You’ve tried NSAIDs. You’ve tried physical therapy. You’ve even tried steroid injections. When nothing works for the chronic pain of osteoarthritis, it can leave you feeling defeated. But there may be hope in a procedure for treating certain kinds of OA, including the spine and knee: radiofrequency ablation. We asked two doctors who regularly perform the procedure to tell us about it.
What Is Radiofrequency Ablation?
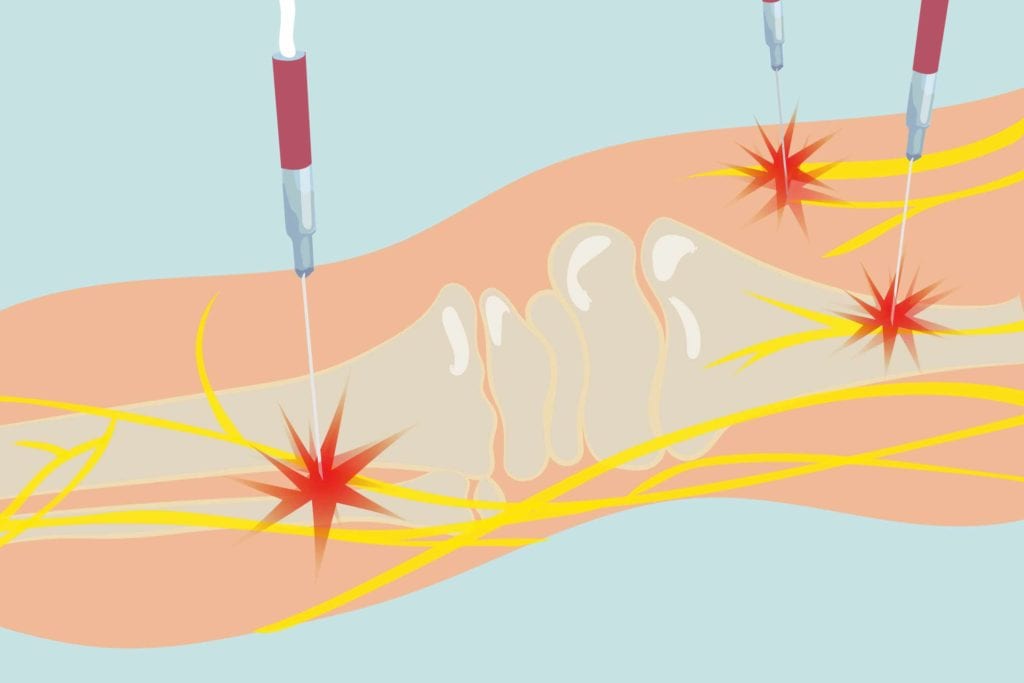
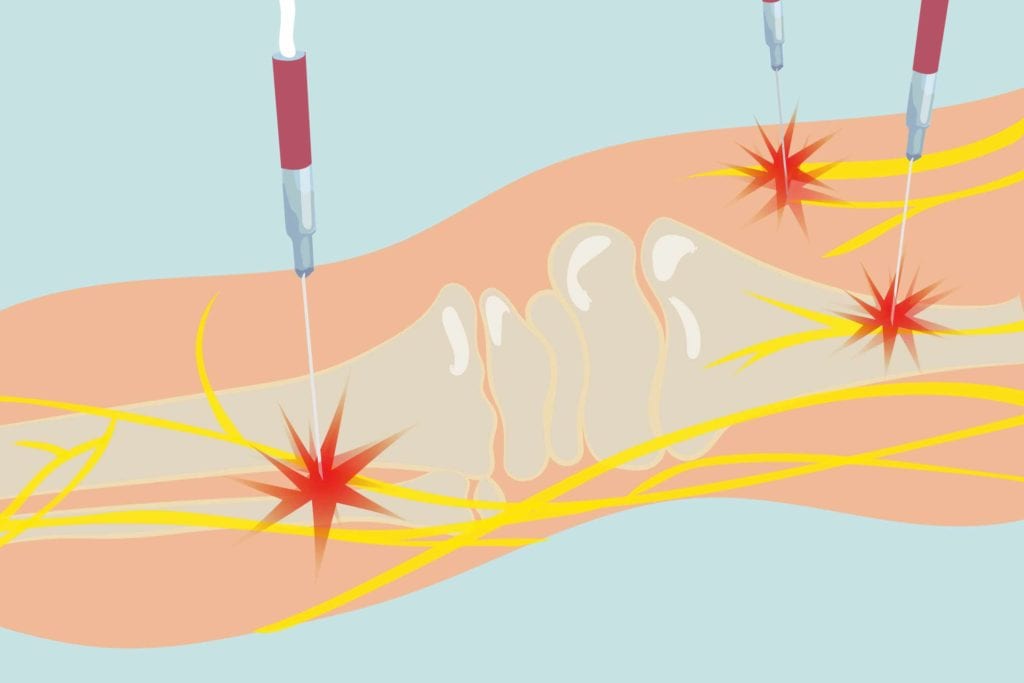
“Radiofrequency ablation or lesioning (RFA) is a non-surgical and minimally invasive procedure that uses heat to ablate or damage pain-transmitting nerve fibers,” says Sameer Kapasi, MD, a physiatrist at Tufts Medical Center in Boston. “The RFA reduces or permanently decreases the transmission of painful information to the brain from the knee.”
These radiofrequency waves generate an electrical current that “burns” the nerve, rendering it ineffective. “A great parallel is the door sensor on your car — if the wire for that sensor is cut, the door and the car still work, but the car does not know whether the door is open or shut,” Dr. Kapasi says. Similarly, when the RFA is performed, the brain can’t tell that the knee is in pain, so you feel less pain.
Why Is Radiofrequency Ablation Used to Treat Arthritis Pain?
The procedure isn’t actually treating the arthritis joint damage itself, but rather the way the patient experiences the pain of arthritis joint pain.
“RFA is effective because it numbs the targeted joint by burning the nerves to the painful joint,” Alice Chen, MD, a physiatrist at the Hospital for Special Surgery in New York City. “The radiofrequency waves transmitted through the needle tip causes the nerve to be inactivated. The nerves can grow back, though, so the effects of the procedure will last approximately six months long.”
What Happens During a Radiofrequency Ablation Procedure?
Your doctor does a trial run with a numbing medication before the actual ablation is done to make sure they know exactly where the pain is coming from, and to confirm that a patient will get relief.
If that’s the case, for the real procedure, “small needles are inserted under intermittent X-ray guidance to the proper locations,” he says. “The area is thoroughly anesthetized or ‘numbed,’ and the temperature of these insulated needles is raised. Then, the needles are removed after 60 to 90 seconds of the elevated temperature.”
The procedure can be done at a doctor’s office or hospital; it just needs to equipped with a fluoroscope, which is an imaging that shows a continuous X-ray image on a monitor.
What Kinds of Arthritis Is Radiofrequency Ablation Best for?
“An RFA can be used to treat an arthritic condition in a large joint like the knee or a small joint like those in the spine,” Dr. Kapasi says. “The RFA has yielded wonderful results for knee osteoarthritis and is regularly used for spinal osteoarthritis.”
One 2018 study showed the procedure was more effective than steroid injections for OA knee pain. Although the study was not “blind” (in other words, the patients knew what they were being treated with), it still showed promise for the procedure on the knee.
The technique can also be used to help treat pain in inflammatory arthritis, such as rheumatoid arthritis, says Dr. Kapasi — as long as preliminary diagnostic blocks show relief.
Is Radiofrequency Ablation Painful?
“The RFA procedure can be mildly uncomfortable during the 90 seconds that the nerve is being denervated,” Dr. Chen says. Some physicians use light sedation, she says, but the patient has to be conscious so they can give feedback to the doctor.
Afterward, “there can be some initial discomfort after the procedure, and the physician may give a small dose of steroid medication to decrease local inflammation from the procedure,” Dr. Chen says. Dr. Kapasi says knee patients may have some soreness post-injection on the day of the procedure, and although unlikely, some transient knee numbness can occur later.
Are There Harmful Side Effects of Radiofrequency Ablation?
The most important thing to avoid adverse effects post-procedureis to go to a doctor who performs RFA regularly. “Care needs to be taken to isolate the nerve being targeted so that the correct nerve is targeted, and the nerve is completely denatured,” Dr. Chen says. “Inadequate ablation may result in increased pain or altered sensation.”
CreakyJoints has heard from patients who had bad reactions to the procedure. “I have been bedridden since the ablation,” Sally, who had the procedure last month, wrote on our website. “The pain is so severe and intense that I can’t even describe how awful it is.” An increase in pain is not a common side effect, so let your doctor know right away if you experience it.
When Do Doctors Recommend the Procedure?
“Doctors will recommend the RFA when a patient has failed more conservative management of arthritis, including physical therapy, NSAIDs, and knee injections of steroid or viscosupplementation,” Dr. Kapasi says. “Often, these patients are not candidates for large procedures with anesthesia, such as total knee replacements. Some patients may not want to go down the knee replacement route, but they have failed conservative management.”
RFA can also be used if knee replacement surgery itself hasn’t provided relief. For back pain, RFA is also used when first-line treatments haven’t worked.
How Does RFA Fit Into an OA Treatment Plan?
The pain relief of RFA can help OA patients further their physical recovery of the joint. For those with spinal arthritis, “once the patient has relief of symptoms, it is important that the patient increase the stability and strength of the back and abdominal musculature — the core muscles — so the joints have less stress on them and hopefully will slow or halt the further progression of the arthritis in the joint,” Dr. Chen says. Similarly, physical therapy and exercise can help strengthen and support the knee joints.
Is There Anyone Who Should Not Get Radiofrequency Ablation?
“The test injection block confirms whether the patient has pain at the given level localizing the area — if a patient doesn’t have significant relief with the temporary block, the RFA should not be performed because the level is not confirmed,” Dr. Chen says. In addition, “patients who have pacemakers may be excluded from having the procedure.”
Because X-rays are used, those who are pregnant also will not be able to undergo RFA; people who have infections or bleeding problems may also not be able to have RFA. Talk to your doctor about whether RFA is right for you.
What Is the Recovery from RFA Like?
Generally, RFA is well-tolerated and has a short recovery — you can usually resume normal activities in 24 hours. “After the procedure, it may take up to a week for the nerve to fully numb,” Dr. Chen says. “Most patients achieve relief after the first week and can resume physical therapy and a strengthening program.” For the knee, Dr. Kapasi says the RFA should take full effect by three to four weeks. And for many patients, RFA is effective in relieving their pain. “Yes, it helped!” arthritis patient Marguerite told us on Facebook.





