By the time you’re in your late twenties, you’ve reached “peak bone mass” — and it’s downhill from there. The rate at which you break down bone starts outpacing the rate at which you form new bone, and it will be that way for the rest of your life. If you started with a decent amount of bone and the breakdown process happens slowly, your skeleton will remain strong enough. But many people lose too much bone and end up with low bone mass (osteopenia) or full-blown osteoporosis. Women are especially at risk after estrogen levels drop at menopause.
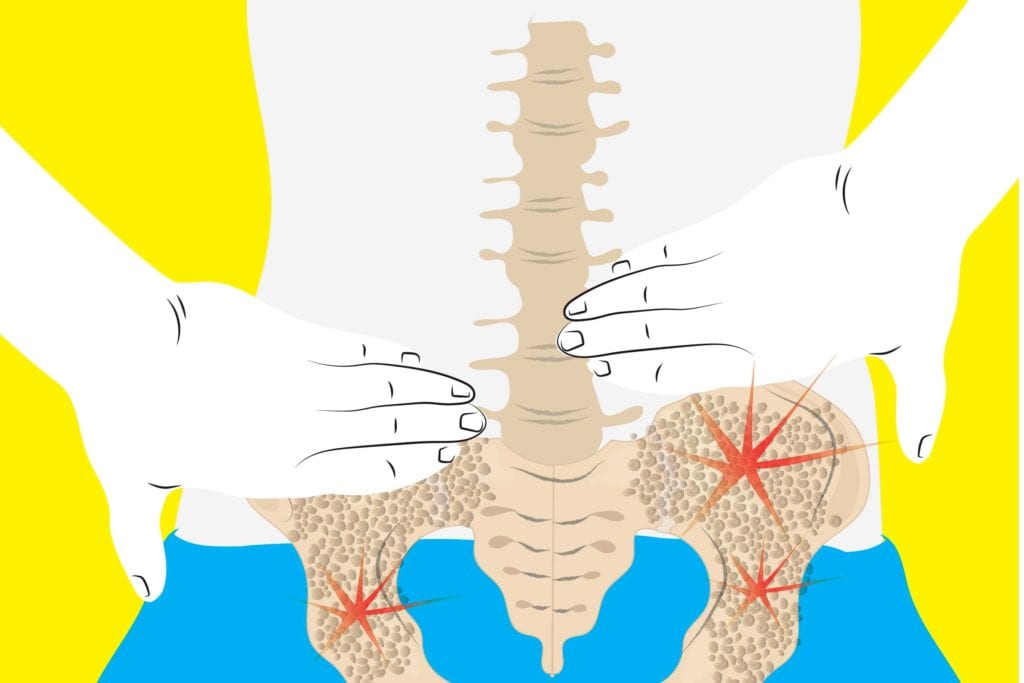
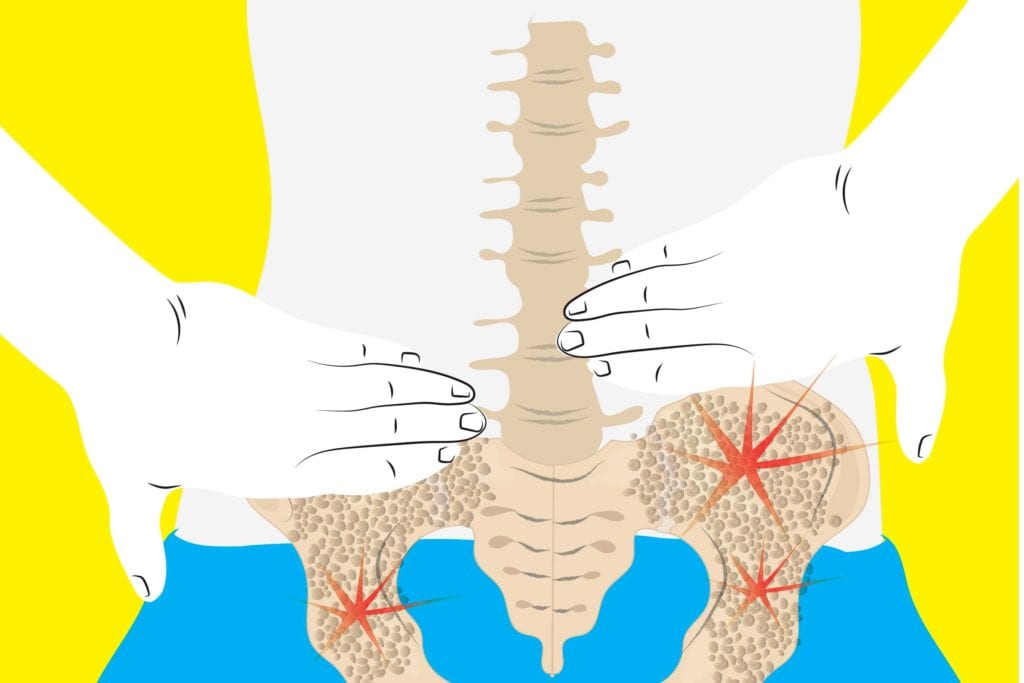
Osteoporosis is dangerous because it means your bones are extremely thin and brittle; even coughing or bending over could cause a fracture, and if you fall there’s a good chance you’ll end up breaking your hip, femur, or spine. To prevent that from happening, doctors most often put people with osteoporosis on bisphosphonate drugs (like Fosamax or Boniva), which are oral meds that slow the breakdown of bone. They help, but there’s a limit to what they can do.
In search of some better solutions, pharmaceutical manufacturers have been developing more aggressive therapies that actually build new bone as opposed to just slowing the rate of bone loss. These types of newer meds include Forteo (teriparatide), which was FDA-approved in 2002, and it took more than a decade for Tymlos (abaloparatide) to follow (FDA-approved in 2017). Now a newly approved option, Evenity (romosozumab-aqqg) joins their ranks.
While Forteo and Tymlos contain synthetic parathyroid hormone, Evenity works differently. It’s a “monoclonal antibody that blocks the effects of the protein sclerostin and works mainly by increasing new bone formation,” according to the FDA.
One thing that these drugs have in common, aside from increasing bone, is that they all carry a “black box” warning — the strictest type of warning that the FDA can issue.
The black box warning on Forteo and Thymos highlights the possible risk of bone cancer, a problem that was detected when the drug was tested in rats. Evenity carries a warning that it may increase the risk of heart attack, stroke, and cardiovascular-related death.
Evenity “should not be used in patients who have had a heart attack or stroke within the previous year,” the FDA warns. “Health care professionals should also consider whether the benefits of Evenity outweigh its risks in those with other risk factors for heart disease and should discontinue Evenity in any patient who experiences a heart attack or stroke during treatment.”
Although that sounds scary, Evenity also has also been shown to have some impressive benefits. In two clinical trials that included more than 11,000 women, those who used Evenity for a year lowered their risk of a new vertebral fracture by 73 percent (versus placebo).
Whether or not the benefits outweigh the risks for you is a matter to discuss with your doctor, who should factor in the severity of your osteoporosis as well as any other health issues (including cardiovascular ones) that you may have. If do decide to try Evenity, you’ll need to see a doctor once a month for a year; at each visit you’ll receive two back-to-back injections of this medication. After the year is up (the drug shouldn’t be used for more than 12 months) your doctor might opt to switch you to another type of osteoporosis medication.
Keep Reading
- Can Probiotics Help Protect Bone Health?
- Even Very Young Women with Rheumatoid Arthritis May Be at Risk for Bone Thinning and Fractures
- What the Mediterranean Diet Can Do for Your Bone Health





