Check out Psoriasis: An Inside Out Disease for more information on this topic.
When you think about psoriasis, flaky skin or plaques might come to mind. However, psoriasis is not just skin-deep; it is a disease that can impact your entire body, inside and out.
“While psoriasis is a skin manifestation, there are other domains outside of skin that are involved in patients who have psoriasis,” says Saakshi Khattri, MD, a board-certified dermatologist, rheumatologist, and internist, and an Associate Professor at Mount Sinai. “Clearly, it’s not something that’s skin-limited, but rather systemic [whole body].”
Psoriasis affects individuals differently, so it’s crucial to personally take control of your treatment and well-being. This includes knowing when to start a conversation with your doctor about treatment escalation, which may involve moving from a topical treatment to a systemic one.
“There’s an issue with patients not knowing that psoriasis extends beyond the skin,” says Dr. Khattri. “Knowledge is power and the first step is for patients to know the other manifestations associated with psoriasis — and then to see a provider who looks at the full picture.”
While there is currently no cure for psoriasis, certain treatments can help keep symptoms under control, per the National Institutes of Health (NIH).
There are several options currently available to help clear skin lesions, both topical (applied directly to a specific part of the skin) and systemic (injected or taken orally, impacting the entire body). Topical therapies are often the first line of psoriasis treatment and may include creams, ointments, and lotions, which often contain corticosteroids. Meanwhile, systemic therapies may include oral retinoids, biologic response modifiers (which are injected), and immunosuppressants. These are usually used to advance psoriasis treatment.
“We have so many advanced therapies, which are very effective and quite safe to use,” says Samardeep Gupta, MBBS, Associate Professor of Rheumatology at the University of Michigan Medical School. “Some studies show the reduction in cardiovascular mortality and morbidity when we use appropriate advanced therapies.”
The number of psoriasis patients using systemic treatments is growing: Those with psoriasis managed with conventional systemic treatments increased from 11.4 percent in 2009 to 13.9 percent in 2019, while those with psoriatic arthritis (PsA) on conventional systemic treatments increased from 37.7 to 49.3 percent, per a 2023 review in Annals of Dermatology.
As you work with your doctor to determine the best treatment, the most important thing you can do is adopt a proactive mindset. Avoid comparing the severity of your condition to others — feeling like your psoriasis “isn’t that bad” shouldn’t deter you from seeking the best possible care and treatment outcomes.
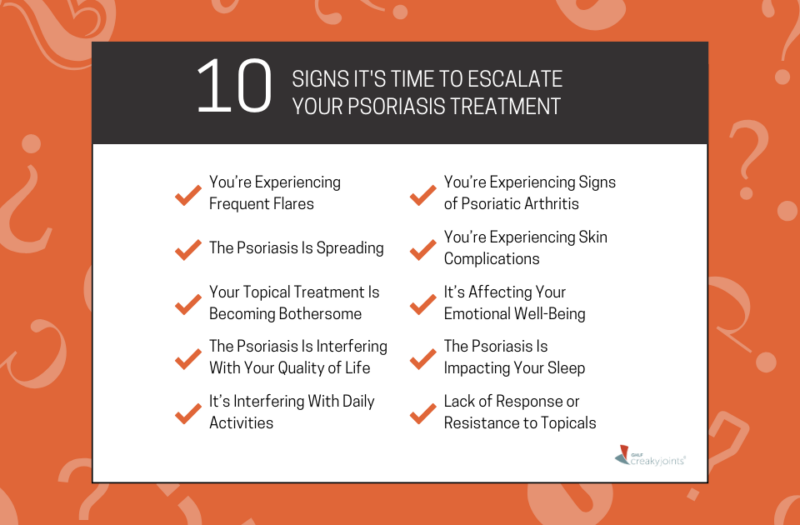
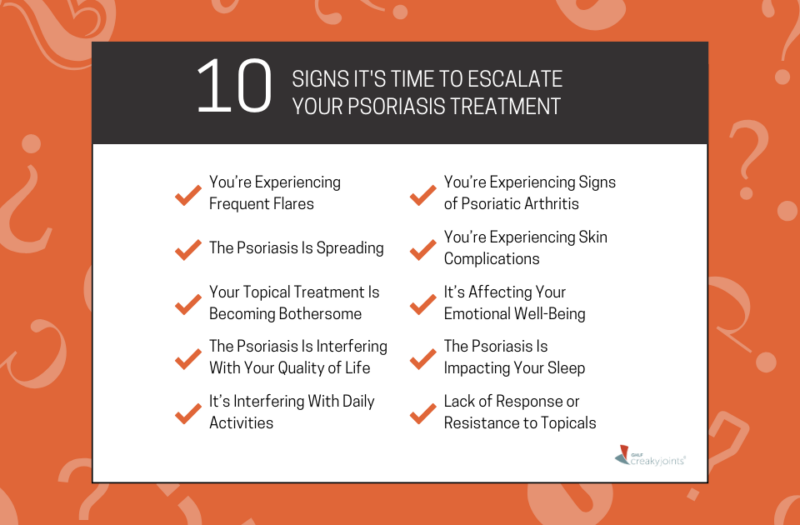
Is It Time to Escalate Treatment?
Here are 10 signs that it may be time to escalate your psoriasis treatment. You don’t need to have all of them to consider making a change in your treatment plan. Being proactive means starting conversations about your care early.
1. You’re Experiencing Frequent Flares
The anxiety of flares, even if they aren’t very frequent, can have a significant impact on your life. A flare is defined as a time in which your psoriasis symptoms get worse, followed by a period of feeling better, per the NIH.
Nicole Safran, a 32-year-old nursing school student and epidemiologist in New York City, says she put off escalating her psoriasis treatment at first, attributing flare-ups to weather or stress.
“I would have flares where I would get plaques on my scalp, but I figured it’s not my whole scalp, so it’s not that bad,” says Safran. “I was definitely dismissing myself when I realized the flares kept coming more and more frequently.”
Switching doctors helped Safran get the right treatment plan, something she encourages other patients to do as soon as possible. Previously, she had tried multiple prescription shampoos, corticosteroid treatments, and salicylic acid softeners, but none of them effectively treated the psoriasis. After finding a new doctor, she was diagnosed with psoriatic arthritis.
“I wasn’t comfortable with my first doctor and felt like there was something wrong,” says Safran. “Every time she did lab values, they were more and more elevated, but she brushed me off. I was able to switch doctors and now I have a good treatment plan, or hopefully will soon.”
Shortly before we spoke with Safran, she had started taking a new systemic treatment. Although she says it’s too early to tell how well it’s working, she says she learned a valuable lesson in advocating for herself and seeking treatment options early. “Looking back, I wish I was more vocal and willing to try something, because for a period of time I was really self-conscious about my appearance based on my scalp,” says Safran.
If your current treatment isn’t working or it has lost its efficacy, get in touch with a doctor who you can speak to honestly — and who answers your concerns and questions. “One treatment or one mechanism of action is not the answer for all patients,” says Khattri. “We are fortunate because we have more than a dozen options to choose from in terms of systemic treatment for psoriasis. If a patient does lose efficacy with their treatment, hope is not lost.”
2. The Psoriasis Is Spreading
If you notice psoriasis lesions appearing in new areas of your body, this may be a sign that your current treatment isn’t effective enough. “If a patient with psoriasis has it on more than five percent of their body surface area, that’s when we trigger the systemic therapies,” says Dr. Gupta.
For context, the size of your hand is about one percent of your body surface area. Your doctor may also consider the area the psoriasis is spreading to when considering treatment escalation (for instance, lesions in sensitive areas like the ears can be very debilitating).
Even if it hasn’t spread yet, the anxiety around where psoriasis may show up next can impact your emotional well-being. While it can be helpful to log any changes you note at home, your doctor will also likely take photos at each appointment to track changes based on your treatment.
“I always take pictures of my patients with psoriasis before I start them on treatment, especially if I’m starting them on systemic treatment,” says Dr. Khattri. “That visually reinforces to them and to me whether or not the drug is working.”
3. Your Topical Treatment Is Becoming Bothersome
While topicals are typically a first line of treatment for psoriasis, they can quickly become cumbersome and aren’t realistic for everyone.
Dr. Khattri asks patients questions to gauge that:
- How impactful has this topical been?
- Can you fit it into your day-to-day schedule?
- Can you commit to putting different topicals on different parts of your body? (For instance, you may need to use a high-potency steroid for your hands, but a mild steroid for your face.)
Some patients may feel that applying ointments twice per day takes away from their quality of life. “You have to wait for it to get absorbed, and even then, it doesn’t absorb completely and it comes off on your clothing — it’s a pain,” says Dr. Khattri. “If they’re bothered by spending time twice a day applying a slew of different topicals to different parts of their body affected by psoriasis, I have a conversation about systemic treatment options.”
If you’re experiencing the need for frequent applications or have skin irritation, these may also be signs that a different treatment approach is needed.
4. The Psoriasis Is Interfering with Your Quality of Life
The physical, emotional, and mental toll of psoriasis can impact your work, social, and romantic life.
“I’ve definitely felt anxiety, especially with meeting new people and dating,” says Safran. “At times, I feel really self-conscious and embarrassed. I’ve had people ask if I’m contagious and that is so humiliating.”
Safran adds that she recently started wearing a hat more often, but that there are certain places she can’t do so (like at her nursing school). When she’s having a flare, she changes what she wears — opting for lighter clothes to hide the flakes — and the way she styles her hair.
If you’re experiencing a dip in your quality of life due to psoriasis, it’s time to talk to your doctor about escalating your treatment. Psoriasis can affect several pillars of your life: A 2021 study in JAAD International found that 10 percent fewer patients with psoriasis were employed six years after diagnosis compared to controls. Meanwhile, after four years of follow-up, 1.4 percent fewer patients with psoriasis were married.
A 2010 study in the Journal of the European Academy of Dermatology & Venereology also found that psoriasis patients experience a productivity loss of about 10.7 percent, without significant differences based on the severity of the disease.
5. It’s Interfering With Daily Activities
Even if it’s simply an inconvenience, psoriasis that interferes with your ability to do daily activities like dressing, exercising, or going to the nail or hair salon should prompt a discussion about treatment escalation.
“Because I’m a lawyer and in suits a lot, and my symptoms are on my head, it looks like dandruff,” says Hunter Garnett, a 31-year-old personal injury lawyer at Garnett Patterson Injury Lawyers in Huntsville, AL, who developed psoriasis a year ago. “I think there’s probably a lot of people who don’t do anything about psoriasis until they have really visible, embarrassing symptoms. It would be so much easier if you get on top of it when it’s a mild inconvenience.”
Garnett started with topical treatments, which he says didn’t help much. After a month or two, he tried injections and then twice-daily pill prescription. Recently, he started a once daily biologic. “It’s helping more than anything else that I’ve done, but I’ve only been on it for a few days,” says Garnett.
If psoriasis is impacting your quality of life, making your everyday living uncomfortable or simple to-do’s into hassles, talk to your doctor.
“Especially if it’s in a sensitive area like the groin, genital area, or scalp, psoriasis can be very disabling and patients might not be able to do things like work,” says Dr. Gupta. “If their social life is being impaired because of their psoriasis, they should seek the appropriate therapy, which could be systemic.”
Dr. Khattri notes that some patients may initially feel uncomfortable discussing psoriasis in sensitive areas like their genitals or under the breasts, but it’s crucial to have that conversation. “It’s important to remove the stigma of having that conversation,” says Dr. Khatti. “The first step to any discussion is knowledge and asking.”
6. You’re Experiencing Signs of Psoriatic Arthritis
There’s not one blood test that can determine if you have psoriatic arthritis (PsA), so it can be challenging to diagnose. It’s key to stay vigilant and look out for early symptoms that may indicate the need for more aggressive treatment.
“About a third of patients with psoriasis will go on to develop psoriatic arthritis, but generally there’s a delay of seven to 10 years,” says Dr. Khattri. “A lot of patients I see with psoriasis don’t know about the association with psoriatic arthritis, so there’s a knowledge gap that exists.”
Symptoms of psoriatic arthritis may include joint pain, stiffness, discoloration or redness near affected joints, pain or tenderness where tendons and ligaments meet the bones, swelling in your fingers and toes, psoriasis rash, nail psoriasis, and fatigue, per the Cleveland Clinic.
A 2015 study in Arthritis Care & Research found that psoriasis patients had significantly higher prevalence of lower back pain compared to a non-psoriasis group (31.1 percent versus 18.9 percent, respectively) and alternating buttock pain (7.2 percent versus 2.4 percent). They were much more likely to have psoriatic arthritis (14.3 percent versus 1.5 percent).
“We believe that psoriatic arthritis is evident if they have inflammation,” says Dr. Gupta. “Besides your pain, there’s also redness, swelling, and heat on the joint — or the inflammation is in the tendon, like the Achilles tendon, and they can’t walk.”
Symptoms may also show up as related conditions like inflammatory bowel disease like Crohn’s disease or eye inflammation. If a patient is experiencing symptoms and they’re currently on a topical psoriasis treatment, it points to the need for more aggressive treatment.
“At this point, we have to move on to systemic therapies, because topical therapies are not going to penetrate the joints,” says Dr. Gupta.
7. You’re Experiencing Skin Complications
While psoriasis itself isn’t contagious and doesn’t cause skin infections, untreated psoriasis can lead to certain skin issues.
“Most patients that have psoriasis don’t have skin infection on their lesions, but you could have an infection with genital psoriasis because it’s a moist, sweaty, warm environment,” says Dr. Khattri. “In that case, a superimposed candidal infection could occur on a psoriasis lesion.”
A candidal infection is also commonly known as a yeast infection. If you’re experiencing other complications like this in addition to your psoriasis, speak to a doctor.
8. It’s Affecting Your Emotional Well-Being
Living with psoriasis isn’t just about physical symptoms — it can also affect how you feel emotionally and mentally.
People with psoriasis are 1.5 times more likely to experience depressive symptoms than the general population and the prevalence of anxiety and suicidal ideation is higher in patients with psoriasis (20 to 50 percent and 12.7 percent, respectively) than those without it, according to a 2022 study in the journal General Hospital Psychiatry.
“When we treat psoriatic arthritis, patients’ depression and anxiety gets better as well,” says Dr. Gupta. “There are many variables…maybe it’s because they’re feeling better about themselves, or maybe drugs are independently changing the disease process.”
Make sure conversations about your psychological well-being are included in conversations with your doctor. Your doctor may recommend additional medication like an antidepressant, if needed.
9. Psoriasis Is Impacting Your Sleep
Itchiness, discomfort, and pain from psoriasis can disrupt your sleep patterns. In a 2019 Dermatology and Therapy study, 58.4 percent of participants with psoriasis reported sleep difficulty and 38.8 percent reported low sleep quantity (less than seven hours per night).
“Up to seven out of 10 patients with psoriasis complain of itching, burning, pain, and discomfort in their psoriasis lesions,” says Dr. Khattri. “Having all of those can certainly impact quality of life and sleep.”
Getting proper sleep is important for overall health, so discuss these sleep disturbances and potential treatment options with your doctor.
10. Lack of Response or Resistance to Topicals
As mentioned previously, new flare-ups may be a sign that your treatment is not working or no longer working. Some individuals with psoriasis can develop resistance to topical treatments over time, in which those treatments become less effective. “Any time a treatment is not helping a patient enough, we start looking at systemic therapy,” says Dr. Gupta.
If you’ve been consistently using topical treatments without significant improvements, that might be a sign that a more robust treatment approach — like systemic medications — is needed to better control your condition.
How to Talk to Your Doctor About Treatment Escalation
If your current treatment isn’t working as expected, it’s important to talk openly with your doctor. Share your treatment expectations, including the goal of achieving almost complete skin clearance. During these conversations, it’s key to ask questions, express concerns, and actively participate in shared decision-making with your doctor to find the most suitable treatment plan for your unique needs.
“My doctor would walk over every lab test with me and also said, ‘I don’t know’ multiple times, which I really appreciate,” says Safran. “If you don’t know something, I want you to be honest with me, because it’s my life. I’ve had doctors look up information while I’m there and I don’t mind because I want to make sure I’m getting accurate information.”
When speaking with your doctor, make sure that:
- You are comfortable asking questions and voicing concerns.
- Your doctor is not brushing you off or dismissing you.
- Your doctor communicates with your other providers for health history and treatment information.
- You are honest about all side effects from medication and new flare-ups.
This shared decision-making, along with recognizing the signs above early on, will help you find the most suitable treatment plan for your unique needs.
Join GHLF’s HEROES Program
GHLF invites you to make a difference in your community with our FREE and unique program called HEROES (Health Education + Reliable Outreach + Empathetic Support). HEROES is a FREE education and outreach initiative that equips beauty professionals to better support clients living with scalp and other skin conditions and offers people living with skin and scalp conditions helpful resources and information on getting a proper diagnosis, managing symptoms, and becoming an empowered patient. To learn more, visit GHLF.org/HEROES today.
This article is part of Psoriasis: An Inside Out Disease and was made possible with support from Amgen.
Interview with Saakshi Khattri, MD, a board-certified dermatologist, rheumatologist, and internist, and an associate professor at Mount Sinai.
Interview with Samardeep Gupta, MBBS, Associate Professor of Rheumatology at the University of Michigan Medical School.
Choi S, et al. Trends in Systemic Psoriasis Treatment: Is Psoriasis Still Being Undertreated? Annals of Dermatology. August 2023. doi: https://doi.org/10.5021/ad.21.151.
Häbel H, et al. Societal impact for patients with psoriasis: A nationwide Swedish register study. JAAD International. March 30, 2021. doi: https://doi.org/10.1016/j.jdin.2021.02.003.
Hedemann, T, et al. “Associations between Psoriasis and Mental Illness: An Update for Clinicians.” General Hospital Psychiatry. March 2022. doi: https://doi.org/10.1016/j.genhosppsych.2022.01.006.
McDonough E, et al. Depression and anxiety in psoriatic disease: prevalence and associated factors. The Journal of Rheumatology. May 2014. doi: https://doi.org/10.3899/jrheum.130797.
Meyer N, et al. Psoriasis: an epidemiological evaluation of disease burden in 590 patients. Journal of the European Academy of Dermatology & Venereology. September 2010. doi: https://doi.org/10.1111/j.1468-3083.2010.03600.x.
Psoriasis: Diagnosis, Treatment, and Steps to Take. National Institutes of Health. October 2023. https://www.niams.nih.gov/health-topics/psoriasis/diagnosis-treatment-and-steps-to-take.
Psoriatic Arthritis. Cleveland Clinic. September 19, 2023. https://my.clevelandclinic.org/health/diseases/13286-psoriatic-arthritis.
Smith MP, et al. Factors Influencing Sleep Difficulty and Sleep Quantity in the Citizen Pscientist Psoriatic Cohort. Dermatology and Therapy. September 2019. doi: https://doi.org/10.1007/s13555-019-0306-1.
Thom N, et al. Prevalence of chronic axial pain, inflammatory back pain, and spondyloarthritis in diagnosed psoriasis. Arthritis Care & Research. May 2015. doi: https://doi.org/10.1002/acr.22528.





