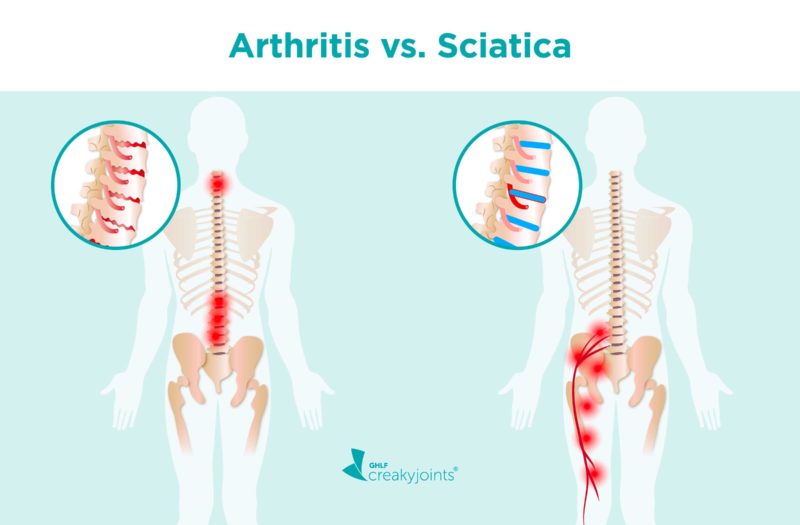
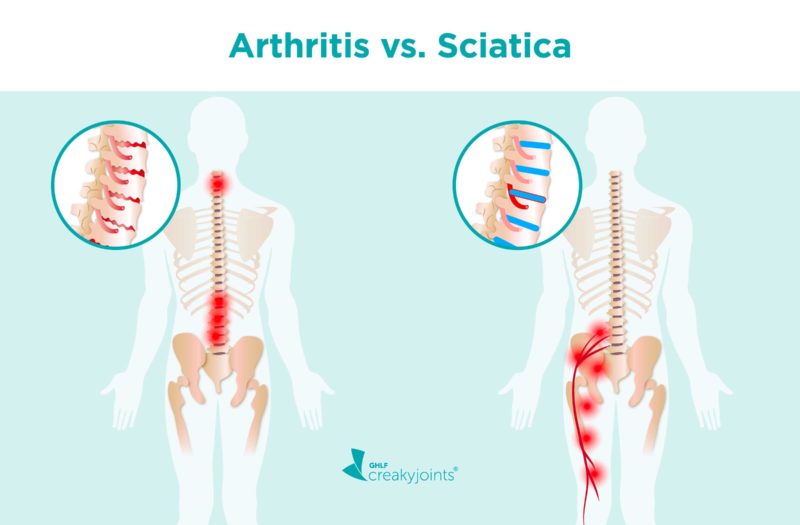
You might be helping a friend move some furniture or just sitting at your desk when it suddenly hits you: a sharp, burning pain that radiates through your lower back and buttocks and down the back of your leg. The most likely culprit is sciatica, which is a painful irritation of the sciatic nerve. But there is a chance arthritis could also be causing your pain. If you’re looking into the differences between arthritis and sciatica, you should know that these problems are not synonymous, though they do sometimes overlap.
Arthritis, in short, is inflammation of one or more joints. There are two general types: The “wear-and-tear” type, known as osteoarthritis (OA), and the inflammatory type, which includes rheumatoid arthritis (RA), axial spondyloarthritis (axSpa), and psoriatic arthritis (PsA), among others. This type of arthritis occurs when a person’s immune system attacks itself, resulting in joint inflammation.
Sciatica, however, is a pain that occurs when something irritates or presses on the sciatic nerve. The most common cause of sciatica is a herniated disk (aka a slipped disk), but arthritis can sometimes cause it, too.
If you’re not sure whether your back pain is from arthritis or sciatica, one way to start is by using online tools like PainSpot, which can help determine what might be causing your pain by asking a series of questions that helps differentiate types of pain from each other.
You may also want to consider the nature/symptoms of the type of pain you’re experiencing. Sciatica is a sharp pain that starts in the sciatic nerve, which runs from your lower back through your hip, thigh, and leg. Arthritis pain, on the other hand, makes your joints feel achy and stiff. It also isn’t limited to your lower body, so if you’re also experiencing pain and stiffness in other places — such as the neck, shoulders, ribcage, or hands — that may be something to consider.
You should see a doctor to receive a proper diagnosis and treatment plan. But it doesn’t hurt to do a little research before your appointment. Read on to learn more about the differences between arthritis and sciatica.
Arthritis vs. Sciatica
If you suspect you might be dealing with arthritis or sciatica, you can learn more about the symptoms of each, the key differences, the treatments, the outlook, and the risk factors.
Understanding Sciatica
Unlike arthritis, sciatica is not a disease but simply a description of pain stemming from the sciatic nerve. “The medical term [for sciatica] is lumbar radiculopathy, and it often happens when the S1 nerve root in the low back gets pinched,” says Dena Barsoum, MD, a physical medicine and rehabilitation physician with the Hospital for Special Surgery in New York City.
People experience sciatica differently, but the sensation usually starts in the lower back and travels down the back of the leg. Many patients report pain, tingling, numbness, and heaviness; some say it feels like an electric shock. Doctors describe sciatica as a type of “referred pain,” which means you sense it in parts of your body other than the one that’s directly impacted. (The pinched or irritated nerve is in your lower back, but you also feel pain or numbness in your buttocks and leg.)
But what’s actually pinching the nerve?
Oftentimes a slipped disc is to blame, and it can happen to anyone. The vertebrae (bones) in your spine are cushioned by disks that are made of a jelly-like substance contained in a tough shell. If you twist or move your body the wrong way, one of those disks could rupture. If you rupture a disk in your lower back and the misalignment puts pressure on the sciatic nerve, you’ll develop sciatica. This type of sciatica usually comes on suddenly.
Sometimes the root cause of sciatica is very simple. A classic example, says rheumatologist Joseph E. Huffstutter, MD, a partner with Arthritis Associates in Hixson, Tennessee, occurs in men who keep an overstuffed wallet in a back pocket. That placement makes them sit awkwardly and can put excessive pressure on the sciatic nerve. “If they start keeping their wallet in their front pocket or switch to a smaller wallet that usually takes care of it,” he says.
Understanding Arthritis in the Spine
In contrast, spinal osteoarthritis (the most common form of spinal arthritis) is often the result of cartilage between the joints slowly breaking down over time due to overuse. It can also occur when the discs between the vertebrae become thinner, leading to more damage, pressure, and friction on the joint cartilage. Spinal osteoarthritis usually causes pain and stiffness in the back itself and does not radiate through the leg. Some inflammatory forms of arthritis, such as axial spondyloarthritis and psoriatic arthritis, may also impact the spine by attacking the lining of the spinal joints.
Axial spondyloarthritis (axSpA) also causes joint inflammation — specifically inflammation of the sacroiliac (SI) joints that connect the bottom of your spine to the top of your pelvis. People with axSpA commonly report lower back pain as well as pain in the hips and buttocks. While sciatica usually causes pain in only one side of the buttocks, people with axSpA may find that the pain switches sides — sometimes referred to as “alternating buttock pain.”
Do You Have Arthritis or Sciatica?
Arthritis and sciatica can both present as back pain, but there are distinct symptoms associated with each. Determining which set of symptoms you’re experiencing may give you a better idea of which ailment you’re dealing with, though of course, you’ll need to consult a doctor to get an official diagnosis.
The type of pain you feel is likely a clue as to what condition you’re dealing with. Arthritis pain tends to be duller and makes you feel stiff. Pain from sciatica is often a sharp, shooting type.
Arthritis Symptoms
The pain caused by arthritis will likely vary depending on the type. Some shared symptoms of inflammatory arthritis include:
- Joint pain, stiffness, and swelling that is felt on both sides of the body
- Joints that are visibly swollen and warm to the touch
- Joint pain that worsens after inactivity
- Fatigue / lack of energy
- Malaise
You can find specific symptoms for rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and gout here.
Osteoarthritis symptoms include:
- Joint pain, stiffness, and swelling that is felt on one side of the body
- Joint pain that worsens after use
- Bone spurs
- Loss of flexibility
- Grating sensation from bone rubbing on bone
Sciatica Symptoms
Sciatica symptoms include:
- Sharp, burning pain that radiates from your lower spine down through your buttocks and the back of your leg, usually only on one side.
- Pain that is more felt in your lower leg compared to your lower back
- Pain that worsens when you cough or sneeze
- Pain that gets worse as the day goes on
- Numbness, tingling, or muscle weakness in the affected leg
- Difficulty controlling your bowels or bladder (if this is the case, you should seek immediate medical care)
Does Arthritis Cause Sciatica — or Vice Versa?
In some instances, arthritis can cause sciatica. If you have osteoarthritis in your spine, for example, the cartilage in that area degenerates over time. As that happens the sciatic nerve can become irritated. Many older adults with OA also develop bone spurs, tiny, jagged edges of bone that can press on the sciatic nerve.
How Common is Sciatica?
Sciatica is extremely common: According to the Cleveland Clinic, around two in five U.S. adults experience sciatica at some point in their lifetime. Some people, however, are more at risk of experiencing sciatic pain because of their lifestyle and other health conditions.
Outlook for Sciatica
Although sciatica can cause intense pain, it rarely requires serious medical intervention. According to Medical News Today, most sciatic pain lasts four to six weeks. That said, sciatica can cause permanent nerve damage if left untreated, so it doesn’t hurt to see a doctor if you are experiencing sciatic symptoms.
In rare cases, sciatica can lead to cauda equina syndrome, a condition that occurs when there is dysfunction of the collection of nerves at the end of the spinal cord (known as the cauda equina). This condition can lead to loss of bladder or bowel control, which requires immediate medical attention and surgery.
Risk Factors for Sciatica
Although anyone can get sciatica, some people are at higher risk than others. Some medical conditions and lifestyle habits that increase your risk for developing sciatica include:
- Age: People who are middle age or older are at an increased risk because, as you age, you’re more apt to have a slipped disk or develop OA in your spine.
- Weight: People who are overweight can be at risk because the excess pounds put extra pressure on your spine.
- Sedentary lifestyle: Sitting for long periods can irritate the sciatic nerve.
- Job: Many believe that a labor-intensive job that requires you to twist your back or carry heavy loads might increase your risk for sciatica. That said, there isn’t conclusive evidence of this link.
- Diabetes: This disease increases your risk of nerve damage, which can make it more likely for you to have sciatica.
- Previous injury: Having a slipped disk in your back can cause pressure on the sciatic nerve. Similarly, other back injuries can cause you to develop sciatica.
- Osteoarthritis: As mentioned earlier, as osteoarthritis breaks down the cartilage that cushions your bones, your body can grow bone spurs to try and repair the loss. It’s possible for these bone spurs to form in your spine and press on your sciatic nerve.
- Weak core: Having well-developed back and core muscles helps support the spine, which in turn decreases your risk for sciatica.
How Sciatica Is Diagnosed
If you think you have sciatica, and it’s severe or not improving, it’s important to see a health care provider. They will likely start by taking your medical history and then “do an extensive [manual] neurological exam so they can assess strength, sensation, and reflexes, and try to understand which nerve or nerves might be pinched,” says Dr. Barsoum. This likely includes:
- Walking: They will likely keep an eye on your gait as well as your posture, as walking with a hunched or flat back can put added stress on your lower back, leading to sciatica. They may also ask you to walk on your toes or heels to see if the pain worsens, another indicator of sciatica.
- Straight Leg Test: Your doctor will ask you to lie with one leg down, while the other leg is kept straight up and raised by the examiner. If raising the leg between 30 and 70 degrees causes pain to occur and radiate down the leg, that can indicate that you may have sciatica.
If a clear diagnosis can’t be made or a patient thought to have sciatica isn’t responding to treatment, your health care provider may order tests, which can include:
- Spinal X-rays: Your doctor may order X-rays to see if there are bone spurs that are pressing on a nerve.
- MRI: Similarly, your doctor may request an MRI to get a detailed image of your bone and soft tissues, which can allow them to see things like herniated disks.
- Electromyography (EMG): This test can confirm nerve compression caused by things like herniated disks by measuring electrical impulses produced by the nerves and responses of your muscles.
- CT Myelogram: This test involves a dye being injected into your spinal canal through your lower back. It allows for the doctor to get a clear look at whether there is anything pressing against your nerves or spinal cord.
How Sciatica Is Treated
At-home treatment for sciatica consists of over-the-counter anti-inflammatories, icing and/or applying heat to the afflicted area, and some patience. For many people, that is enough to help them heal within a few weeks.
If your pain is bad enough that you’ve sought professional help, however, you likely need extra help. Treatment options for sciatica include:
Physical therapy
This is the most common — and generally most effective — treatment for sciatica, says Dr. Huffstutter. The main goal is to take pressure off the sciatic nerve by strengthening and stretching the surrounding muscles. “Physical therapy can be invaluable; it’s really hard to learn how to do the right exercise without it,” he says.
Epidural steroid injections
“Physical therapy is very helpful, but sometimes the pain is too severe, and the patient feels they can’t do it,” says Dr. Barsoum. In that case, the first step might be to inject inflammation-reducing medication directly into the epidural space that surrounds the nerves in the spine.
Oral medication
Your doctor might suggest using anti-inflammatories, muscle relaxants, or even a narcotic medication if the pain is very severe. These drugs can make you feel a lot better and give your body a chance to heal.
Surgery
Though it is not common, if you have a herniated disk that hasn’t healed on its own (as it usually does) or you have a loss of control of urine or stool, then surgery might be in order. “More often than not, a patient can get completely better without surgery,” says Dr. Barsoum.
Track Your Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Sign up here.
Camino GO, et al. Straight Leg Raise Test. StatPearls. July 31, 2021. https://www.ncbi.nlm.nih.gov/books/NBK539717.
Herniated Disc. American Association of Neurological Surgeons. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Herniated-Disc.
Interview with Dena Barsoum, MD, physical medicine and rehabilitation physician with the Hospital for Special Surgery in New York City
Interview with Joseph E. Huffstutter, MD, rheumatologist with Arthritis Associates in Hixson, Tennessee
Klein J. How long does sciatica last for? Medical News Today. October 23, 2020. https://www.medicalnewstoday.com/articles/how-long-does-sciatica-last#how-long-does-the-pain-last.
Sciatica. Cleveland Clinic. March 25, 2020. https://my.clevelandclinic.org/health/diseases/12792-sciatica.
Sciatica. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/sciatica.
Sciatica. Mayo Clinic. August 1, 2020. https://www.mayoclinic.org/diseases-conditions/sciatica/symptoms-causes/syc-20377435.
Sciatica home remedies and self-care. Harvard Health Publishing. April 21, 2020. https://www.health.harvard.edu/pain/sciatica-home-remedies-and-self-care.
Spinal Arthritis (Arthritis in the Back or Neck). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/spinal-arthritis.
Wiseman D. Cauda Equina Syndrome. American Association of Neurological Surgeons. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Cauda-Equina-Syndrome.
Yu DT, et al. Patient education: Axial spondyloarthritis, including ankylosing spondylitis (Beyond the Basics). UpToDate. January 7, 2020. https://www.uptodate.com/contents/axial-spondyloarthritis-including-ankylosing-spondylitis-beyond-the-basics/print.





