed with PsA more than two years ago, I’ve barely talked to anyone else who has it.
That’s weird, right? Especially when you consider that I’m an author and a journalist and I’ve literally interviewed hundreds of people over the years.
I don’t know exactly why I haven’t sought out other PsA patients, but I suspect I’ve been in a little bit of denial about having this disease. But, you know what? It’s time. I need help and I need support, and I’m pretty sure that if you’re listening to this, you do too.
In this podcast, I’ll be talking to other people with PsA about what they’ve been through and how they’re coping. We’re gonna talk about things like, what’s working? What isn’t? And I’ll be sharing insights and perspectives from top rheumatologists.
Look, I’m not giving out medical advice here. I’m not a doctor; I’m a patient just like you. But I’m going to share what it’s really like to live with a condition that most people have barely heard of, let alone truly understand.
I mean, when I found out that I had PsA, I barely had a basic grasp of what it was. I didn’t know how debilitating it could be, or how much it could affect me beyond the pain that seemed to come out of nowhere or the psoriasis on my skin. I didn’t know about the brain fog. I didn’t know about the fatigue. I didn’t know about the medications and treatments. Seriously, I had no idea.
And it turns out that we have a lot to deal with.
That’s where this podcast comes in. I’m learning that having a support system is one of the most important things you need after you’re diagnosed. None of us has all the answers. PsA is complicated and it affects everyone so differently. But my hope is that we can talk it out and learn from each other.
So let’s get going.
For today’s show, I spoke with Lauren Scholl, a working mom from the suburbs of Chicago. Her story really resonates with me for so many reasons, including that we’re both managing PsA while parenting young children.
What I found with my daughter, we’ve come up with, kind of a system for that 4 o’clock, just fatigue, where we call it quiet time, and she brings her book or her coloring pages or whatever it is on the bed with me, and lets me sleep and just get super cozy.
LS – That’s so sweet. I wish my two little boys would give me some quiet time, that would be amazing.
DK – Lauren is 33 years old, married, and a mom of two boys age 5 and 7, while my daughter is 8. By the way, Lauren is also a personal trainer, which is something we definitely do not have in common.
Tell me how your diagnosis came about. Did you start with symptoms? What were they?
LS – I was diagnosed about four and a half years ago. And I was convinced that I injured myself working out, it got to the point where I really couldn’t walk. I was a former professional dancer, instructor, competitive dancing, which was hard on my feet. And so I had noticed my pain often happened mostly in my toes. And so when I got to the point where I could not walk, I went to see a podiatrist who saw extensive arthritic patterns in my joints, and then he noticed that I also had psoriasis patches on my knees and on my ankles. And he asked if that had been a thing. I said, “Oh, yeah, I’ve had it for seven years, eight years.” And he was the one who sent me to a rheumatologist, you know, to explore things further because he did say “it does look like this could be a psoriatic arthritis-type diagnosis, but I’m not a rheumatologist.” So that’s how I got here.
DK – I totally get it. My symptoms also started actually in my foot. And the top of my foot would just would, like this tiny part of my foot would swell up, it was the most bizarre-looking thing, and I couldn’t wear normal shoes anymore. I had to run around in flip-flops. And thank God I don’t live in Chicago, or that that would have been a nightmare, so you can get away with that for a really long time. So how did you react when you got this diagnosis? I mean, most people don’t even know what it is. I didn’t.
LS – It was tough for me because of the lifestyle that I live, I was afraid. You know, what does this mean for my training? What does it mean for day to day? Does this mean that I’m just never going to get better?
DK – So your job is to be a trainer, how has that affected your life?
LS – It’s hard because my job is bending over and picking up weights and demoing exercises and things like, a reverse lunge, where you have to step back and really bend the toes. I mean, there are days where I can’t do it. I can’t demo that for someone. So I have to use my words. I’ve tried to learn ways to work around it, I’ve changed my training style, and I feel like as a personal trainer, I can’t just tell people to work out, right? Like I have to live the lifestyle that I preach. I’ve talked to my doctor on multiple occasions, she said that exercise has been recommended to help fight the fatigue and help keep people moving. So, finding that balance, for me, has been a really key piece to living with psoriatic arthritis, because that activity I’ve found to be something that I need to keep me going. However, if I am flaring, it is hard, and I have to like, really listen to my body and know what I can handle.
DK – Can you walk me through, just when you went to your doctor, how it went. You walk in there, you go to your rheumatologist, they give you your diagnosis, and did they put you on a medication? How did that work out, because some people have to kind of, you know, try different things before something works.
LS – We tried multiple biologics and just couldn’t get my inflammation markers to come down. I was still flaring, at least, like one to two times every month, where I would be on a steroid pack or something like that, just to try to help with that inflammation, after–
DK – What kind of symptoms do you have, what is going on?
LS – So recently, I’ve been having flare-ups in my hands, which is kind of new for me, it hasn’t been, my hands have not been the most affected. I noticed that if I go to a doctor’s appointment, I can’t get through, like, filling out an intake form. By mid-page, my hands are just tired and not working, and I can’t grip my pen right. I’ve had like really bad swelling within my knuckles.
I was back there this week, because the swelling came back and my hands wouldn’t open and close again. So we went through the ultrasounds and the bloodwork, and it looks like they’re probably going to have to change me to something that will hopefully work a little bit better.
DK – What do you have to say about talking to your doctor? Has that been something that you’ve been able to communicate with your doctor easily? Or did you have to work to really report your symptoms?
LS – The first rheumatologist that I saw, I don’t feel like she had the sympathy towards, like, or empathy, I don’t think she felt the pain. There were days where I’d go in there on crutches because I couldn’t walk, and she’s like, “I’m sorry, there’s nothing we could do for you. You tried the steroids, and you–” and I’m like, “I can’t walk. I can barely drive here!” When it got to a point where it was so, my pain was so bad, I went on Facebook, because that’s the place you go for everything. And I asked my friends, does anybody know a rheumatologist? And so someone referred me to the rheumatologist that I see now. She is phenomenal, and very easy to talk to.
DK – Well, you found the right doctor. And I personally feel like that is half the struggle.
LS – So when I talk to my doctor or my rheumatologist about medication I feel like she really listens to me, I’ll tell her kind of how I feel on the medication. And she, she hears me and she’s ready to, like, pivot and try the next thing, and she just assures me that with every medication that we have tried, that we’re learning a little something new so we can kind of continue to move on. And she just has assured me that we are definitely not at the end of the road here, that there are lots of opportunities to find something else that will work.
DK – Even though Lauren is clearly struggling, as I am, to find a treatment plan that works, I found it reassuring to hear how she connects with her doctor and how they work together. Because for me, finding the right doctor has been a journey. For more on how to communicate better with your doctor, I talked to Dr. Eric Ruderman, a rheumatologist at Northwestern University in Chicago.
ER – It’s important to tell me what’s important to you. What do you want to get better? What are the things about your disease that need to get better? What are the things you want to do that you can’t do? That’s the functional aspects so that we can sort of make sure we cover that.
And then when we think about treatments, you know, what are the side effects that worry you the most? That may not be the most likely or maybe not even be the most worrisome, but for you, might be a big issue. You know, and it may have to do with somebody else in your family had a problem with one thing or another or some particular, you know, side effect from a medicine you had years ago, that was just a big issue for you.
So, you know, what are the concerns that you have, so that I take that into account as we start to think about medicines and walk through the options.
DK – Okay, so speaking of getting better, I also wanted to learn more about a term I heard recently, which is “minimal disease activity” or MDA. To be honest, I wasn’t exactly sure what it was, so Dr. Ruderman explained it.
ER – It’s the idea that, you know, whatever treatment we choose should take all the different aspects of disease, whether it’s your skin, your joints, your tendons, your nails, whatever it is that’s active, and control all of that. That’s the idea. That if we just stick to one thing, we really haven’t solved everything. And so the idea is to come up with a treatment plan, then maybe one medication, maybe several different things, if that’s what we have to do, that really controls all of the aspects of what’s going on.
It’s really, you know, in an ideal place, we would have all of the different things that go into psoriatic arthritis well-controlled so you don’t really know that you have them.
DK – I hesitated to ask Lauren about minimal disease activity, because she’s struggling with her symptoms. But her answer shed light on this whole other aspect of what it’s like to live with PsA.
I guess for me when I think of minimal disease activity, it means that I would have, all of my markers go down, or all of my symptoms would go down to a more manageable level. What do you think life would look like for you?
LS – So I have not been there yet. I have hope that I will one day. I know that for me, my psoriasis on my skin has never cleared up. However, it also hasn’t been my main concern to me; if I feel great, that’s what’s gonna keep, like, my first and foremost priority. But as a whole, we just haven’t quite gotten to that, to that place yet, where, well-rounded, I could say that minimal disease activity is happening, but I’m hopeful. I think that, you know, I think that as we continue to trek down this path, you know, a few even, I would love a few months of MDA, would be, sounds really, sounds really great to me.
The way I’m thinking of it is like, how would my, like would my personality change? Would it change me to be a happier person? I try to consider myself a pretty happy person as it is, I’m really grateful for all the things that I have, that have helped me along this journey, my parents have been extremely helpful with my kids, my husband has been so hands-on and supportive and helps take loads off of me. But I feel like it would make me feel a little bit more independent, like, the confidence in myself that I would feel, to be able to do things like, all, like a lot of frustration gets built up inside of me, because I feel like I should be able to do these things.
And I think that I would have — more so than being pain free — the energy to really enjoy and be in the moment with my family and like, really run around with the kids at the park and enjoy that, not like wonder when it’s gonna end. You know what I mean?
DK – I do.
LS – I think that’s probably, like, the biggest lifechanger would be to be able to be in the moment and enjoy it and live it.
DK – There are times when I’m going through my day, and I do this thing in my head, it’s like a conversation I have with myself, and it’s just like, next thing. Get through unpacking the groceries, okay, you did it. Next thing. You’ve got to do the dishes. Okay, next thing. Having to have that mindset, I find, is exhausting.
LS – Yes. To be honest, I feel like I get through the day to day, I go through those motions and I get things done the way that I would if I was any typical 33-year-old, but where it affects me psychologically and you know, mental health, again, it’s like that confidence. It’s like the inner joy being present, and confident. I think that’s a big thing.
DK – Yeah I do know. And I know for me that I had to really go through a learning curve with my daughter, because for a long time, I actually didn’t want her to know that there was anything wrong with me, and so I tried to hide it. And she, I think, actually just started to get concerned.
So what do you do with your kids? Because we can’t really hide this from them. Or maybe you’re doing a better job than I did.
LS – So my situation is a little bit different than yours; my 7-year-old was actually diagnosed with juvenile rheumatoid arthritis this past year. So we’ve had a lot of discussions. It was a really hard year for him, and it did open the door for us to really start talking about it.
I’m able to now say to him, “you know, when your feet really hurt, Owen, or you know when your knees are really bad? That’s how mommy feels right now.” So he really relates and understands. And my little one Carter is 100% a mama’s boy, and he just wants to take care of me.
And to be honest, I try not to let my pain or, like, the fatigue take away from the kids, because I feel like, at 5 and 7, all you want to be doing is exploring and running around.
What I find is that if I push through it, and I’m like, you know what, “let’s go on a walk or let’s be active or let’s go play,” at the end of the day, my feet are like pulsating. I’m in bed at like, 7:30, feet up, and I just, I can’t, like, it feels like I’m walking on bruises. And it’s, it’s your kids, right? Like, there’s nothing you wouldn’t do for them. There are days where I do that and I fight through that, and they’ll never know that or maybe they will way later on down the road.
DK – Yeah, I really get it. It’s such a fine balance, because I know for me that when I — it’s kind of like “gas, brake” for me — because when I push through it, which I do all the time, but there comes a point where I know I have to stop, because I’m gonna just be worse the next day and worse the next day. I get so upset when I make it to a point where then getting out of bed is hard. But you know, I think, as a mom, I really have to think about what I’m capable of, and also asking for help.
This is a hard question. This runs in your family. So for you, this is like a family disease? And is it both or one of your sons who’ve been diagnosed?
LS – So far, just one of my sons, however, my youngest does have psoriasis. So we’re keeping a very close eye on him as well.
DK – How are you coping with that?
LS – Not well. It’s been hard to think about knowing the pain that you’re in, and then having you see your child in that pain or thinking that like your kid is feeling the same pain that you feel is, like, gut-wrenching. However, I feel blessed in a way, of knowing that I can help them through it, because I’ve been there and I can relate and I understand and I know. I can advocate for them for school and things along those lines, for the accommodations that he needs at school.
DK – What I love is, is that what I was thinking when you were talking, is that they’re really lucky to have you as a mom. Because having a mom who can be empathetic, who can prepare, who can find the information, who can advocate. That’s a really special thing. But I can imagine that it’s really, really tough.
LS – It’s scary for me to think about the long road that they have ahead of them too. My grandfather had rheumatoid, my dad has autoimmune issues as well, on my dad’s side of the family, it’s extremely, it’s just heavy in their genetics.
So I definitely saw my grandfather deteriorate with rheumatoid arthritis. He was a physical therapist, he had to stop working, he had to stop golfing, he had to stop doing the things that he really loved.
So thinking about taking those things away from me is really hard. Even if it’s down the road, I’d love to see myself you know, you see on YouTube, those like 98-year-old women that are still like, teaching Zumba classes or whatever that might be.
DK – You know, what I want to know is, I mean, I have a couple of questions about, first of all, you know, you’re young, you’ve got obviously friends in your life, other people in your life, how, are they aware that you have psoriatic arthritis? How did you explain that to them? Because I find it really hard. People think I have just, like maybe like, granny-sore hands or something. And I’m like, no, it’s, honestly, it’s worse. But I don’t want to sound super complain-y either. So I struggle with how to talk to people about it.
LS – Yeah, it’s been hard for me, I have like one very close friend that totally gets it. She has been amazing and understanding. What’s hard is that as a mom, I’m meeting all these new moms at the kids’ schools, and it’s kind of been like, “oh, let’s go on this walk.” This group of moms is going to the beach, and they’re gonna go on, or they’re doing this run, right? and “you’re a personal trainer, you’d be really good at that.”
So it’s hard. It’s a struggle for me, because I don’t want to be like, “Oh, hi, I’m Lauren. I’m the one that has psoriatic arthritis, I’m constantly tired, and I really hurt all the time.” The last thing you want to be is like that whiny, that whiny person that’s new to like, the moms group.
DK – Oh totally.
LS – So with my close friends, my family gets it. I’m lucky because it’s heavy in our family, so like they really understand. My best friend gets it. She’s been there for me, when, to take my kids when I’ve had bad days. But new people? I hide it. You know? I don’t, it’s not something I talk about, unless it, you know, unless it would come up in conversation. And I’ll be honest, I try to fight through it and keep up with them, because I want to. You know? Like, the stuff that I want to do.
DK – I understand that. And by the way, no offense to grannies, I, you know, I’ll be a granny someday, so I will have granny hands. So, one thing I want to do in this podcast is get as much advice as possible from other people with psoriatic arthritis. I mean, I need all the help and good ideas I can get, and I want you to get them too. So here’s Lauren’s advice.
LS – My biggest piece of advice would be to listen to your body. When you feel like something’s not right, or you feel that you’re hurting. Take the time to rest when you need to, don’t wait for it to get worse, to ask for help, to go see, to talk to your rheumatologist and let them know what you’re feeling or to track it.
Something that I had to really, kind of develop, a new understanding for what does it mean to know my body, to know what I can handle, to know what I need when I’m in pain, to know when it’s time to call the doctor, getting to know those signs, and just, again, surrounding yourself with the people that are going to support you, that are going to try to understand — if they can’t physically understand — but try to understand what you’re going through. And advocate for yourself. The way that I advocate for my kids or the way that you ask for help from the doctor, those are probably the best, best pieces of advice that I could give.
DK – That’s amazing, Lauren. You’re so inspiring. Thank you so much. It’s been so great to talk to you.
LS – It was so nice to meet you. Thank you so much for having me. And you’re inspiring too, hearing your stories and stuff has been great.
DK – I hope you’re as inspired by my conversation with Lauren as I was. She’s dealing with so many moving parts as a young mom with a chronic illness. I mean, she has kids who have chronic illness, and she’s a personal trainer! But I love her ingenuity and spirit, and her willingness to do what it takes to make things work.
Anyone out there who’s parenting with this disease knows it’s a lot, so it was really helpful for me to hear what another mom is going through. We can’t give up, right? We have to be there for our kids, if we have them, and our loved ones in general. That’s why I think it’s so important to keep working and pushing forward to try to feel better. It’s not easy. We gotta dig deep. But I think we’re worth it.
That’s it for The Psoriatic Arthritis Club. Thanks for listening.
This podcast was made possible with support from AbbVie.
For more support and stories from other PsA patients like you, subscribe to The Psoriatic Arthritis Club or visit psoriaticarthritisclub.org. You can also visit CreakyJoints.org for the latest information and news about living better with PsA.
Episode 2
Diane’s Story: It’s Never Too Late to Start Getting Good Care


Diane should have been diagnosed with PsA well before she actually was. As a woman of color who grew up poor, she endured decades of inadequate treatment, misdiagnosis, and stigma. But she also learned a lot about how to turn things around and advocate for better care. “Someone told me a bunch of years ago, you have a voice, use it,” Diane says. “That had to be the best advice ever. Use your voice.”











Episode 2: Diane’s Story: It’s Never Too Late to Start Getting Good Care
DK – Deanna Kizis
DT – Diane Talbert
GW – Dr. Grace Wright
DK – Hi, I’m Deanna Kizis and I’m hosting The Psoriatic Arthritis Club, a new podcast from CreakyJoints and the Global Healthy Living Foundation about the ups and downs of managing psoriatic arthritis.
I’ll be talking to people living with PsA, sharing their stories, what they’ve overcome, how they’re coping, and what’s working for them, plus perspectives and insights from top rheumatologists.
I’m an author and a journalist who interviews people for a living, but the real reason I was so eager to get involved with this podcast is because I have psoriatic arthritis too — and I know I have a lot to learn about it.
In the two years since I got diagnosed, one of things that’s started to worry me the most is what will it be like to have this chronic disease for the rest of my life? I’m only 51 and I have an 8-year-old daughter, so there are a lot of unknowns for me. I want to stay healthy for her, and for myself.
That’s why I was so eager to speak with fellow PsA patient Diane Talbert, who’s been dealing with psoriasis and psoriatic arthritis for pretty much her entire life. She has been through so much, as you’ll hear, and she was really comforting and helpful.
Just a reminder, I’m not doling out medical advice here. I’m not a doctor, but there will be one on later in the show. I really think it’s important that those of us who have PsA try to help each other by sharing our experiences.
So let’s do it.
I want to know that. When I get to your age, what is gonna happen?
DT – You’re going to be, you’re going to be awesome.
DK – I am?
DT – You’re going to be awesome. Yes.
DK – Diane is 63 years old and she lives in Maryland. She’s married, has two sons and six grandchildren, and she’s one of the most positive people I’ve met on my PsA journey so far. But seriously, Diane has had it tough. Her disease went mistreated for decades and she had some early childhood experiences that must have been really hard.
That’s why I was struck by her resilience and the fact that she kept pushing for better care for her PsA.
DT – Well, I got psoriasis at the age of 5. I probably had it before that, but I remember it was my first day of school, when I went to school, they told me I couldn’t come in because I was covered from head to toe in psoriasis, and they thought I was contagious.
So I knew from that moment that I was different. I didn’t realize it before then, and all the other kids were wearing, you know, short sleeves and shorts. And my mother always covered me up in clothes because she didn’t want me to feel different or embarrassed.
I didn’t really feel out of place until maybe in my teenage years, and that’s when kids started pointing and staring and going, “ooh, what is that on you?” and you know, kids are mean, so they were saying mean things. And that kind of, you know, made me feel bad and very insecure in life.
They didn’t know how to treat my skin. Nobody had ever seen anyone with such a bad case of psoriasis, and when you would read about psoriasis in textbooks, there’s always flaky, white, and mine was not like that. I had dark purplish psoriasis. They just didn’t know how to treat me, so that was the problem.
DK – I’m so sorry. And what a terrible time to be, to be an adolescent, and going through something like that, where you’re already so self-conscious and trying to find your place in the world.
DT – I actually started having pain at a young age, but again, because nobody even heard of psoriatic arthritis. I started having symptoms that I remember most at the age of 25. And I remember I would go to my doctor, and I would tell them, you know, I’m having these symptoms of having pain in my body, I can’t lift my arms, can’t comb my hair.
I just started getting, like, stiffness in my, in my shoulders, there was pain in my hands and my knees. It was just pain all over. And I went to, to my doctor, and back then because they didn’t put, psoriasis wasn’t connected with psoriatic arthritis. So they just told me it was in my head.
So I went back to the doctor again saying I think this is arthritis. He goes “No, you’re too young to have arthritis.” He was kind of saying, stop over-exaggerating, there’s really nothing wrong with you. Just go get some rest, you’re too young to have this, have the pain that you’re saying you’re having.
This, this went on for years, this going back and forth to doctors that would give me medicines, the ones that would even give me pain medicine, but they would all say “there’s nothing wrong with you, you know, just like chill out.” So this, so I decided there’s nothing wrong with me, you know, maybe it is in my head.
DK – Oh my gosh, I hate this story.
DT – It got worse. And actually a dermatologist at the time says, “Why don’t you see a rheumatologist?” I didn’t know what a rheumatologist was. Go see a rheumatologist. So I’m 50 years old, I went to a rheumatologist who did extensive tests on me from head to toe. I mean it was just amazing, and he came back and he says, “Yes, you have what’s called psoriatic arthritis.” From that day on, we started treating me for psoriatic arthritis.
DK – Do you think that that had to do, anything to do with your gender? Or being a Black woman or any of those things?
DT – I believe, because I grew up on the wrong side of the tracks, I was a woman, I wasn’t very educated when it came to my skin, that they, they told me anything.
I don’t think that I would have suffered so much in my life if I wasn’t a Black woman, I think things would be different, and also, I believe that because I didn’t have the greatest insurance back in the day that I got low quality care. And I think that that’s something that we all need to talk more about is these disparities in health care, you know, we get overlooked a lot, and this is nothing new, it’s always been like this, you know. I went years taking treatment that didn’t work for me. And not one doctor said, “let’s, let’s do something different.”
DK – You’ve had all of this experience. And so how, is there a way to help other people in terms of, if there’s someone else who was listening to this? Who is a person of color, a woman of color? A person who doesn’t have a lot of money? What would you add? What would you say to them?
DT – That’s such a good question. For me pain is physical, pain is not something we dream up, it’s it’s really there, you know because nobody believes you doesn’t mean that it’s not there. I mean, having chronic pain affects your body, it affects your mind, your emotions, it affects your relationships with family and friends, and it’s just, you know, it’s something that we just have to keep harping to tell people: this is real.
And if you do get a medication, and maybe if you are, don’t have a lot of money, don’t settle for the first medication your doctor throws at you, especially if it’s not working, you know? And then if it’s not working, say something. Don’t wait like I did, 25 years before, you know, saying, something is wrong here.
I mean and you have to get treated because you don’t want to damage your joints, you know. We can’t wait too long to start a treatment, you know, because we don’t want to get sicker.
DK – It’s hard to hear Diane’s story and about all of the roadblocks she faced. Race and medical care is such an important topic — and, frankly, it could be a podcast all on its own — so I asked rheumatologist Dr. Grace Wright about the challenges of accessing better care and treatment for PsA when you’re a person of color.
GW – When we think about the difficulties that patients face and being diagnosed, it’s compounded by the difficulties patients who have different skin colors often face. So you know, there are so many barriers that we can run into.
It’s difficult when you have a shortage of supply of physicians who look like you, that might connect with you more easily, in some cases, based on you know, the kinds of rash that they themselves may experience, the differences, because we don’t have enough diversity amongst our health care provider groups. So that’s not always easy. And so sometimes you really have to stand up and say, “that’s not what I said, that’s not what I’m feeling.”
So you know, I go back to the courage that’s needed to confront the doctor who’s dismissing you, the courage that’s needed to find that person who’s going to take the time to do the investigations. And, and sometimes it’s clear to a patient that it’s not going to be this person, because I don’t, i don’t have a rapport, I can’t seem to get them to hear me. And it’s okay to then find somebody else.
So it’s really having the courage to insist again. It’s like if you go to the store and you wanted, you know, this bag of flour, and they don’t have it, you ask them, “can you check in the back and see if it’s there?” It’s the same approach. Can you check again? Is there a blood test, or somebody else I can go to? Because I really want to know what this is. Maybe it’s just dry skin. But I really want to know. That’s a way to build courage, so that you’re able to push past the barrier, in which sometimes you’re discounted as a patient sitting in the room. I can, I can talk about this for a long time. We’re actually writing an entire educational series on this. So it’s a very, very important issue.
DK – Hearing Dr. Wright talk about courage immediately made me think about Diane, because she does have that courage. She pushed, she persisted, and when she finally found the right doctor, things started to change for the better.
So then how did you get properly treated? How did you find a doctor? What happened?
DT – It took me 30 years to find a doctor. I’d lost count of the doctors that I had seen over the years, and I wasn’t educated enough to know that I could get clear. So in my mind, I was starting with “this is the best I’ll ever, ever get.” When I was, I think around 38, my body kind of exploded. I was 90% covered in psoriasis and I was in the worst pain in my life, it even hurt for water to touch me. And I knew at that time, it’s like, nobody can live like this.
That’s when my husband and I decided, you know, enough is enough. We’re just gonna find a good doctor, you know, and he took off from work that week. And that’s what we did. We searched for a doctor, and we found one, and I’ve had him for like 15 years now.
DK – What happened when you went to the doctor? What, what did the doctor say?
DT – He was just, he was the best, he sat me down, he actually talked to me first, you know, we need to work on a treatment plan that, really, that works for you. He wasn’t talking at me, he talked to me, you know, we need to do something together.
When treatment is not working, we, he actually sits me down and we, we will discuss a treatment plan, like I said, we’ll try this for three months and if it doesn’t work, then we’re gonna put you on something else. He is not one of these doctors who rushes in, then rushes out. He sits down with me and has a conversation, and I really like that.
DK – Oh that’s fantastic. I mean, having the right doctor is so important. Because it’s like, if you can’t even, you know, get to the point where someone’s listening to your symptoms and has good ideas — and by the way, more than one idea — then you can’t get better. They’re kind of the gateway to whatever treatment you’re going to need, right?
DT – Yes, yes exactly.
DK – So Diane, tell me about what kind of symptoms you have right now. What’s going on with you?
DT – Well right now, you know, I have the psoriasis, of course, it never goes away, but I also have the pain of the psoriatic arthritis. It’s in my elbows, my shoulders, my arms. It’s like the pain starts at my knees and it just, it just works its way up and it’s just, it doesn’t go away. The pain is always there, all the time. That’s, that’s basically it.
DK – I get it. I’m assuming you’ve been talking to your doctor about what’s going on? Are you guys going to keep going with the same one or try something else?
DT – I have been on seven biologics. And I think my body is just running its course, but we, we always just go to another one if it’s not working in six months, we’ll go off of it and start me on a new one to see if it works. And so I’ve been on biologics for 20 years now. So it’s just, it’s just ran its course and I understand that.
DK – Look, I’ve only had PsA for two years and I’m still trying to find the right treatment plan. It can be really frustrating. When I was first diagnosed, I thought I would just take a medication and feel better right away. Now I know it can take more trial and error than that. And, look, as Diane said, if one medication doesn’t work, partner with your doctor and figure out what’s next. For me, that seemed like really good advice. So next our conversation turned to the idea of what feeling better would look like for us.
I know that doctors now are doing this thing, where they’re talking about the idea of minimal disease activity. I think the idea is getting to the least amount of symptoms, kind of across the whole spectrum of symptoms that you have. So for me, you know, what I would consider like, a more minimal disease activity would be, my skin’s actually pretty good. But not two or three flares a month, and fatigue issues and brain fog, those would be things that I would really like to see minimized, personally.
DT – So for me, I guess it would be, like less flares. If I had less flares, I wouldn’t stay in bed as much. Maybe I would go to the store more often, or, you know, even go, even go out with my husband sometimes instead of going, you know, “I’m really drained right now. I don’t want to do anything.” Or when friends call me I can say, you know, I can stop saying, “I’m sorry, I’m tired today,” you know, and then them saying, “well, you weren’t tired yesterday.” The other thing would be, you know, the pain, we have pain every day. So I guess less pain would be one of them, even, you know, it, it hurts to walk sometimes.
So I mean that would be minimum disease activity to be able to be able to walk on longer walks. I have a dog, I can’t even walk my dog because it’s too much and he’s not a big dog, but he’s strong, and I’m scared he’s gonna hurt me.
DK – Because you’ve really been dealing with this for a while. How have you been able to deal with it, in terms of, emotionally? I mean, you have so much experience with this. So I don’t know, it must have changed over time.
DT – It did. It actually, it actually got better for me as I got older, as I got wiser, as I learned about me, my disease. But I also had to learn how to tell my story, and that’s what I did. I learned to tell my story. It wasn’t an overnight thing. It took me a long time to get where I’m at, but my having psoriasis and psoriatic arthritis have truly made me a better person. Truly.
I’ve got to speak in front of the FDA before, you know? I go to Capitol Hill every year and speak in front of Congress, you know. I attend conferences, I go to events, you know. I’m doing this podcast right now. So I get to do all these amazing things in the name of psoriasis and psoriatic arthritis. I have met people, seen people, that most people will never see in their whole life.
Someone told me a bunch of years ago, you have a voice, use it. That had to be the best advice ever. Use your voice. You know, I just never knew how far my voice could go. And sometimes I still to this day, I know like, um, you know, stop mumbling girl, you know?
DK – No, you’re not mumbling!
DT – I just knew a few years ago that I wanted to help people. I didn’t want people to feel like they were by themselves. But that’s how I felt my whole life, that I was alone, that there was nobody like me, no one understood.
DK – I admire Diane’s attitude. She’s not so positive that it feels like a bunch of bull. She definitely is keeping it real. She has symptoms, she doesn’t have it all figured out. But she has this wisdom and perspective that is really reassuring, right? Anyway, like I said at the start of this podcast, I have concerns about having a chronic illness for the rest of my life. So I was eager to get Diane’s take on that.
And what about the stigma? You talk about how you have, you know, skin stuff, when you’re flaring, when your skin is flaring. It’s always flaring, right?
DT – It’s always flaring.
DK – So how do you deal with that? Do you worry about stigma anymore? Are you just like…
DT – Not at this point in my life, I don’t care any more. I’m not, I’m not a teenager anymore, like I’m in my 60s. If you don’t want to look at me, go away. You know, just just leave me alone. I don’t really care anymore. You know, that’s just my take on it.
DK – I think as women, we gain a lot of power back when we decide that we’re not here to be looked at by other people for approval. Yeah, yeah, I don’t, I don’t really need that, actually. I have so much more to offer than what, you know, my leg looks like. And if you don’t get that, then I don’t, I really don’t have time for you.
DT – That is so true.
DK – I worry about, you know, the progression of the disease. I get scared. I try not to think about it too much, you know, because I worry about pain, and you know, if I’m this way now, what am I going to be like in 20 years?
DT – Trust me, I understand what you’re saying. And I used to feel the same way. But like I say, you know, for me, I had to learn to balance my, balance things in my life and I couldn’t really worry about you know, am I going to get worse?
But one of the things that I’ve learned over the years, we have to also take care of ourselves, you know, somebody else is not going to do it for us and we have to do it for ourselves. And one of the things I do, as a psoriatic arthritis patient, as you know, we get tired more often. So we need more sleep, so I’m saying, go get your rest, you know.
And another thing is keep your, keep your stress under, you know, at a minimum. It’s hard, but stress does, it really triggers our disease, you know, so how to manage your stress.
And then, the last thing you know, you know, growing up, as I said before, I kept to myself, wouldn’t talk to people. So I used to keep every, everything in and wouldn’t tell anybody. And if this is you, I would suggest you know, maybe just talking to a therapist, or a good friend, or just, you know, anybody. And my last thing is remember, you are not alone in this journey. There’s always someone you can talk to or help you.
DK – Diane, this has been such an incredible pleasure. Thank you so much for taking the time to talk to me. Really. I learned so much.
DT – No, thank you. This was awesome. Thank you for making me feel comfortable. I’ve learned so much from you, too. Thank you.
So I think Diane helped me feel less alone, and I hope she did that for you too.
Speaking with her was really validating. I struggle with the fact that I have a disease that other people can’t see. Yeah, I have psoriasis, but I can cover that up. I worry that people will think I’m a wimp if I don’t feel well or I’m being too needy or complainy. Hearing about everything Diane’s been through, I think it does give me that permission to take care of myself.
Diane showed me why I shouldn’t settle, even if it’s been a really long time since I’ve felt well. I was struck by her perseverance and how she ultimately developed the confidence to be heard. Her story shows how important it is to have doctors you trust, who listen to you, and who will work with you.
And by the way, hearing her say that it’s going to be okay really meant something to me, because she’s been there, and she’s still fighting.
That’s it guys. Be well, take good care of yourself, and thanks for listening to The Psoriatic Arthritis Club.
This podcast was made possible with support from AbbVie.
For more support and stories from other PsA patients like you, subscribe to The Psoriatic Arthritis Club or visit psoriaticarthritisclub.org. You can also visit CreakyJoints.org for the latest information and news about living better with PsA.
Episode 3
Eddie’s Story: 20 Years of Life Lessons for Coping with PsA


Eddie’s PsA story involves a relatively quick journey to getting diagnosed and on treatment. But he’s had his share of challenges along the way, and that means plenty of wisdom to impart about the many curveballs that PsA can throw your way. “If you don’t say something, then nothing’s going to change,” Eddie says. “[Doctors are] wonderful people. But clairvoyance is not something that is taught in med school.”











Episode 3 - Eddie’s Story: 20 Years of Life Lessons for Coping with PsA
DK – Deanna Kizis interview audio
EA – Eddie Applegate interview audio
GW – Dr. Grace Wright
DK – Hi, I’m Deanna Kizis and I’m the host of The Psoriatic Arthritis Club, a new podcast from CreakyJoints and the Global Healthy Living Foundation about the ups and downs of managing psoriatic arthritis.
If you’ve been listening to our first couple of episodes, then you know I’ve been living with psoriatic arthritis for two years and I’m doing okay. I’m still having pain and flares and honestly it’s been kind of a lot. I’m learning how to cope with brain fog and fatigue, and I work, and I have an 8-year-old daughter.
I’m not a pessimistic person, but I do admit that sometimes it’s hard to stay positive about everything that this disease keeps throwing at me.
The good news is that talking to other patients about PsA is so helpful. As you’ll hear, Eddie Applegate and I have had more fun discussing PsA than you could ever think possible. And on a serious note, we talk about how there are no easy answers, but there is a lot we can learn when we lean on each other. As a patient, I’m finding that I need more tools that I can use when working with my doctor. And it’s so important to build out a self-care toolkit.
Just a reminder, I’m not giving out any medical advice. I’m not a doctor, just a patient. But there will be a rheumatologist on later in the show.
I’m so excited for you to meet Eddie. This is the first time I’ve ever spoken with him, but I feel like I’ve known him forever. I honestly wish I had.
Yeah, well, we have to use these bodies? You know.
EA – I can’t trade this in for a newer model.
DK – To the end. Yeah, I know exactly, well, I don’t get, it’s not a Subaru. I can’t trade it in for a new one. Yeah.
EA – There’s not a lease on this one. I’m not getting a new one every couple of years with a down payment.
DK – You bought it.
Eddie is 45 years old and lives in the suburbs of Atlanta, Georgia. If I’m sort of a PsA rookie, then Eddie is a total pro. He’s had psoriatic arthritis for almost 20 years and he is a wealth of knowledge. I walked away from this interview inspired and ready to start putting his advice into action.
EA – have a diagnosis story that I like to say is, it’s a little different than people’s because it was a successful diagnosis early on. Which is, I have, I have heard horror stories from from many people.
In my early to mid 20s I had started to experience a lot of pain and stiffness, especially in the mornings. I would sit in the tub and soak in the tub for like 30 to 45 minutes just to loosen up, especially my hands, my hands were and still prove to be, a bit of an issue. And then I started a job in a town that was about an hour away from where I live. So I had a, a fairly long commute every morning and getting out of the car, I would feel it in my legs. Getting up I could tell there were issues there, so I asked my mother if she thought that I had arthritis, and she’s like, well, “you may, but you’d have to go and get a referral first before you can see a rheumatologist.” So I decided to, just to, go to an urgent care clinic. I didn’t have a primary care physician at the time.
The doctor looked at me, looked at my symptoms, looked at my face, because I still had some psoriasis on my face at the time. I had been previously diagnosed with psoriasis, and within a minute or two, he said, “Oh, you have psoriatic arthritis.” An urgent care general practitioner. First time.
DK – That’s great. You’re so lucky.
EA – I call myself a unicorn for that. I know now how lucky I was.
DK – You’re not lucky because you got psoriatic arthritis in your 20s. But, like, you are lucky, right?
EA – Getting diagnosed easily and getting to see a rheumatologist within a month. I know that both of those are, you know, almost unheard of, in, in real life.
DK – Yeah, I was fast and mine took years. How did you cope with that diagnosis? Because you’re fairly young to get it, right?
EA – And it was a little surprising. I was like, “wow, I’ve got arthritis.” That’s when I kept hearing, “Oh, you’re too young to have arthritis.” I think every one of us no matter what age we are when we are diagnosed, I think that everyone is probably told at one point in time, you’re too young to have arthritis.
But, it’s, I think I caught it near the beginning because I was okay-ish at the beginning, but then it kind of, not long after, right around the time of diagnosis and things seem to be getting worse and worse all of a sudden, like, I, my joints were a lot more painful. Getting up from a seated position or a crouched position was, would get tougher and tougher. Walking would become and look, even look, more labored, not just become more labored. But, you know, my parents and my sister said “you walk like an 80-year-old,” which, when you’re not yet 30, that’s not, that’s not what you normally want to want to hear.
DK – No.
EA – Plus, that’s when my skin started getting worse as well. And I got it all over my face pretty much, and being a guy, you can’t, you can’t, hide behind makeup. Like, Like a
DK – It doesn’t work for that anyway.
EA – I like hearing that. I don’t feel so…
DK – It’s true. It will just peel right off. It’s kind of like, remember when we were in high school and kids would put that flesh-colored pimple cream on? And you’d be like, Wow, you have a giant beige spot on your face with pimple underneath. It’s like that. You’re just like, what is that anyway?
EA – Okay, good. I don’t I don’t feel like I’ve missed anything, though, so I feel a little better about that.
DK – It’s so distressing. And I had a similar experience. So what happened when you went to your doctor and started saying, okay, here are my symptoms? How did you get good care? Because as you know, sometimes you have to push a little bit. I don’t know if you did.
EA – I got lucky with that first doctor. He was really good. He made sure to ask me a lot of questions and tell me a lot of things. So my doctor started me on, was going to start me on a biologic and I was going to take it in conjunction with an oral medication for my disease. It was called methotrexate. And it was fine. My symptoms didn’t get worse. I don’t feel that they got better. But they didn’t get worse. So at, at best I was able to maintain.
DK – Yeah, that’s the part that I personally find really frustrating is that you get the diagnosis. But that doesn’t necessarily mean that you’re going to improve right away. It can take a really long time.
EA – That was me at the beginning. And I didn’t feel like I was improving. Because usually, whenever you go to the doctor, and you’re sick, and they give you medication, you’re like, “Oh, good, I’m gonna be better in a week.” I take this, I take this antibiotic, and 10 days later, I’m going to be fantastic. It doesn’t work that way. And that’s the mindset that we don’t, we don’t realize that we may not get back to pre-diagnosis days, but whenever you do kind of stay where you are — and this is something that I’ve learned over my almost 20 years — that’s when you have to say something.
It all goes back to that communication. It could be that the medication you’re on is not working and it’s not good for you, and so something else needs to be tried. So it was, it was very disheartening for me at the beginning. I was not officially diagnosed with any sort of depression, but I was not in a good mental state in my late 20s and early 30s because I was in pain all the time, I had gained weight because I was not moving. I felt that pain of just plateauing, and you’re just kind of wondering if things are going to get any better, and I wish I would have known then to speak up more or talk with someone. There are many resources out there. I hate that I didn’t know. I do feel like I lost time.
DK – And so what turned it around for you? Because it sounds like you were really kind of plateaued for a long time.
EA – I got lucky with, with number two, and I was on that medication for 12 years, minus a six-month try on a different one.
DK – Does that mean that the medication that you’re on right now is not working as well?
EA – A little over a year ago, I had started having some pain in my knee and in my ankle that was new. And so I told my doctor about it. And he said, “Well, you know, it could be that your current medication may not be working anymore, and may not be as effective anymore. We can look into changing your medication because he’s all about you know, if it’s not working, let’s, let’s try something else.” So I’ve been very lucky with my doctors, I know that. None of that would have happened if I just said, “Oh, I’m fine.” Because you know what they say, the squeaky, the squeaky wheel gets the grease.
You don’t want to be stuck in something that’s not working because you’re afraid to say something. Because if you don’t say something, then nothing’s going to change. If a change is needed, if you feel a change is needed, and you don’t say anything, the doctor is not going to know.
DK – They’re not psychic.
EA – Exactly. They are, they are, they’re wonderful people. But, you know, clairvoyance is not something that is taught in med school.
DK – So this conversation is really important. I like the idea of really letting your doctor know what’s going on, what’s bothering you. And also trying to figure out that balance of, like, Am I really feeling as good as I can? Am I not? What does feeling well with this disease even look like? We asked rheumatologist Dr. Grace Wright how she thinks about this.
GW – If you feel much better then oftentimes patients will say I’m better enough. Because I was so worse before. But my goal is to have you be well. So treatment inertia is, is really a very difficult thing, because it occurs on both sides, the patient and the physician. I may accept too little for you, you may accept too little for yourself. How do we shift that? And part of that, I find, is transforming how we rethink possible.
So I always sort of say to myself, you know, I have a big kitchen analogy of things that I put in the kitchen cupboard and push to the back. And I kind of forget about it and say, well, it’s there, it’s going to last for forever. And we sometimes do that with patients, and patients sometimes do that with their symptoms, where they just accept that it’s going to be there and it’s going to be there all the time. So I go through this exercise of pulling things out of the back of the cupboard, of taking a patient, sort of stepping back and going, are they really as good as they can get? What are the things that we have now that we didn’t have three years ago, or two years ago or 10 years ago, when they got to this date, and it really forces me to rethink, and then have the conversation with a patient to say, you know, you don’t really have to have five swollen joints all the time. Perhaps maybe you can think about being able to walk around the block rather than having to walk and stop every 10 steps. But part of it really is me re-envisioning your possibilities because it’s not often easy for the patient to know that there are other options, that there are additional things that can be done to change their lived experience.
DK – A lot of what Dr. Wright shared reminds me of this conversation we’ve been having on this podcast about minimal disease activity. I’m still learning about it, but my understanding is that it can be a way for doctors to assess how our PsA is doing by looking at a range of our symptoms, a way to make sure that things are getting better across the board. I wanted to get Eddie’s take on this, because it sounded like he was doing well with his PsA for a long stretch of time.
So we were talking about this concept of minimal disease activity and I’m wondering would you think that you are there right now? And if not, what would that look like, to be there?
EA – I think when I first started medication number two, I believe I was in minimal disease activity there for a number of years. I know I’m not in full disease activity. I don’t feel like I did pre-pre all of that. But I don’t feel as good as I did right after I started that. So I am, so if minimal is full, then I’m probably at about three-quarters of a tank.
DK – So you have 25 percent to go.
EA – Yes, I have, I’ve noticed more recently, within the past year, year and a half I’ve noticed that pain comes more, stays a little longer, and then when you feel the, the aches and the pains and you see the swelling and the knots kind of creep back in more you get, it is a little discouraging, but you just kind of realize that I’m still able to function, I’m still able to, to do a lot.
But you just, you notice it more. And I think that’s when you know you’re not in minimal disease activity, when you, when you notice it. You know, when you’re, when you’re not thinking about it as much, you’re not noticing as much, then you kind of realize it, yeah.
DK – Minimal disease activity for me is when I can remember my own friends’ names.
EA – When I can get out of the car without grunting.
DK – When I can eat a lollipop without shattering my own jaw.
EA – When I can take the top off of the two-liter bottle by myself without any help and without feeling it right after.
DK – Yeah if I don’t have to hand my daughter the string cheese to open for me then I’m in minimal disease activity.
EA – Exactly.
DK – You’ve been dealing with this for a long time, and you advocate for really good health care, what would you say to someone who’s been living with this, or maybe you know, is new to this.
EA – Definitely talk to your doctor. Let your doctor, or medical professional, because it could also be a physician’s assistant, or a nurse practitioner. Let your medical professional know how you’re feeling. Don’t try to sugarcoat it. You don’t get extra credit for being a martyr on this. “Oh, yeah, I’m fine.” No. If your pain is an 8, say your pain is an 8. You’re not going to get extra credit for coming in saying, “oh, I’m just at the 3 today and I’m still able to,” tell them, you know, be honest.
DK – I had to learn that the hard way, to be honest. Yeah. I actually said out loud. Someone close to me is like, you know, you really need to call your doctor. And I heard myself say, “I don’t want to bother them.”
EA – I’m glad that it’s not just a southern culture mindset. It’s everywhere. Because we’re all like, “Oh, I don’t want to bother the doctor.” I don’t want them to think that I am, they’re gonna think that I’m just a complainer.
DK – I worry about that all the time. All the time. I also worry that people think I’m making it up. That’s like a big one because people can’t see how bad I feel, I really worry that people think I’m just histrionic or attention-seeking, or–
EA – As I said, you, people, you may think “oh, they’re, she’s just doing that for attention or he’s just, he just wants people to feel sorry for him.” No I don’t. We know our bodies better than anyone. So why shouldn’t we be our best advocate for this vessel that we know better than anyone else?
Knowing your body and learning not to be afraid to speak up to the doctor. It’s taken me a long time, it’s taken me almost 20 years to be able to say, like, “Nope!” At my last telehealth visit, I said my hand is hurting, you can’t really tell, but they’re swollen, right here, my feet as well. And she said, “Okay, well, let’s get a new baseline. Let’s get some X-rays. Let’s see how that goes.” So if I didn’t speak up, that was not going to happen.
Keep up with your symptoms, even if it’s, you know, writing down on a piece of paper or a notepad or on your phone beforehand: “This is how I’ve been feeling.” Keep track of everything. There are wonderful apps that will help you.
DK – I do not know about the wonderful apps.
EA – ArthritisPower is a wonderful app. I know. It is great to put in your symptoms. And it’s great to look back and see how things can change over time. And on a certain day, like, “Oh, I felt bad here.” And it’s great if you switch medications and then see, okay, let’s see if this medication is working.
But if you’re a writer, write it down. Just have some way to, so you don’t forget because a lot of times we get amnesia whenever we go to the doctor’s office because we forget everything that’s been happening. You’re, you’re on your drive over there. Alright. My feet have been hurting for the past two weeks. I’ve been extra tired. I felt this.
And then you get to the office, “So how are you feeling today?” “I’m fine.”
DK – Uh huh. Oh, I’ve totally forgotten. I look, I mean, I have brain fog anyway. So it’s amazing I’m even here right now.
EA – And then we get in there afraid to tell the doctor how we really feel, so if worse comes to worst, write it down and go “here.”
Go, “here you go. Here’s the paper. This is how I feel.”
DK – Uh, I love. You know everything. I’m so happy.
I told you that Eddie has a wealth of knowledge and he’s got a lot of support to give, right? So before we wrapped up, I got a little bit more of his wisdom.
EA – Learn what you can and can’t do. If there’s the things you can’t do, are the things to make it where you can do them? Are there little life hacks? Are there tips, are there tricks? Are there aids that will help you to do that? Don’t be completely frightened. Is it, is it scary? It’s absolutely a little bit scary. Let’s, let’s be honest, it is scary at times. But it’s, you know, your life isn’t over.
And I think that’s where learning your limits from what you can and can’t do. Because learning what you can do. “Oh, I can do this, I can do that, I can, I can still do that.” Focus on the can. I think too often, and I know that I’m guilty of it as well, “I can’t go and this. I can’t do that.” You know, it’s gonna, it hurts too much for me to do this. So what can I do instead?
DK – One of the things that I also like about that is that there are some things that I found that I can do, that have become new, very passionate interests of mine. You know, I don’t think that Zumba is in the cards anymore. But my vegetables are amazing. So yeah, and I didn’t know that I would actually enjoy gardening as much as I do and get as much out of it and also how it actually helped keep me in shape. So there have been things that I’ve focused on.
EA – It is self care. Because a lot of times people forget how important self care is. This disease is more than just a physical disease. It can take its toll on you, mentally and emotionally as well. And so you do have to make time to recover. Just, take a holistic approach to yourself, you know, mind, body, soul, and just, you know sometimes soaking in the tub. That’s one of that’s one of my, my self-care, is like, I need to soak in the tub, is one.
So whenever I watch House Hunters and they go, “I don’t need a tub, I just need a shower. I’m like, “No, you leave that tub right where it is.”
DK – It just occurred to me, I do have this friend who, when I’m really upset about something, she does tell me to make a list. And on one side of the list are the things that I can’t control, right? And on the other side of the list are the things that I can. And then she says, “Okay, now turn your attention to all of the things on the right side of the list.” And that really is so helpful to me.
EA – Yeah, because we too often focus on that negative. My mind can be a very, just a dark cave of negativity. And it’s just, you have to, you have to fight that. You’ve got to realize that there is some happiness, and you know, what, what I can do? And am I hurting today? Yes. Can I still sit and do my New York Times crossword puzzle app on my phone? Absolutely. Sit in the tub and soak for a little bit and just relax for a little bit. Can I do that? Yes. And so it’s just those little things.
Those are some things I would suggest to people. There’s no, there’s no perfect roadmap that fits everybody. There’s no one plan that fits everybody. But we’ve all been there in some way, shape, form, or fashion. And we all are just trying to get through this together the best that we can. We don’t have all the answers. We’re not going to have all the answers because there’s so many things that we don’t know. But listen, learn. Ask questions.
DK – Thank you so much. This has been so much fun. I love talking to you.
EA – I love talking to you as well.
DK – Thank you so much for talking to us. Seriously. It’s been great.
EA – Thank you for having me.
DK – I hope you walk away from this conversation feeling as supported and validated as I do. I don’t have close friends with chronic illnesses like psoriatic arthritis. Eddie — and Diane and Lauren, who were in the first two podcast episodes — were the first people with PsA I’ve ever talked to about what it takes to live with this disease.
What I got from them is that you have to keep talking to your doctor about how you’re feeling, and to be really clear about where you’re struggling.
I also learned that it’s okay that I’m going through various treatments and I can know that just because I’m not feeling great yet doesn’t mean I won’t feel better at some point. And I loved hearing about the life hacks that can help me cope.
And most importantly, it felt so good to find out that even though we have a chronic disease like PsA, there is a community that can help. That includes the right health care provider, resources like CreakyJoints, talking to others who have this disease and putting yourself out there to make new friends, which is what I did while hosting this podcast.
That’s it for The Psoriatic Arthritis Club. Thanks so much for listening.
This podcast was made possible with support from AbbVie.
For more support and stories from other PsA patients like you, subscribe to The Psoriatic Arthritis Club or visit psoriaticarthritisclub.org. You can also visit CreakyJoints.org for the latest information and news about living better with PsA.
PSORIATIC ARTHRITIS PATIENT AUDIO GUIDES
Want to learn more about managing PsA?
Our Patient Audio Guides offers information and insights from leading psoriatic arthritis experts so you can be more informed — and take better care of yourself or a loved one. Check them out below and wherever you listen to podcasts.
Be sure to subscribe for access to future episodes.
Audio Guide:
Collaborating with Your Rheumatologist
Whether you’re newly diagnosed, suspect you have PsA, or are experiencing worsening symptoms, this guide will help you prepare for more effective doctor visits to discuss treatment and improve your quality of life.











Audio Guide: Collaborating with Your Rheumatologist
Narrator 00:00
Be inspired, supported, and empowered. This is the Global Healthy Living Foundation Podcast Network.
Angela Degrassi 00:08
Did you know that psoriatic arthritis affects more than 1 million people in the United States alone? Welcome to the Patient Audio Guide produced by the nonprofit, CreakyJoints and the Global Healthy Living Foundation and made possible with support from AbbVie. Our mission today to empower you to work with your doctor for a better quality of life with psoriatic arthritis. Maybe you or someone you love suspects you could have psoriatic arthritis or PsA for short. Or perhaps you have been recently diagnosed with psoriatic arthritis or maybe you’ve had psoriatic arthritis for a while, but you’re experiencing new symptoms or are concerned that it’s getting worse. This audio guide can help you better plan for your next doctor’s visit so that you can have a more informed conversation about treatment options, disease activity, and more. I recommend taking a moment to grab a pen and paper or open a note on your device because we’ll be sharing valuable insights to help you plan for your next doctor’s visit. Start planning for a better quality of life today. Remember, this is not a substitute for professional medical care. Always talk to your doctor about issues concerning your health or medical condition. Today we’ll discuss how to work with your rheumatologist to have a more informed conversation about treatment options and disease activity. Joining us today is Shilpa Venkatachalam. PhD, MPH and Director of Patient Centered Research, Operations and Ethical Oversight and Co-President of GHLF Canada. Shilpa is one of my colleagues here at GHLF. And also happens to be a patient herself. Hi Shilpa.
Dr. Shilpa Venkatachalam 01:56
Hi Angela, thank you so much for having me today and for this really important conversation.
Angela Degrassi 02:02
Shilpa, I really value working with you and you always bring such great insights to these conversations because you’re a researcher but you’re also living with a condition yourself. So you really get to see so many different aspects of what it’s like to treat and live with a chronic condition. We really appreciate you sharing your experience with us today.
Dr. Shilpa Venkatachalam 02:26
Absolutely, Angela. I want to start actually by sharing some information about myself for context. My name is Shilpa Venkatachalam. And I work in patient centered research in chronic diseases and a dramatic and musculoskeletal conditions like psoriatic arthritis. In fact, I myself was diagnosed with seronegative RA or rheumatoid arthritis in 2017. Then, about five years later, surprisingly, it was suspected that I actually have psoriatic arthritis, not rheumatoid arthritis course this came to me as a shock. And then shortly after that, my diagnosis was again changed to seropositive rheumatoid arthritis with what I was told were some features of psoriatic arthritis. So as you can imagine, it’s been quite a journey. So far, I’ve tried and been on at least 10 different medications or DMARDs and I’m on my 11th, which is a JAK inhibitor. I’ve been on pills, on single therapy, double therapy, combination therapy, injectables, and some have worked well for a very long time and some really haven’t. In fact, some seemed like they would be working initially, but they didn’t really after the first three or four weeks. Unfortunately, this is a very familiar story for many of us living with these conditions. So I guess today I speak from the perspective of a researcher, as well as a patient and like any other patient, I have my own fears and apprehensions about medications, about side effects, my own battles with pre-authorization and frustrations. And then of course, there’s elation and happiness and hope when I try a new medication and wait for it to work and sometimes it does.
Angela Degrassi 04:12
Thanks Shilpa. So let’s dive in and talk about some practical steps you can take to work effectively with your rheumatologist and manage psoriatic arthritis more proactively. Okay Shilpa, we structured this audio guide to inspire collaboration between patients and their rheumatologist. Here are eight things you can do to be more prepared for your next appointment. Let’s start with step number one, define your treatment goals and lifestyle considerations. It’s really important to identify what you want to achieve with your treatment. Some common medical goals include reducing pain and stiffness or improving joint function. Lifestyle goals may involve maintaining fitness or balancing work and personal life.
Dr. Shilpa Venkatachalam 04:50
So goal setting is a really important part of disease management and goals really come in all flavors. Most importantly, goal setting helps you introspect and think about what things really matter to you, right? What can make you live well and be happy while living with this disease? So for example, your doctor may have goals that have to do with your bloodwork, your doctor might want to make sure your CRP levels are in control, or that you’re not anemic, or that your fracture is healing nicely. But personal goals can be things that relate to your everyday life, I want to get to a place where I can sleep through the night without waking up in pain. I want to be able to go out with my friends and not have people look at my skin lesions. I’ll give you a personal example. Recently, I needed to travel internationally. And then of course, I fractured my foot. My goal was to find a way to travel despite my fractured foot, but also to make sure I was resting my foot, giving it the necessary time to heal, and so I ended up using crutches and a wheelchair. Another goal of mine was to reduce stiffness, joint stiffness. So I spoke to my doctor, and she reevaluated why I was having so much stiffness in the first place. Was my current biologic not working? Did I need to switch medications? Was I not exercising and doing my physical therapy? These are some of the questions we thought about together, and then we worked on a plan so that in three months, my stiffness would get better.
Angela Degrassi 06:30
Defining your goals is so important and being able to communicate that to your rheumatologist is key. Just as important is sharing your priorities and preferences for treatment options. It’s essential to clearly communicate what you want to achieve with your treatment. Are you looking to reduce pain and stiffness? Or do you want to improve joint function? Also, take a moment to think about your lifestyle and what type of medication would work best for you? Maybe there’s more than one way to administer the medication? For example, are you more comfortable with taking a pill? Or would an injection be more suitable? By sharing this information, you and your doctor can work together to find the treatment plan that fits your needs and lifestyle the best. It’s all about finding what works for you.
Dr. Shilpa Venkatachalam 07:20
And I’ll be honest, I’m a researcher. In fact, my research is in this area. And still I have fears like anyone else. When it comes to medications. There was one particular medication, for example that I was taking that was making me very nauseous. So I spoke to my doctor, and she suggested I try a few different things and stay on the medication. But I was not wanting to do that. I just did not want to take that medication. So I sat down with her and I asked her to provide me with other alternatives. And I promised her that I would adhere to the next treatment she would put me on, together, we made a plan and I was able to move to another medication. It is really important to advocate for yourself. Your doctor wants what is best for you. And in the end, even the best medication will not work if you don’t stick to it. Learn about your preferences, because it will also help you learn about yourself.
Angela Degrassi 08:17
Thanks Shilpa. That’s insightful, it’s so important for patients to share their priorities with their provider. And that’s something that a patient featured in this season of The PsA Club did very well. If you haven’t listened to Jonathan’s episode, go check it out and Shilpa that brings us to our next point discussing treatment options. When it comes to treating psoriatic arthritis there’s a wide range of options available, including NSAIDs, topical therapies, ultraviolet light, and systemic therapies. During your discussion with your doctor, it’s crucial to explore the benefits and risks of each treatment option. Don’t hesitate to ask any questions you may have to ensure you fully understand the potential outcomes and possible side effects.
Dr. Shilpa Venkatachalam 09:04
So one of the most frustrating things about living with a disease like psoriatic arthritis is that you just don’t know which medicine is going to work for you. You have to try your medication and then wait and watch. Sometimes it works. Sometimes it doesn’t. It is so frustrating. Meanwhile, the pain and the fatigue is always there interrupting everything you do. I use multiple things when I’m in a flare or when I’m waiting to see if medication can actually work for me. I asked my doctor about what she thinks too. Sometimes I feel like I’m asking too many questions. And then I remind myself, this is my health after all. I’ve asked my doctor and I’ve asked other patients what kinds of braces and splints work for them. If my pain is really bad, I asked my doctor to give me something like an NSAID that can give me immediate relief. If the onset causes an upset stomach. I asked my doctor where else I can turn to all this time I’m hoping and waiting for my medication to kick in. And I know that it may not because it may not be the right medication for me after all, I hate that process of waiting and watching and then going through it all over again if needed, but that’s happened to me. I was diagnosed in 2017. It’s 2024. So far, I’ve cycled through 11 medications, I know there are options, but I also know that I cannot lose hope, or maybe I can momentarily but then I need to do everything I can and use every support I have to get back on track.
Angela Degrassi 10:39
Thanks Shilpa. Something else that’s really important is monitoring your progress. Let’s talk about that for a moment. regular monitoring is vital. This could involve various disease activity measures like the disease activity score DAS, which combines the number of swollen and tender joints, global health assessment and a blood test marker like C reactive protein or CRP to determine disease activity, the psoriasis area and severity index PASI which is used to assess the severity of psoriasis skin symptoms often associated with PsA or the composite psoriatic disease activity index CPDAI, which evaluates skin and joint involvement and patient reported outcomes to measure overall disease activity in PsA.
Dr. Shilpa Venkatachalam 11:32
So there are really important in understanding how you’re doing with your disease. These are disease measurements that are important from a research standpoint, as well as from a care standpoint, it’s really a great advance in science that we have ways of measuring things, how well a medication is working, how controlled a disease is, how active my inflammation is, imagine if we did not have a way of measuring this we’d be completely lost. It’s like walking in a dark room and trying to find a switch, you may hit a wall, you may break a lamp, you may enjoy yourself, you don’t want to make decisions in the dark, you want to be guided to make the best decisions possible. And that is what measures like the DAS or the CDAI or bloodwork and biomarkers and labs do their roadmap, a helping hand, a switch to turn on the light so that you know what needs more attention and improvement, how your treatment needs to be adjusted. For example, think of it like the volume control, you need to find the right volume to enjoy your music too loud, and it will hurt your years and sound like noise, too low and you won’t be able to hear anything. measures allow us to understand what to turn up and what to turn down. They help us to figure out if the medication I’m on currently is actually working, and if it isn’t, they help us have a conversation with our doctors. So that together, we can figure out the way forward.
Angela Degrassi 13:02
I can see how these measures really help you to understand your condition and really figure out what’s next. And having these measures might also be helpful when it’s time to adjust your treatment. So let’s talk about that, adjusting treatments as needed. Don’t hesitate to talk to your doctor about adjusting your plan if you find it’s not meeting your goals or causing side effects.
Dr. Shilpa Venkatachalam 13:27
So that is a really important point, Angela. It really is very important to keep speaking to your doctor, reevaluating your goals, and adjusting your goals if required. There are so many examples I can give for myself. Recently, I had a lot of foot pain, it got worse over time. Now first I thought this is a flare. And so I took a course of glucocorticoids with my doctor’s advice, of course, and a few weeks later, I had relief for a few days, but then the pain came right back. Next I was sent to do some imaging. Imaging revealed that I had a lot of synovial fluid and bone erosion and a fracture that happened without any event, at least as far as I can remember, this made me nervous. I didn’t want to switch medications all over again. I told my doctor that I wasn’t ready to switch. My doctor looked at me and asked if I would rather continue limping and taking painkillers, eventually even risk having more bone erosion. She even told me I might be unable to stand without pain if I continued like this. She spoke to me about how I was doing myself a disservice that things would only get worse. Eventually, she and I determined that I did need a new medication and I eventually started one. So talk to your doctor, if you are scared about changing medications and be clear about what your fears are. I was afraid of the side effects of going through a medication that might not work all over again. So speak to your doctor about every fear that you have and develop a timeline to help you assess if you are getting better, especially when you start a new medication.
Angela Degrassi 15:11
Shilpa you mentioned, you had to adjust treatments 10 times, unfortunately, it can take some time to find the right treatment. And that’s okay. I’d like to talk about how mindset is an important part of the patient journey. Having patients with your journey is essential. And your doctor is your partner in this process guiding you to what works best for you.
Dr. Shilpa Venkatachalam 15:34
Absolutely right. But it’s easier said than done, isn’t it? Sometimes finding the right treatment can even take years when I start a new medication, which unfortunately, like many others, I’ve done a few times now. I mean, forget the physical side effects. There are so many mental health concerns, anxiety about if the new medication is going to work, fears about what the long term side effects might be, I always worry about my liver and my kidney, for example, thinking about, well, what if this medication doesn’t work. And of course, having to go through all this all over again, these are just some of the fears. This is just the tip of the iceberg. But through it all, you have to find a way to be patient with yourself and with your body. There’s going to be a lot of bumps along the way. But you know, chronic illness can also teach you a lot. It teaches you patience, it teaches you to face challenges, because you may sometimes have no choice. In fact, it may help to even get a therapist or psychologist to help you navigate the many different emotions that can swell up while dealing with a chronic illness like this one.
Angela Degrassi 16:47
Shilpa, you have to be so strong to go through that experience over and over. And that’s something I really admire about you. Your patience reminds me of our first episode of this season with Ashley who very gracefully shares her experience with how she has had to navigate her own journey with a lot of patients. We’re getting towards the end of our audio guide and have just two more points to make. Let’s talk about complementary treatment. I know that is something you’ve explored quite a bit. If you’re using additional ways to manage your symptoms, be open with your doctor to make informed decisions together.
Dr. Shilpa Venkatachalam 17:25
That’s because medications alone is never enough. Don’t get me wrong, they’re absolutely important. But if you don’t combine them with other lifestyle related modifications, then you’re not giving yourself a fair chance. We know through research that a multi pronged approach is very important. And what I mean by multi pronged approach is using medications along with other strategies like exercise, healthy diet, sleep, hygiene, and so on. Me personally, I meditate because it helps me stay a little calmer, especially when I’m about to go for a blood test or start a new medication. I need to be more disciplined about physical therapy, I’ll admit, because I know the research shows that physical therapy helps a great deal to build strength and support your joints. I even try to cook my own food as much as I can. And I’ve adjusted my diet according to what suits me. That means sometimes sacrificing the things that you love to eat, observe your body, it really gives you clues. And if you listen to those clues, you will experience the benefits.
Angela Degrassi 18:36
Absolutely. Those are all great options to explore. Last but not least, our final point is don’t settle for subpar treatment. If you feel your treatment plan isn’t working. Speak up, seek a second opinion if you think your doctor isn’t fully understanding your concerns.
Dr. Shilpa Venkatachalam 18:54
Absolutely. I couldn’t agree more. In fact, in the first years when I was diagnosed, and I started on a medication, weeks and months passed, and I just wasn’t feeling any better. My pain continued, my stiffness continued. And I kept going back to the doctor and telling him that I had more pain and more stiffness. And my doctor kept telling me to give it more time to be patient to take NSAIDs. Every time I showed a bony prominence, the doctor would tell me it was the nature of the disease. And so after a while I stopped and I decided to seek a second opinion. The first appointment of my second opinion was an entirely different experience. It lasted an entire hour and a half. I was examined physically, every joint was examined and looked at. The doctor asked me about my values, my preferences, what my goals were, and together we drew up a plan. I really didn’t know what I was missing until I sought a second opinion. So don’t be afraid to seek one.
Angela Degrassi 20:01
Your journey toward managing chronic illness may have ups and downs. But by working closely with your health care provider and following these steps, you can find the treatment that helps you lead a better life. Remember, it’s a partnership and your doctor is there to support you every step of the way. Thank you Shilpa for your insights and for openly sharing about your own journey as a patient.
Dr. Shilpa Venkatachalam 20:25
Absolutely Angela, thank you so much for having me. I will say that being a researcher doesn’t make the journey any easier. I do know the background. I do know what the research says. But I still have my own apprehensions, my own fears, my own anxieties just like any other patient.
Angela Degrassi 20:44
To our listeners, thank you for joining us on this enlightening journey into managing psoriatic arthritis. We hope that our conversation with Dr. Venkatachalam has empowered you with the tools and insights you need to have more informed conversations with your healthcare provider. Remember, your journey with PsA is unique and we encourage you to take what resonates with you and tailor it to your own experiences. Reach out to your medical team. Engage with support communities, and don’t be afraid to advocate for yourself. To learn more about what it’s like to live with psoriatic arthritis and to hear from fellow patients like you, check out The Psoriatic Arthritis Club podcast available wherever you listen to podcasts or PsoriaticArthritisClub.org. If you found this audio guide helpful, please consider sharing it with friends and family who may benefit from it. Your support helps us reach more people who need this vital information. This audio guide is produced by the nonprofit CreakyJoints and the Global Healthy Living Foundation and made possible with support from AbbVie.
Narrator 21:57
Be inspired, supported, and empowered. This is the Global Healthy Living Foundation Podcast Network.
Audio Guide:
Understanding Psoriatic Arthritis Symptoms
Learn more about the range of symptoms you can experience with PsA, the importance of talking to your doctor about all of your symptoms to improve your care, and how doctors and patients use a measure like minimal disease activity to ensure your PsA symptoms are getting better.











Audio Guide: Understanding Psoriatic Arthritis Symptoms
ER – Dr. Eric Ruderman
GW – Dr. Grace Wright
AO – Dr. Alexis Ogdie
Welcome to this Patient Audio Guide about psoriatic arthritis symptoms. This audio guide is produced by the nonprofit CreakyJoints and the Global Healthy Living Foundation and is made possible with support from AbbVie.
Maybe you or someone you love suspects you could have psoriatic arthritis (or PsA for short), or perhaps you have been recently diagnosed with psoriatic arthritis. Or maybe you’ve had psoriatic arthritis for a while, but you’re experiencing new symptoms or are concerned that it’s getting worse.
This audio guide can help you learn more about psoriatic arthritis and how it affects your health, so you can manage it better and, more importantly, start feeling better.
Remember, this is not a substitute for professional medical care. Always talk to your doctor about issues concerning your health and medical condition.
To learn more about what it’s like to live with psoriatic arthritis and to hear from fellow patients like you, check out The Psoriatic Arthritis Club podcast, available wherever you listen to podcasts or at psoriaticarthritisclub.org.
Let’s start by making sure we explain exactly what psoriatic arthritis is. PsA is a chronic inflammatory disease that can affect both your skin and your joints.
Psoriatic arthritis is different from other forms of arthritis, like osteoarthritis, which happens because of wear and tear to a joint over time.
When we say that PsA is “inflammatory,” it means that there is an abnormal response of your immune system. Your immune system is normally responsible for identifying germs and other foreign substances, but in PsA, the immune system starts attacking your own healthy tissues and cells, specifically the joints and the skin.
This is important to understand for two reasons.
One, because in order to treat PsA, doctors need to use medications that target and reduce that inflammatory response. Two, inflammation can cause irreversible damage to your joints if it is not treated, which can impact your mobility and physical function. This is why finding the right PsA treatment plan is so important.
When we talk about psoriatic arthritis symptoms, one of the first things to understand is the relationship between psoriasis and psoriatic arthritis. Psoriasis is an inflammatory skin disease that can cause a rash, or thick, red skin, or flaky, silver-white scaly patches. Skin can also itch and be painful.
Psoriatic arthritis is an inflammatory disease that can affect both your skin and your joints.
Here is more about the connection between psoriasis and PsA from Dr. Alexis Ogdie, a rheumatologist at the University of Pennsylvania.
AO – Most patients who develop psoriatic arthritis have had psoriasis for some period of time. Let’s say somewhere on average, between five and 10 years they’ve had the psoriasis, and then they develop the joint pain and swelling. But there are a fair number of people that actually develop them within the same year, and then there’s fewer patients that develop the inflammatory arthritis first, and then they later develop the psoriasis. But at any one point in time, the psoriasis may be bad, and the joints mild, or vice versa. The joints may be bad, and the skin mild, so they’re not really connected on a day-to-day basis, let’s say.
So most people with psoriatic arthritis have psoriasis first, then develop arthritis symptoms like joint pain and swelling.
But PsA is much more than just skin issues and joint issues. It’s important to be aware of all the different symptoms of psoriatic arthritis, because they can affect each patient so differently.
Here’s an overview of how patients tend to come in with PsA, from Dr. Eric Ruderman, a rheumatologist at Northwestern University.
ER – People present with a lot of different things, so they can talk to you about, they tell me their pain in their joints, they have stiffness in their joints, they have swelling in their joints, and it can be a lot of different joints, sometimes it’s many, sometimes it’s just a few joints. They may have pain at places where tendons attach to bone, or we call it enthesitis. That’s usually around a joint, but other places as well, that might be things like tennis elbow pain, or a bursitis, or plantar fasciitis or Achilles tendonitis, those are the kinds of things that people may complain about. Their skin may be active, and even nails are an important thing. So people with psoriatic arthritis have a much higher incidence of having nail changes, the kind of nail, fingernail and toenail changes that you see in psoriasis.
Let’s just spend a minute going over the many different symptoms of psoriatic arthritis. First, there’s joint issues: tender, painful, swollen, and stiff joints. Commonly affected areas include the fingers, toes, ankles, and knees. The pain tends to be worse in the morning or after long periods of rest or inactivity.
The lower back is another area that can be affected by psoriatic arthritis, due to inflammation of the spine and sacroiliac joints, where your spine meets your pelvis.
Then there is psoriasis, or psoriatic plaques, on the skin. There are many different ways psoriasis can present, but it often shows up as thick red skin with silvery-white patches. However, keep in mind that psoriasis can look different in different skin tones. It may look more purplish or grayish on darker skin.
Sometimes there is foot, ankle, heel, or elbow pain in PsA that is due to something called enthesitis, which is inflammation of the tendons and ligaments that attach to your bones. You may think you have tennis elbow or Achilles tendinitis when, in fact, it could be a form of psoriatic arthritis.
PsA can affect your fingers and toes in other ways, by causing swelling of the entire digit. This is called dactylitis. It’s sometimes referred to as “sausage fingers” or “sausage toes.” If you have this, taking rings on and off can be challenging. Wearing certain shoes could be uncomfortable.
Your nails may experience changes, such as pitting, where they look like the surface of a golf ball, or look thickened or start to separate from the nail bed.
Psoriatic arthritis can also cause fatigue and make you feel tired and run down, which can be very debilitating.
If all of this sounds like a lot to handle, well, it is. Here’s Dr. Ogdie’s take on this.
AO – That is a lot for patients to deal with. And not everybody has all the features. And in fact, this is what we call this a very heterogeneous disease, meaning there’s just so many different forms of it. So you can have any one of those different things.
The fact that PsA can take so many forms is really important when it comes to figuring out the right treatment plan. We’ll get into this more in future audio guides, but consider this perspective from Dr. Ruderman.
ER – When you think about all the different aspects of disease, and you sort of think about people as a whole person, and everything that goes into it, it becomes really helpful as you start to talk through the treatment options. As we think about what kinds of therapies, what kinds of treatments we might offer. So for example, you know, somebody who has bad psoriasis, bad skin disease, light treatments, phototherapy might be very helpful for them. That’s not going to do anything for their joint symptoms. And so if they have skin disease, and no joint disease, that might be great. But if they have a lot of arthritis, then maybe we need to think about something else that’s going to address both aspects of their disease. And so instead of being on one thing for your skin, and another thing for your joints, and something else for your nails, you could maybe find a single therapy that might address all of that.
Being aware of and being able to explain all the ways your psoriatic arthritis symptoms are affecting you is key to partnering with your doctor on your care. Here’s why.
ER – I need to know what’s going on. I have people who have, you know, who have a lot of trouble with their joints, but not trouble with their skin, or vice versa. And unless I know that, unless we talk about that, we can’t really make appropriate decisions on how to manage their disease because I need to know what’s bothering them, what gets in the way.
Don’t be afraid to get specific about all the ways, big and small, that your PsA may be affecting you. Here’s rheumatologist Dr. Grace Wright explaining what she wants her patients to tell her.
GW – I want them to tell me what matters. So if your skin is driving you nuts, let’s talk about that. If the swollen pudgy digit is driving you nuts, let’s talk about that. And I have patients who have dactylitis, they go, “huh, I have a bigger ring. It’s not a big deal.” But for others, that’s not the case. So I need to know what matters to you. I need to know if you’re sleeping, if you’re in pain, if you’re depressed, if the skin that’s not obvious to everybody is really what’s affected. I’ve had patients, when they take off their clothing, their entire back is covered in psoriasis. They’re the only ones who are aware and nobody sees it on the outside, but they suffer because it’s their back, right? So we need to see those hidden areas and when they talk about what can we do to target those areas that matter to them.
The fact that PsA is so heterogeneous means that doctors and patients need to look at a variety of factors to understand how the disease is doing and whether it’s getting better on a given treatment plan. There is a measure that we are hearing more about, which is known as minimal disease activity, which is becoming more widely recognized.
If you have PsA, you should start to learn about it.
Minimal disease activity is a way that doctors can evaluate how your psoriatic arthritis is doing based on a number of different factors. It’s not just assessing one or two symptoms, like just skin symptoms or just joint pain. Minimal disease activity takes into account many different aspects of psoriatic arthritis in order to make sure that the condition is getting better across many aspects of the disease.
To assess minimal disease activity, your doctor will ask about or check for tender and swollen joints, whether you have any enthesitis (inflammation of tendons and ligaments), how much of your skin is affected by psoriasis, patient reports of pain, daily function, and how you’re feeling overall. You have to score low in most of these areas in order to be considered to have minimal disease activity.
Here’s Dr. Wright’s take.
GW – When we treat a patient, we treat them holistically, so that we don’t just treat the joints or just treat the skin, we want to treat across all the different areas in which psoriatic arthritis affects them. So that I’m getting all of you under control, not just one part of you under really good control and ignoring the other components. So this really is saying this is a more holistic approach to taking care of a patient.
We hope this audio guide has provided helpful information about the range of symptoms you can experience with psoriatic arthritis, the importance of talking to your doctor about all of your symptoms in order to help improve your care, and how doctors and patients can use an evaluation measure like minimal disease activity to assess if your PsA symptoms are getting better across the board.
Psoriatic arthritis can be a complex condition to navigate, but remember that there are many effective ways to treat PsA, especially when you partner with your health care providers. You have what it takes to deal with this.
We’d like to thank Dr. Ogdie, Dr. Ruderman, and Dr. Wright for their input and expertise. Keep listening to our audio guides for more about managing psoriatic arthritis.
For more about what it’s like to live with psoriatic arthritis, check out The Psoriatic Arthritis Club podcast, available wherever you listen to podcasts or at psoriaticarthritisclub.org.
This audio guide was made possible with support from AbbVie.
And for more information about managing PsA and to join a free, worldwide support and advocacy community of PsA patients and their families, visit CreakyJoints.org, which is a part of the nonprofit Global Healthy Living Foundation.
Audio Guide:
Understanding Psoriatic Arthritis Treatment
Learn more about PsA treatment options, the importance of treating inflammation to reduce the risk of joint damage and other complications, and why your doctor needs to know about all your PsA symptoms to pick the right treatment approach for you.











Audio Guide: Understanding Psoriatic Arthritis Treatment
ER – Dr. Eric Ruderman
GW – Dr. Grace Wright
AO – Dr. Alexis Ogdie
Welcome to this Patient Audio Guide about psoriatic arthritis treatment. This audio guide is produced by the nonprofit CreakyJoints and the Global Healthy Living Foundation and is made possible with support from AbbVie.
Maybe you or someone you love suspects you could have psoriatic arthritis (or PsA for short), or perhaps you’ve been recently diagnosed with psoriatic arthritis. Or maybe you’ve had PsA for a while, but you’re experiencing new symptoms or are concerned that it’s getting worse.
This audio guide series can help you learn more about psoriatic arthritis and how it affects your health, so you can manage it better and start feeling better.
Remember, this is not a substitute for professional medical care. Always talk to your doctor about issues concerning your health and medical condition.
To learn more about what it’s like to live with psoriatic arthritis and to hear from fellow patients like you, check out The Psoriatic Arthritis Club podcast, available wherever you listen to podcasts or at psoriaticarthritisclub.org.
In our audio guide on psoriatic arthritis symptoms, we explained that PsA is a chronic inflammatory disease that can affect your skin and joints. It can also cause other symptoms, such as inflammation where tendons attach to bones, called enthesitis; swelling of your fingers and toes, called dactylitis; changes to the fingernails, such as pitting and thickening; and fatigue.
Not everyone with PsA will experience all of these symptoms. The combination of symptoms that you have, and how they affect you, may help determine how your doctor approaches your psoriatic arthritis treatment plan.
This audio guide will provide an overview of various treatment options for psoriatic arthritis, so you can be more informed when you talk with your doctor. But before we get into that, we need to spend some time explaining the importance of treating your psoriatic arthritis in the first place.
Let’s start by explaining what we mean when we say that PsA is inflammatory. This means that there is an abnormal response of your immune system. Your immune system is normally in charge of identifying germs and other foreign substances, but in PsA, the immune system starts attacking your own healthy tissues and cells, specifically the skin and the joints.
Here’s more on this from Dr. Eric Ruderman, a rheumatologist at Northwestern University.
ER – If you have very active arthritis, it can cause damage to your joints, and that damage may be irreversible. And so the sooner you recognize what you have, and start on some treatment that can control it, the less likely you are to have damage down the road because you’ve interrupted the process. So that’s really critical. People who have really active disease are more likely to have heart disease, they’re more likely to have strokes, they’re more likely to have vascular disease because of all the systemic inflammation that they have. There are other illnesses that are seen in higher frequency with people with psoriatic arthritis, such as inflammatory bowel disease, like colitis. Eye disease, so people with psoriatic arthritis get uveitis, which is an inflammatory problem in the eyes that needs to be managed, or it can affect your vision. The impact on your whole body by having psoriatic arthritis is driven by the inflammation. It’s not just in the joints, but it’s all through your body, it can cause all these other problems. And by controlling it, you may reduce your risk for some of these other complications.
So it’s important to understand that PsA is driven by inflammation and if your condition is not under good control, you could experience irreversible joint damage, which can impact your mobility and physical function.
Though that may sound scary or overwhelming, on the other hand, it should be reassuring to know that an effective treatment plan can help prevent further damage to joints as well as treat the other symptoms of PsA.
This may inform why your doctor is making certain treatment recommendations. Here’s more on this from rheumatologist Dr. Grace Wright.
GW – So the goal of treating psoriatic arthritis and in fact, all inflammatory arthritidities, is to number one, improve signs and symptoms. I want you to feel better. But I also want to stop what’s happening on the inside, which is damage to the joint structures, right? So yes, we’re going to look at getting rid of the stiffness and the swelling and the fatigue and the pain that you feel. But I also want to make sure that the bones are intact, that your joints are not being destroyed. So that 10, 15 years down the road, we’re forced to do surgery to fix that joint, because we didn’t save that 10, 15 years earlier. So that’s one aspect. And then when we think about the skin, yes, we would love for everybody to have 100% clear skin. And we actually do have therapies now that for some patients are able to do that. Others will get 75% improvement, 90% improvement, but really, we want to get you to the best possible place in terms of getting you back into your life. That’s kind of my threshold. Can you get back into a life where you’re not always thinking of, “Oh, my skin; oh, my joints; oh, my back; oh, I’m so tired” — where you can now take your energies and do something with them, not just sort of have to bury all the symptoms that you’re maintaining. We now have some very effective therapies that can work really well for many patients.
You may be wondering, “well, how would I know if I’m at risk for irreversible joint damage or other PsA complications?” The answer is that your doctor monitors how your psoriatic arthritis is doing to make sure your symptoms are improving and to help prevent long-term damage.
They may order blood tests to check for levels of inflammation or X-rays to look for signs of joint damage.
Your doctor may assess your overall PsA symptoms by measuring something called
minimal disease activity, which is a way to evaluate your psoriatic arthritis based on a number of different factors. It includes counting the number of tender and swollen joints you have, how much of your skin is affected by psoriasis, and how much enthesitis you have. Your doctor will ask you, as the patient, to evaluate your own pain, function, and assessment of how your disease is impacting your life.
If your score is high in most of these areas, it could suggest that your disease is not well-controlled.
On the other hand, if your score is low in most of these areas, it could suggest that your disease is being well-controlled and you would likely be feeling better.
So now let’s spend some time discussing what PsA treatment options include. The focus of this audio guide is on explaining various medications, but it’s important to note that a well-rounded treatment plan may also include physical or occupational therapy and healthy lifestyle changes, such as diet, exercise, and stress management.
Dr. Ruderman told us that he thinks about medications in two broad categories: those that only address symptoms like joint pain, and those that also address the underlying systemic inflammation process.
In addition, some medications work better for certain symptoms and not others.
ER – When I work with somebody to come up with a treatment plan for psoriatic arthritis, there are some medications that just help them with their symptoms, and don’t really address the process.
Medications in this category include non-steroidal anti-inflammatory drugs, or NSAIDs for short, such as ibuprofen. They can be prescription or over the counter. These medications can help relieve joint pain and stiffness and reduce inflammation.
Corticosteroids, including oral medications and joint injections, also fit into this bucket. They can help relieve symptoms like acute joint swelling and inflammation. They may be helpful during a disease flare-up, but they’re not recommended for long-term use in PsA.
There are also topical medications, like creams, that can be used for psoriasis. They help reduce skin inflammation caused by psoriasis plaques.
ER – And then there are a variety of medications that we think of as systemically active medications that help address the process.
By “process,” Dr. Ruderman means the systemic inflammation that is driving PsA disease activity. There are many medications in this bucket.
You may hear the term “conventional disease-modifying antirheumatic drugs” or conventional DMARDs. These are medications, often given orally, that can help relieve joint pain and stiffness. Methotrexate is an example of a commonly prescribed DMARD for psoriatic arthritis.
Another category is known as “targeted synthetic disease-modifying antirheumatic drugs.” These are oral pills that target specific parts of the immune system to help reduce inflammation. They can reduce joint pain and swelling and may help prevent long-term joint damage. These medications are often categorized as oral small molecules and include Janus kinase, or JAK, inhibitors, and PDE4 inhibitors. They may sometimes be taken in combination with some conventional DMARDs.
Another broad category is known as biologic disease-modifying antirheumatic drugs, or biologics. Given as injections or infusions, these medications act on specific parts of the immune system to help reduce inflammation. They can reduce joint pain and swelling and may help prevent long-term joint damage. There are many different kinds of biologics. They may sometimes be taken in combination with some conventional DMARDs.
Which medications you and your doctor decide on will depend on many different factors. You and your doctor should discuss things like your current symptoms, your goals for treatment, how the medication is given, the potential side effects, your health history, and the severity of your psoriatic arthritis.
Here’s Dr. Wright on the importance of getting a treatment plan that is personalized for you.
GW – So the right treatment for a patient treats the disease that they have. There are some patients that have very little skin, some that have very little swollen joints, some that it’s on the axial, some for whom function is really bad because of the fatigue, but other than that, they’re not so bad, right? So we have to think about these areas of minimal disease activity, all of the domains that we’re checking here, but then apply that to that particular person. So yes, you want your treatment to address everything, understanding that it may not be one approach, one drug that treats this, it may be that your fatigue is improved by exercise plus your medications, you may need a topical, plus your injectable or your oral, you know, in addition to changes in diet, in order to address this. But at the end of the day, I want you to have this holistic approach that addresses all of you when I manage your disease.
Dr. Ruderman explained that many patients have concerns over medication side effects. Each medication has its own set of potential side effects, or the benefit-risk profile. You should make sure to talk to your doctor about both when you’re deciding on a treatment plan.
ER – People are, you know, appropriately and understandably concerned about risks and side effects with different medications that you talk about, you know, with them, especially these days when they’ve seen commercials on TV. And, you know, they always have that list of things that could happen, some of which sound horrific. And, you know, part of my job is to say, Well, look, you know, they have to tell you all those things, but the risks are pretty low. And here’s the story. But then you also have to talk about the risk of not treating things, you know, that the alternative to not having the medicine is not zero risk, it’s the risk of having a disease that’s not well treated. And what’s that going to lead to? It’s, you have to sort of have that, that becomes part of the discussion.
Another common question that comes up about treatment is: When will it start working? When can you expect to start feeling better?
GW – So we can assess whether medication or a treatment strategy works by measuring it, right? So we can look at the skin and say, is the skin improving? We know from all of the clinical trial data how quickly we expect them to work, and how much we expect them to work. If I have you on a medicine that should work within 12 weeks, and it’s now six months and you’re still struggling, it’s clearly not working for you. But what we don’t have is a magic solution where within one week, you’re better. And I think part of it is really setting expectations that it typically takes about three months for us to see, you know, effect x, whether it’s joints getting better, skin getting better. Nails, for instance, will take sometimes a year because nails grow slowly. So it’s really sort of understanding all of these areas that we talked about, they all have their own timelines. But we know for the different agents, what those timelines are, and can help guide you so that we can, you know, level set the expectations appropriately.
You may hear other PsA patients talk about trying different medications in order to find one that works for them. Because psoriatic arthritis affects each person so differently, this “trial and error” can be a common part of your patient journey. Here’s some perspective from rheumatologist Dr. Alexis Ogdie.
AO – So sometimes patients do get really discouraged, particularly after they fail a couple drugs, for example, and I shouldn’t say that they failed the drug, the drug has failed them. So once the drug has failed you a couple times it gets frustrating. But what I’d say is, you know, hold hope because there’s many different therapies available and sometimes it’s not the first one or the second one, sometimes it’s the third one. But keep hanging in there and we can generally find something that’s going to make you feel better.
If you’re listening to this and feel discouraged about how your PsA is doing, we want to end with this insight from Dr. Wright.
GW – So the first thing I say, if you’re not doing well is that you can be better, you can be better, there are options that we have. There are things that we can do today that we couldn’t do 5, 10 years ago. And so find somebody who will listen to your voice, find your own voice, so that we can certainly start to approach you with a different set of options so that you can start to become reengaged in your own life.
We hope this audio guide has provided helpful information about the types of medication treatment options available for psoriatic arthritis, the importance of treating inflammation to reduce the risk of irreversible joint damage and control other symptoms, and why your doctor needs to know about all your PsA symptoms in order to help pick the right treatment approach for you.
Psoriatic arthritis can be a complex condition to navigate, but remember that there are many effective ways to treat PsA, especially when you partner with your health care providers. You have what it takes to deal with this.
We’d like to thank Dr. Ogdie, Dr. Ruderman, and Dr. Wright for their input and expertise. Keep listening to our audio guides for more about managing psoriatic arthritis.
For more about what it’s like to live with psoriatic arthritis, check out The Psoriatic Arthritis Club podcast, available wherever you listen to podcasts or at psoriaticarthritisclub.org.
This audio guide was made possible with support from AbbVie.
And for more information about managing PsA and to join a free, worldwide support and advocacy community of PsA patients and their families, visit CreakyJoints.org, which is a part of the nonprofit Global Healthy Living Foundation.
Audio Guide:
Understanding Healthy Lifestyle Changes for Psoriatic Arthritis
Learn more about the benefits of exercise, diet, mental well-being, and stress management. Understand how these lifestyle changes, when paired with the proper treatment plan, can play a pivotal role in managing psoriatic arthritis.











Audio Guide: Understanding Healthy Lifestyle Changes for Psoriatic Arthritis
ER – Dr. Eric Ruderman
GW – Dr. Grace Wright
AO – Dr. Alexis Ogdie
Welcome to this Patient Audio Guide about healthy lifestyle changes for psoriatic arthritis. This audio guide is produced by the nonprofit CreakyJoints and the Global Healthy Living Foundation and is made possible with support from AbbVie.
Maybe you or someone you love suspects you could have psoriatic arthritis (or PsA for short), or perhaps you have been recently diagnosed with psoriatic arthritis. Or maybe you’ve had PsA for a while, but you’re experiencing new symptoms or are concerned that it’s getting worse.
This audio guide series can help you learn more about psoriatic arthritis and how it affects your health, so you can manage it better and start feeling better.
Remember, this is not a substitute for professional medical care. Always talk to your doctor about issues concerning your health and medical condition.
To learn more about what it’s like to live with PsA and to hear from fellow patients like you, check out The Psoriatic Arthritis Club podcast, available wherever you listen to podcasts or at psoriaticarthritisclub.org.
In our other audio guides, we explained that PsA is a chronic inflammatory disease that can affect your skin and joints as well as cause other symptoms like fatigue. We addressed the fact PsA often needs to be treated with medication to reduce inflammation in order to prevent irreversible joint damage and control other symptoms.
But living a healthy lifestyle is also important in the overall management of your psoriatic arthritis.
This audio guide will provide an overview of how healthy lifestyle changes can impact your PsA management.
First, let’s hear from Dr. Eric Ruderman, a rheumatologist at Northwestern University, about how lifestyle changes fit into your overall PsA treatment plan.
ER – I think a healthy lifestyle is going to help you feel more functional. It isn’t going to control the underlying disease process necessarily. And I think that’s one of the things I do try to stress to people. It isn’t that you can say, “Oh, I’m going to eat better, I’m going to exercise. And that’s going to make this go away.” Because we don’t think it will. It may help control some of the symptoms, and may help control how much it affects you and affects what you do. But it isn’t going to make it go away. And so I really try to encourage people to think of the, you know, that sort of stuff, whether it’s diet or activity, or exercise, as an adjunct to what we’re doing as part of our medical plan. They go together, they’re not, they’re not one or the other. They’re really sort of part and parcel that go together in managing disease.
What’s more, managing PsA with medication that reduces inflammation and disease activity may help you live a healthier lifestyle. When you have less pain and inflammation, you may sleep better and have less fatigue. You may have more energy for physical activity and preparing healthy meals, which, in turn, may help you better manage your PsA.
Here’s how rheumatologist Dr. Grace Wright thinks about it.
GW – It’s important to recognize that when you treat the underlying drivers of inflammation that there are many added benefits. So yes, sometimes depression, the stiffness, the fatigue, the ability to be present at work, the ability to connect with others socially, it’s really hard to maintain that social connectedness, when people are sort of backing away from you, because you’ve got these swollen joints and flaring red skin, and they don’t really understand why that’s the case. So you know, this total approach to care has all of these unintended or intended consequences that are beneficial to patients. It’s about your wholeness as a human being that we want to make sure you’re reconnected, you’re engaged, and you’re able to function well.
The importance of treating the whole patient ties back to how doctors evaluate how well-controlled your PsA symptoms may be and how making healthy lifestyle changes may impact your symptoms. This idea is similar to a clinical assessment measure called minimal disease activity, where rather than looking at one or two symptoms, like just skin symptoms or just joint pain, minimal disease activity takes into account many different aspects of psoriatic arthritis in order to make sure that the condition is getting better across many aspects of the disease.
To assess minimal disease activity, your doctor will ask about or check for tender and swollen joints, whether you have any enthesitis (inflammation of tendons and ligaments), how much of your skin is affected by psoriasis, patient reports of pain, daily function, and how you’re feeling overall. You have to score low in most of these areas in order to be considered to have minimal disease activity.
And making healthy lifestyle changes as part of your treatment plan can be an important part of working to manage your overall health.
Here’s Dr. Alexis Ogdie, a rheumatologist at the University of Pennsylvania, discussing how lifestyle changes can help improve your PsA management.
AO – I cannot overemphasize how important it is to have a healthy lifestyle. And there’s so many reasons why, but I’ll give you a few. So number one is function and how you’re functioning in life is so much more than just your disease. So you have a lot of power to help with your own function. And that’s through exercise, making sure all the muscle groups are working well. A lot of people say that when they first start exercising, they get extraordinarily fatigued and they have more pain, you got to make it over that fence and then regular exercise will actually help keep your functional status up. Number two is diet matters. Patients with psoriatic arthritis have a really high prevalence of obesity. Obesity impacts function, but obesity also impacts the likelihood of your response to therapy. So if you can maintain a healthy weight, you’re much more likely to respond to your therapy. In addition, maintaining healthy mental energy is so important. If you think about just like anything going wrong in your day, if you’re in a good place mentally and emotionally, you’re much more able to deal with that. Well, the same thing is true for psoriatic arthritis. Let’s say you have a flare. If you’re in a good place emotionally, you’re going to be able to deal with that a lot better. Additionally, depression, anxiety and stress cause flares. And they actually increase the disease activity that you’re experiencing, increasing the impact of disease on your life.
So let’s talk about the components of managing PsA with healthy lifestyle changes. It starts with being physically active. It’s always a good idea to talk to your doctor about safe physical activity for you. A mix of aerobic exercise, stretching, and strength training is often recommended, but it needs to be catered to your abilities and level. If it’s been a long time since you’ve been physically active, consider this tip from Dr. Ogdie.
AO – Physical therapy is a great place to start if it feels like too much at first. Water therapy is actually a great place to start because it’s getting into a warm pool where they’re starting to get things moving, and you don’t have the gravity on the rest of your body. So it’s a great place to start if you’re really having a lot of pain. Once you move from water therapy to physical therapy, kind of land physical therapy, they can start working on those different joint muscle groups that need strengthening, and other ones that need stretching.
Another issue is having enough energy for exercise. When you have fatigue, which is very common with PsA, exercise may be the last thing on your mind. But research actually shows that exercise can help manage fatigue.
AO – Aerobic exercise can be really important, that’s counterintuitive to people who are really fatigued. Because you don’t want to go exercise and feel like, initially, it makes you feel worse. But actually, the best demonstrated therapy for fatigue is, or one of them at least, is to go get regular aerobic exercise. And then over time, over the next few weeks, for example, you will start to feel less fatigue. I also say that, with aerobic exercise, you don’t necessarily need to go out there and start with like 20 minutes every day. It could be, if five minutes is causing you a lot of fatigue, start with five minutes or four minutes and then slowly build up over the course of a few weeks. So start slow and increase slowly.
Another component of a healthy lifestyle with PsA is diet. While there’s no one diet that is recommended for psoriatic arthritis, it’s generally a good idea to eat nutritious, well-rounded meals that include fruits and vegetables, beans, nuts and seeds, whole grains, fish, lean meat, and healthy fats like olive oil and that limit sugar and highly processed foods. You may hear this referred to as a Mediterranean diet or an anti-inflammatory diet.
Here’s how a healthy diet can affect your PsA.
AO – So a healthy diet is more than just being good to yourself, but it can help improve your energy levels, and number two, they decrease your risk for heart disease and help you maintain a healthy weight. Having obesity or being obese, or even overweight is associated with poor outcomes for patients with psoriatic arthritis and we want people to maintain a healthy weight so they can respond better to their therapies.
A healthy lifestyle with PsA also means managing stress levels and mental health. This includes having stress-reducing activities in your routine and taking time for self-care. It’s also good to talk to your doctor if you have any concerns about your mental health. They can advise on whether additional treatment, such as seeing a therapist or medication, could be helpful.
AO – So at every visit, I ask about depression and anxiety, and one is because it’s really really common. It’s common in everybody, but it’s particularly common in psoriatic arthritis.
In some cases, people may not even recognize that they are experiencing mental health issues. And your doctor may help you identify that, as Dr. Wright explains.
GW – The first thing that we can do when we have patients who have mental health issues is, number one, assess whether or not they’re even aware that this is a mental health issue. Many patients don’t realize that their behaviors are driven by depression. So the fact that you’re always tired, you’re never able to get out of bed — I may be able to uncover the depression. And even though I’m not an expert in treating the depression, I can refer you to somebody who can help. So you know, again, identifying the behaviors, and getting people number one to accept that mental health is just that. There’s physical health, there’s mental health, there’s emotional health. And this is an area that sometimes we need help with. And there are professionals who can assist with this.
In addition to exercise, diet, and stress and mental health, there are many other components of living a healthy lifestyle with PsA. You may want to try physical or occupational therapy. You can use treatments like heat or ice to manage pain and swelling. You may want to make changes to your routine to help you sleep better, such as having a set bedtime and minimizing your caffeine intake. And, of course, quitting smoking may help improve your PsA and overall health in many different ways.
Keep in mind that you don’t have to make all of these changes at once. Adjusting to life with a chronic disease is a lot. And make sure to partner with your healthcare provider on your PsA patient journey. They are there to help you. The more you tell them about what’s going on, the more they may be able to help.
AO – Patients should feel like they have a doctor who’s partnering with them and listening to them and taking into account what’s important to them. Every patient should have the opportunity to give their treatment goals, to have their treatment goals heard, and have the rheumatologist give them a plan for how to achieve their goals.
Achieving treatment goals often entails a combination of medications and lifestyle adjustments. Here’s an example from Dr. Ogdie of what this partnership could look like.
AO – Let’s say you want to be able to walk two miles, and you’ve only been able to walk around the block. So we should be able to help think through, “well, what do we need to do to do that?” Your knee is inflamed right now, maybe we can do a joint injection to make the knee better. Then we need to get you to physical therapy so you can strengthen the muscles around the knee. And then you need to start slowly increasing your walking. You’re going to do this a little bit every time. And maybe we’ll think about a knee brace to help get that knee more stable because if it’s wobbling while you’re walking, that’s maybe part of the problem. So we should be able to help you think through at a granular level, what can we do to get you to help achieve your goal?
We hope this audio guide has provided helpful information about healthy lifestyle changes for psoriatic arthritis and how lifestyle changes and medication work together to help you manage your condition.
Psoriatic arthritis can be a complex condition to navigate, but remember that there are many effective ways to treat PsA, especially when you partner with your health care providers. You have what it takes to deal with this.
We’d like to thank Dr. Ogdie, Dr. Ruderman, and Dr. Wright for their input and expertise.
Keep listening to our audio guides for more about managing psoriatic arthritis.
For more about what it’s like to live with psoriatic arthritis, check out The Psoriatic Arthritis Club podcast, available wherever you listen to podcasts or at psoriaticarthritisclub.org.
This audio guide was made possible with support from AbbVie.
And for more information about managing PsA and to join a free, worldwide support and advocacy community of PsA patients and their families, visit CreakyJoints.org, which is a part of the nonprofit Global Healthy Living Foundation.
BEHIND THE MIC
The Psoriatic Arthritis Club features host Deanna Kizis, a PsA patient looking to connect and learn from other people living with PsA, and insights from top psoriatic arthritis experts.


Shelley Fritz
Patient-Centered Engagement and Insights Manager, GHLF
Shelley engages in communication efforts, supports patient advisory boards, and contributes to patient-informed protocol design for research projects. Shelley also supports patient-focused content. She brings 28 years of experience in public education and a unique perspective as a patient living with rheumatoid arthritis, fibromyalgia, and celiac disease.


Angela Degrassi
Research Manager for Patient-Centered Research, GHLF
Angela organizes projects, connects patients to resources through ArthritisPower, and brings leadership experience from the health and fitness industry. As a lifelong patient advocate and caregiver to a parent with MS, she brings a unique perspective to her work.


Deanna Kizis
Deanna Kizis is an author, journalist, and screenwriter who has written two novels, a children’s book, and more articles than she can count about culture, health, architecture, design, Hollywood, and broken hearts. Diagnosed with psoriatic arthritis several years ago, Deanna is a reluctant member of this “club” but says that working on this podcast has given her hope and a valuable connection to those who are also living with PsA.


Eric Ruderman, MD
Rheumatologist
Dr. Ruderman is a rheumatologist and the Associate Chief, Clinical Affairs for the Division of Rheumatology at Northwestern University, where he has been running a psoriatic arthritis clinic with dermatology colleagues for nearly 20 years.


Grace Wright, MD
Rheumatologist
Dr. Wright is a consultant rheumatologist in New York City and served as Clinical Associate Professor of Medicine at NYU Medical Center. She is the President of the Association of Women in Rheumatology (AWIR).


Alexis Ogdie, MD
Rheumatologist
Dr. Ogdie is a rheumatologist and Associate Professor of Medicine and Epidemiology at Hospital of the University of Pennsylvania. She treats PsA patients in the Psoriatic Arthritis Program at Penn Medicine and specializes in PsA research.
More Resources
Living with psoriatic arthritis (or caring for someone who is coping with psoriatic arthritis) isn’t easy. There’s a lot to learn about symptoms, treatments, and staying healthy. CreakJoints, a non-profit patient community for people living with arthritis and rheumatic conditions, has plenty of resources, always free, to provide help and support.
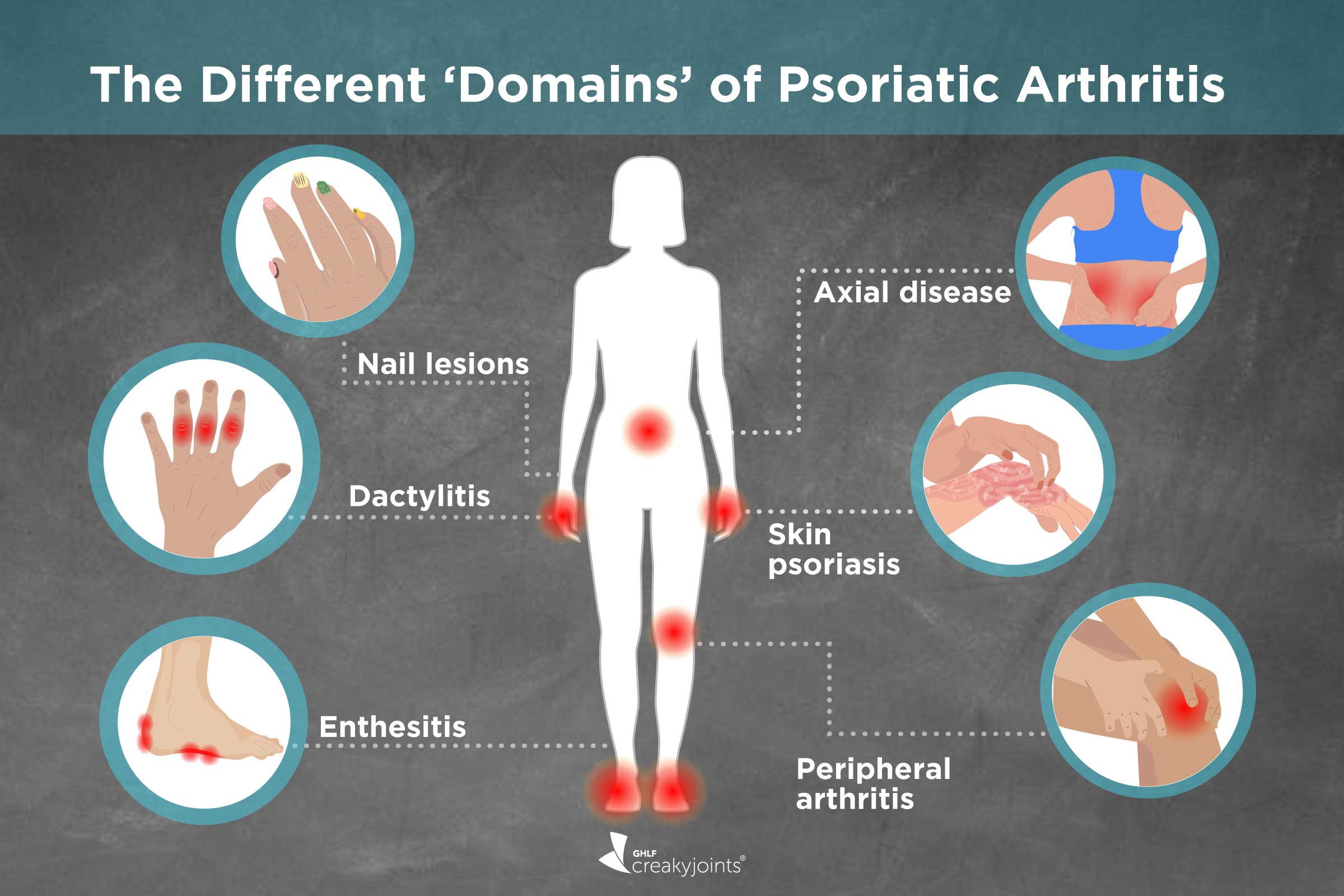
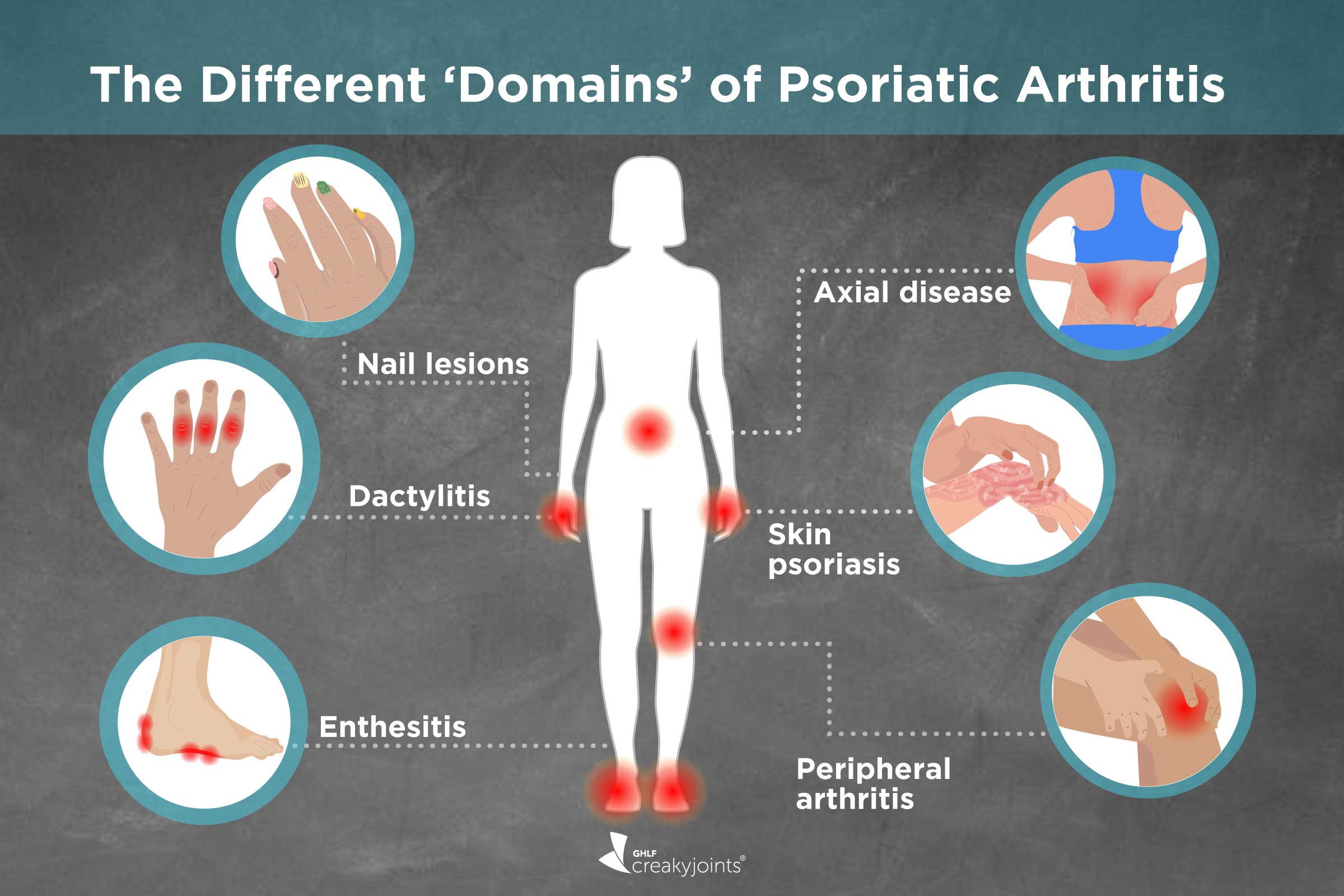
Is Your PsA Treatment Working? Red Flags to Raise with Your Doctor
Frequent flare-ups, fatigue, or difficulty with daily tasks might signal a medication change. Learn how to talk to your doctor about these signs for improved care.
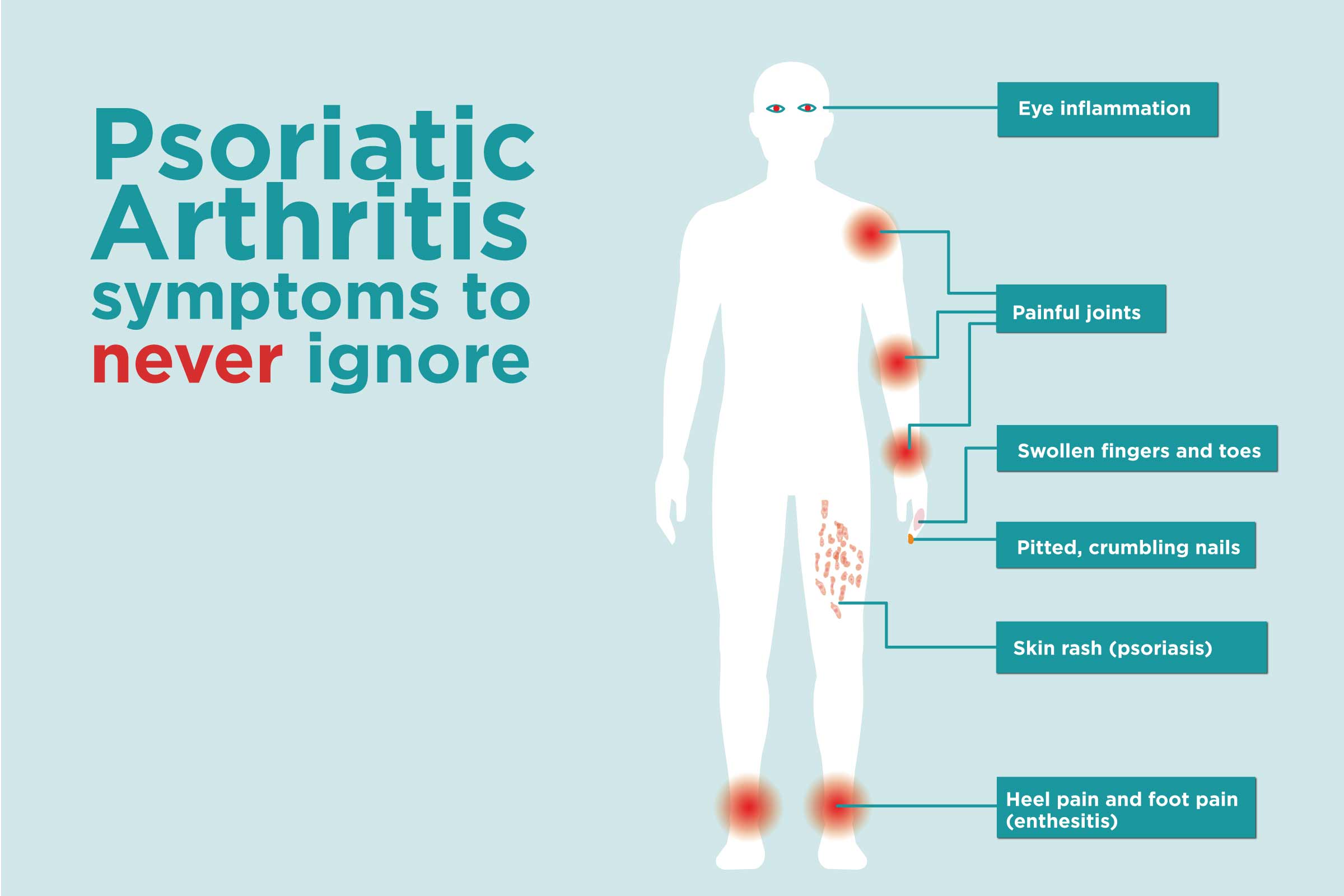
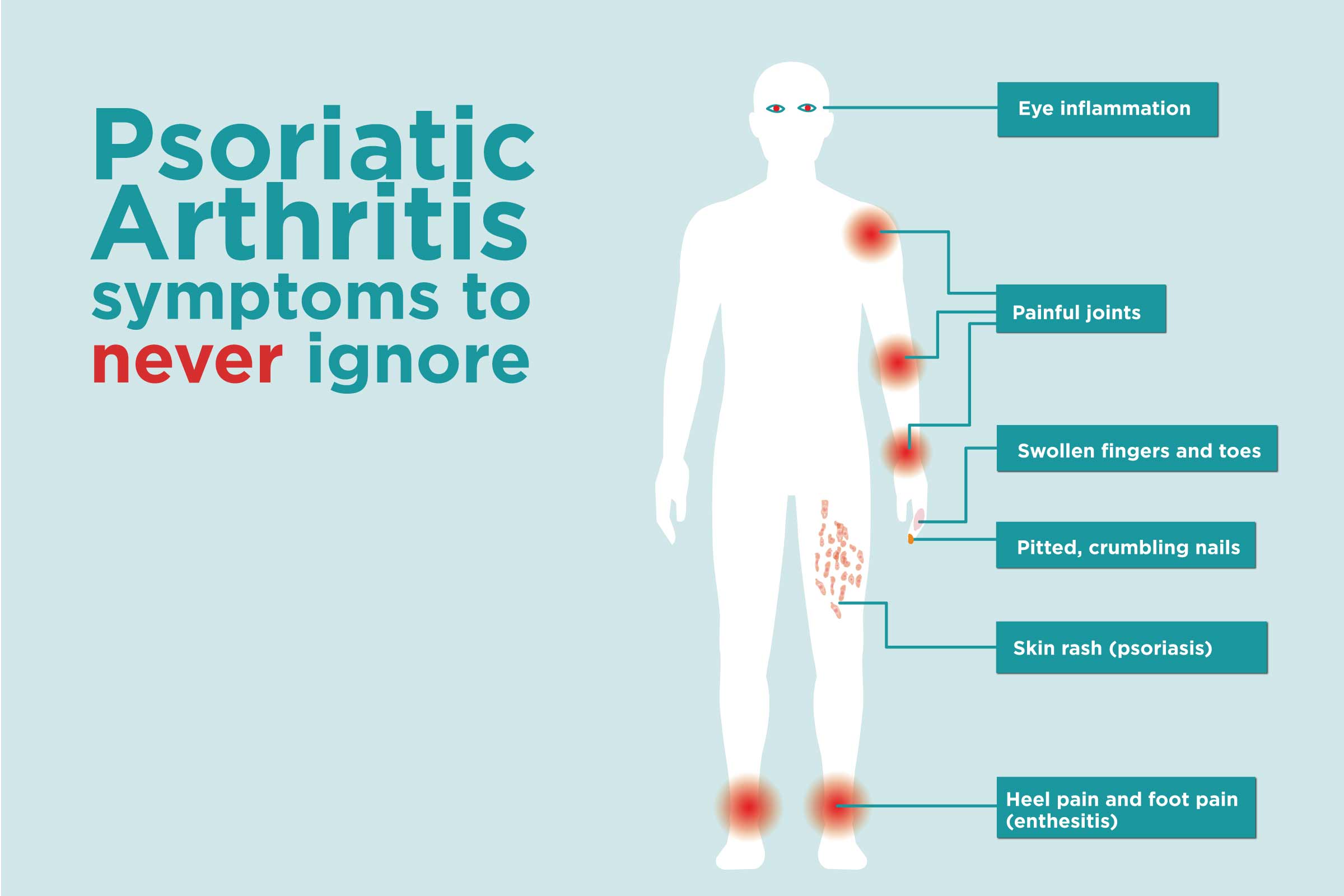
Understanding the Visible and Invisible Symptoms of Psoriatic Disease
Explore the complexities of psoriatic disease, from the hallmark symptoms like itchy skin and swollen joints to the hidden emotional and physical tolls.
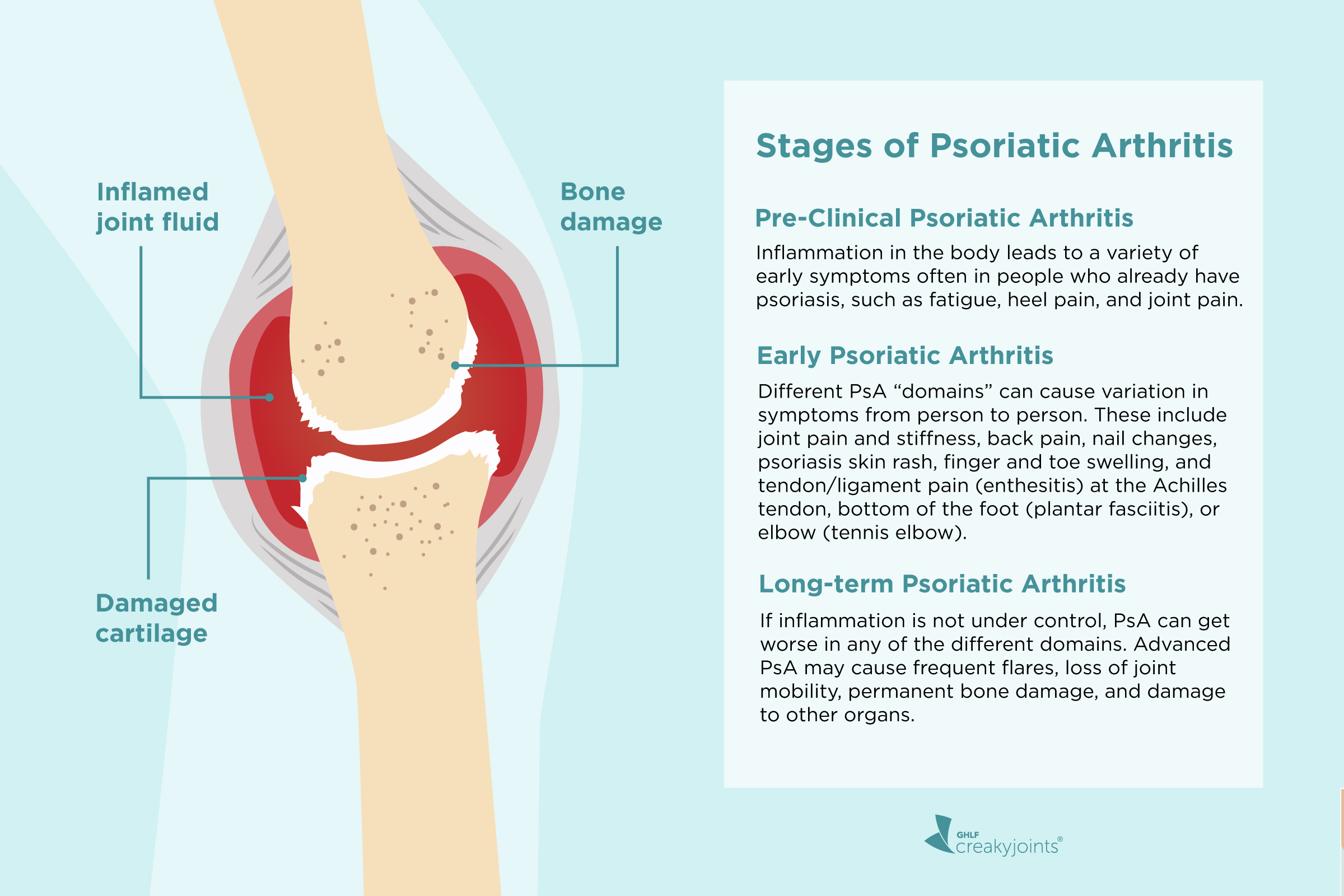
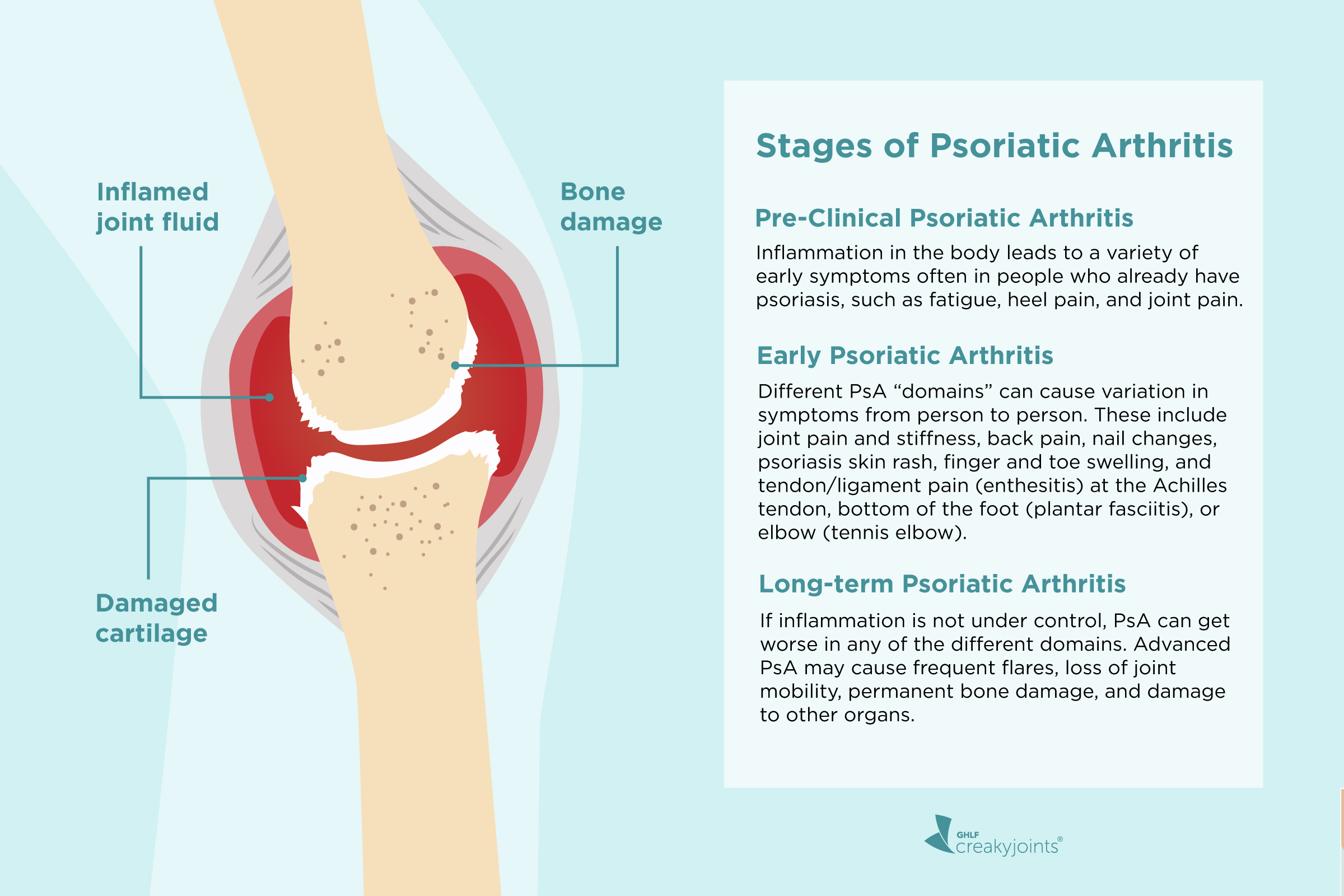
Stages of Psoriatic Arthritis: Signs of Early to Late Disease Progression
Psoriatic arthritis is not a one-size-fits-all disease, and the stages and progression are not straightforward or uniform from patient to patient.
FIGHT BACK AGAINST INFLAMMATION: A PATIENT’S GUIDE
A New Audio Guide Mini Series About Inflammation
LISTEN TO OUR AUDIO GUIDES
Our new audio guides, “Fight Back Against Inflammation,” produced by the nonprofit CreakyJoints and the Global Healthy Living Foundation and made possible with support from UCB, will focus on the
critical topic of inflammation and its impact on psoriatic arthritis (PsA) as well as other types of inflammatory arthritis like axial spondyloarthritis (axSpA).
Inflammation is a subject close to our hearts because, when left unchecked, it can bring about many added challenges for our patient community — from joint pain and fatigue to lost days, gaps in memory, and lack of mobility. Join us as we explore how understanding and managing inflammation can significantly improve your journey with these conditions.
Part One
Understanding and
Identifying Inflammation
Dr. Jeff Stark, rheumatologist and Head of Immunology Medical at UCB, shares his expertise on inflammation and helps us understand why inflammation matters, how it affects our daily life, what signs to look for, and how doctors check for it. Let’s unravel the mystery of inflammation together.
Part Two
Managing and Treating
Inflammation
Dr. Jeff Stark, rheumatologist and Head of Immunology Medical at UCB, shares tips on how to talk with your health care team, what treatments are out there, how lifestyle changes can help, and what you can do to feel your best every day. Let’s take positive steps toward fighting inflammation together.
BEHIND THE MIC


Dr. Jeff Stark
Rheumatologist and
Head of Immunology Medical at UCB
Jeffrey Stark, MD, leads the medical affairs teams across rheumatology, dermatology, and gastroenterology. Prior to joining UCB, Dr. Stark spent several years running a full-time rheumatology clinical practice. He has served on the board and the development council of the American College of Rheumatology (ACR) Rheumatology Research Foundation and is a member of the Medical Advisory Board of the Georgia Chapter of the Lupus Foundation. Dr. Stark is also a past President and Executive Board Member of the Georgia Society of Rheumatology.
More Resources


Your Guide to Understanding Arthritis Inflammation
Discover why keeping tabs on inflammation is crucial for managing your condition and overall health and learn how to effectively monitor and interpret it as a proactive patient.


The Impact of Inflammation and How to Talk to Your Doctor
Discover the importance of understanding and discussing inflammation with your doctor — and get tips on communicating with your care team to better manage your health.
Subscribe for More Psoriatic Arthritis Resources
By subscribing, you agree to receive emails from CreakyJoints and its parent organization, Global Healthy Living Foundation. We will never sell your data. See our Privacy Policy.






The Psoriatic Arthritis Club is a new podcast series produced by the non-profit Global Healthy Living Foundation, its arthritis patient community CreakyJoints, and made possible with support from AbbVie.
The Psoriatic Arthritis Club Audio Guide, Fight Back Against Inflammation and Season 3, was produced by the non-profit Global Healthy Living Foundation, its arthritis patient community CreakyJoints, and made possible with support from UCB.
Our podcasts and audio guides are for educational purposes only and shouldn’t take the place of medical advice. Always talk to your doctor about the right path for you.