If you have arthritis, either inflammatory arthritis or osteoarthritis — or related conditions like fibromyalgia — you’ve probably been dealing with chronic pain. Pain has two parts: the physical and the psychological. The medications you take help pain symptoms by addressing your physical needs, but what if there was a way to also help reduce your pain through psychology?
If you just read that and thought, “That sounds great, except I’m sure it won’t work for me — my pain is too great and I’ll never be able to feel better,” then you’ve just displayed the type of negative thought patterns that cognitive behavioral therapy (CBT) aims to change.
What Is Cognitive Behavioral Therapy?
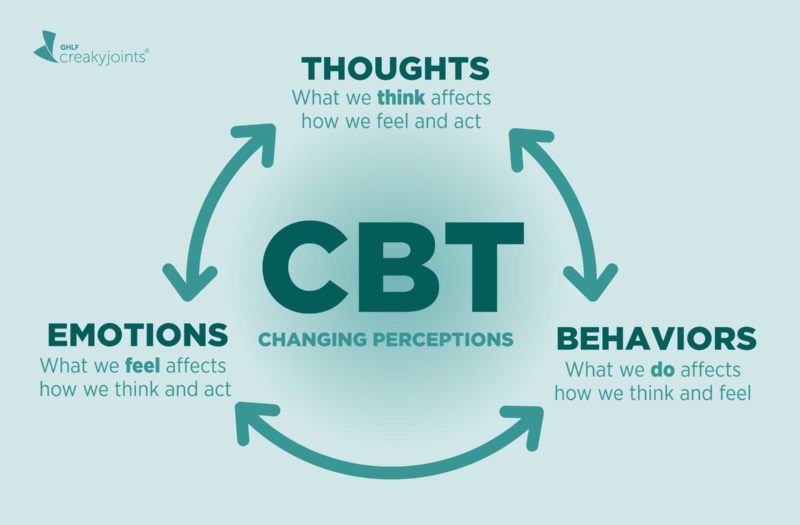
First developed in the 1960s and 1970s, CBT is rooted in the idea that the way you perceive situations influences the way you feel, and that you have the ability to change your thought patterns to feel better. It is one kind of many different treatment methods and techniques used in psychotherapy.
“Cognitive behavioral therapy is at present the most widely used psychotherapeutic treatment for adults with chronic pain,” says Shilagh A. Mirgain, PhD, a psychologist in the department of Orthopedics and Rehabilitation at the University of Wisconsin Research Park Clinic in Madison, Wisconsin. “CBT involves examining both what you think — cognitions — and what you do — behaviors — about pain. It is a systematic and structured way of identifying which behaviors and thoughts are helpful and which are unhelpful.”
CBT isn’t a single technique, but rather an approach to psychotherapy that involves helping patients view their pain differently in order to have a better quality of life. It also might not be the only approach a therapist uses during your sessions. A combination of techniques individualized to each patient may be part of your overall therapy treatment.
CreakyJoints member Mary G. says she saw a therapist in the years after her diagnosis, which was more than 30 years ago, and she still uses some of the skills today. “She specialized in chronic illness and was immensely helpful,” Mary shared on Facebook. “I think we did mostly CBT. The most important thing I learned was to accept my new life and stop mourning the one that was gone.”
For most patients, CBT or other therapy approaches aren’t meant to take the place of medication but complement it as part of an overall treatment plan that aims to help people with chronic pain feel better physically and mentally.
How Does CBT Work?
The mind-body approach of CBT isn’t just about talking on a psychologist’s couch; it’s about taking action to ultimately change your thinking and behavior.
“CBT is different from talk therapy in that the primary goal is to provide patients with strategies and skills to learn to self-manage their problems,” says Tamara J. Somers, PhD, an associate professor in the Department of Psychiatry and Behavioral Sciences at Duke University Medical Center in Durham, North Carolina. “The goal of CBT for arthritis pain is to increase patients’ self-efficacy for pain management — that is, their confidence — to manage their pain and decrease pain interference with their daily life.”
CBT does this by teaching skills to increase helpful coping thoughts and behaviors to deal more effectively with daily pain symptoms and improve overall functioning and quality of life, Dr. Mirgain says.
“It helps me get out of my negative thoughts and move forward,” Eileen D. told us on Facebook. “It also helps me understand what I am going through better.”
A typical session may entail first assessing the areas of difficulty in your life affected by chronic pain, and how you deal with it. Do you not want to leave the house for fear of pain? Do you ruminate with negative thoughts about your pain that go around and around in your head? Do you believe your negative thoughts are truths that can’t be changed? Then the therapist can work with you to develop strategies to practice at home to stop yourself from entering that vicious thought cycle or to get out of your comfort zone little by little to become more active. The goal of CBT is to learn to change your thoughts in order to change your behavior.
And you’re not locked in for years and years with CBT. This kind of therapy is generally designed to be a few months of weekly hour-long sessions to give you action-based tools you can use on your own for years to come. “Ranging typically from eight to 12 structured sessions, CBT is considered a short-term treatment that promotes active coping strategies,” Dr. Mirgain says.
CBT and Arthritis: How It May Help
CBT has been studied for arthritis pain for many years and is considered the “gold standard” for psychological treatment of chronic pain. “There are several well-designed studies that have shown that CBT can be effective for patients with arthritis,” says Liana Fraenkel, MD, MPH, a rheumatologist and adjunct professor at Yale School of Medicine in New Haven, Connecticut.
“It compares to other non-pharmacologic approaches such as exercise.”
One meta-review from Boston University found that CBT treatments consistently led to improvement in chronic pain. Another analysis found that CBT was more effective in pain reduction for fibromyalgia than other psychological treatments. Another found CBT was the most effective psychotherapy for rheumatoid arthritis.
“There is a lot of empirical evidence to suggest that CBT can be helpful for both osteoarthritis and rheumatoid arthritis pain,” Dr. Somers says. “There is also evidence that CBT applied to these conditions can improve pain self-management ability, physical disability, distress and other pain-related outcomes.”
Dr. Fraenkel notes that in addition to helping with chronic pain, CBT is also proven to help conditions that tend to co-occur with pain, such as insomnia, anxiety, and depression.
Some of the particular benefits of CBT include:
Coping with pain
“CBT involves skills that are scientifically proven to be helpful in managing pain,” Dr. Mirgain says. “These skills involve changing the way you respond to pain, both in terms of your thoughts and feelings. It involves learning self-management skills such as goal-setting, relaxation training, activity pacing, coping thoughts, improving social support, distraction, challenging negative thoughts, challenging negative pain beliefs, sleep tips, increasing positive activities, and assertiveness.”
In Dr. Fraenkel’s recent study presented at the ACR/ARP Annual Meeting, she found that CBT was a comparable treatment to a prescription NSAID (non-steroidal anti-inflammatory drug). CBT also lacks the risk of side effects associated with pain meds.
Reducing depression and other conditions that go along with pain
CBT also has been studied for treating depression, which often comes with chronic pain. “CBT is also very helpful in addressing commonly co-occurring conditions such as anxiety and depression as well as insomnia, which all worsen the experience of pain,” Dr. Fraenkel says. “It is also very helpful for patients who have anxiety and stress.”
Managing fatigue
Recent research has also found some evidence for managing fatigue as well, which makes sense as CBT also helps energy-sucking conditions like insomnia and depression. Improving fatigue can help you get back to your normal life. “CBT focuses on helping people with arthritis pain get more active and do more of the things they enjoy or want to do but have reduced or stopped because of pain, and improve physical and social activity,” Dr. Mirgain says.
Increasing function
By changing negative thought patterns, CBT helps arthritis patients stop “catastrophizing” their pain, which makes you feel helpless or out of control. This leads to better function in daily life. Although it doesn’t stop the pain, it stops the response to pain — kind of like teaching you to be more optimistic about your condition.
“Patients with a more positive attitude toward life appear to be able to cope better and have less distress, avoidance, and disability with a pain condition than those who tend to take a more negative view,” Dr. Mirgain says.
Boost self-management of your disease
Overall, the goal of CBT is to give you skills to take back power over your disease. “CBT helps foster a sense of control over pain and encourages the development and strengthening of self-management skills,” Dr. Mirgain says. Ultimately, CBT isn’t just about therapy sessions; it’s giving you tools to use at home.
What Does CBT Entail?
“Patients may be taught a variety of skills and strategies to help manage their pain, such as progressive muscle relaxation, imagery, activity pacing strategies, pleasant activity planning, examination of pain-related thoughts, and goal setting,” Dr. Somers says.
Here are a couple of examples:
Progressive muscle relaxation
“In a session, this can include breathing exercises that teach a patient to tense certain muscle groups throughout the body, such as the stomach and calves, notice the tension, and then relax that muscle group,” Dr. Somers says. “The patient is then asked to practice progressive muscle relaxation daily with one goal being to learn to notice tension quickly and be able to relax quickly as they go through their days.”
Activity-rest cycle
“The activity-rest cycle is a type of pacing where patients identify an activity that they tend to overdo that leads to pain, such as cooking or lawn work, and then set a pre-specified time they will do the activity before they would expect to have pain, maybe 15 minutes,” Dr. Somers says. Then, once they reach their time limit, they rest for a specified period of time, such as five minutes.
“The patient is asked to repeat this cycle when doing the activity with the goal of decreasing the likelihood of pain due to overdoing it; and also being able to complete an activity or get more done by purposefully alternating between activity and rest,” Dr. Somers says.
Read more here about strategies for energy pacing.
Learning to be mindful of thoughts, and then change them
Patients work on recognizing what thoughts they’re having that are unhelpful and even unrealistic. So, if you think, “I’ll never not be in pain and my life sucks,” CBT encourages you to catch yourself doing it, stop yourself, and reframe your thinking to something more like, “I’m having pain now but yesterday I really enjoyed myself at with my grandkids at the park. I sometimes have pain, but I do enjoy my life.”
In this way, patients can identify and change negative, unhelpful thought patterns that have a negative influence on behavior. “People learn to create more adaptive thinking patterns and active coping behaviors,” Dr. Mirgain says.
How Is CBT Different from Other Kinds of Therapy?
Unlike therapy styles that focus more on why you feel a certain way or dig deep into your past, CBT tends to stick to your current thoughts with an aim to change them to be more productive, positive, and realistic.
CBT doesn’t look to explore your childhood traumas through years of in-depth psychoanalysis. Rather, CBT looks to provide patients with more immediate solutions to problems with their thoughts and behavior. For example, a therapist performing psychoanalysis might ask you about your home life, your family growing up, or issues with your parents to discover root causes of depression. You might talk freely about whatever you feel like during a session.
But CBT is more targeted and action-based, so a therapist may ask you what specific thoughts precipitate your feeling depressed or anxious, and then help you to redirect your thinking from a new angle. And therapy doesn’t just take place on the therapist’s couch. You’ll practice these strategies at home, too, and then report back to your therapist how they worked.
Depending on your goals for therapy, CBT might not be for everyone. If you want to explore the roots of your problems and feelings then CBT might not be for you. Some professionals have criticized CBT as being too superficial in treating the symptoms but not the underlying cause of an issue.
However, when you’re dealing with a specific problem like chronic pain, CBT may be a good choice that can help alleviate issues relatively quickly; yet there are no guarantees that the strategies will work for you.
CBT vs. Acceptance and Commitment Therapy
Some CreakyJoints members shared that they have benefitted from a variation on traditional CBT known as acceptance and commitment therapy (ACT). According to Psychology Today, ACT aims to teach people “to stop avoiding, denying, and struggling with their inner emotions and, instead, accept that these deeper feelings are appropriate responses to certain situations that should not prevent them from moving forward in their lives.”
As CreakyJoints member Sian C., a health psychologist, says, “I think it is one of the best types of interventions to help people with chronic illnesses. The premise is not to change or challenge thoughts — as is classic CBT — but learn to change your relationship with them. Learning about acceptance doesn’t mean approval of your struggles but being with your reality so you can act towards living a meaningful life.”
CreakyJoints member Cheryl C. shared on Facebook that CBT helped her to a point, but that ACT, which she describes as a mindfulness-based approach, has helped more. “For me CBT was limited because I knew some of my anxious thoughts were distortions and it felt like CBT tried to get me to ‘think my way out of them,’ which didn’t work,” she says. “Acceptance-based therapy helped me ‘de-fuse’ or detach from my thoughts rather than argue with them. In CBT it was about replacing distorted thoughts with ‘correct’ thoughts. In ACT, it was about recognizing my thoughts as just … thoughts, regardless of whether they’re right or wrong, and learning to live with them.”
For more information about ACT, CreakyJoints members recommend reading the book The Happiness Trap by Russ Harris.
How to Find a CBT Therapist
Therapists who practice CBT may be psychologists, social workers, counselors, or psychiatrists. You can start by asking your rheumatologist or primary care doctor for a recommendation. Local hospitals may offer pain management support groups that utilize CBT techniques.
You can search online for therapists who specialize in CBT techniques via tools at the Association for Behavioral and Cognitive Therapies, the National Association of Cognitive-Behavioral Therapists, PsychologyToday, or GoodTherapy.
Finding a nearby therapist, though, can be challenging. “Tried to find CBT near me and nothing,” Robin K. told us on Facebook. “There needs to be more help out there.” If you find a therapist who’s far away, you may be able to use CBT over the phone or through video conferencing. You can also consider trying telemedicine apps that specialize in mental health, such as TalkSpace or BetterHelp.
If you’re not sure whether a therapist is trained in CBT, ask them, says Dr. Somers. “Many PhD-level psychologists have been trained to do CBT for pain and symptom management as have many masters-level clinicians,” she says.
Although CBT might not be right for everyone, it has been shown to be an effective therapy that might be worth trying. With chronic pain, your psychological health is as important as your physical health.
Track Your Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Learn more and sign up here.
Keep Reading
Backman CL. Arthritis and pain. Psychosocial aspects in the management of arthritis pain. Arthritis Research & Therapy. December 2006. doi: https://doi.org/10.1186/ar2083.
Bruce B, et al. Intensive CBT Is Effective in the Treatment of Significant Functional Impairment and Psychological Distress Found in Fibromyalgia: But Can We Improve Depressive Symptoms? [abstract]. Arthritis & Rheumatology. 2019. https://acrabstracts.org/abstract/intensive-cbt-is-effective-in-the-treatment-of-significant-functional-impairment-and-psychological-distress-found-in-fibromyalgia-but-can-we-improve-depressive-symptoms.
Ehde DM, et al. Cognitive-Behavioral Therapy for Individuals With Chronic Pain. American Psychologist. February-March 2014. doi: http://dx.doi.org/10.1037/a0035747.
Fraenkel L, et al. Stopping NSAIDs for Arthritis Pain (SNAP): A Randomized Withdrawal Trial Comparing NSAIDs to Cognitive Behavioral Therapy [abstract]. Arthritis & Rheumatology. 2019. https://acrabstracts.org/abstract/stopping-nsaids-for-arthritis-pain-snap-a-randomized-withdrawal-trial-comparing-nsaids-to-cognitive-behavioral-therapy.
Glombiewski JA, et al. Psychological Treatments for Fibromyalgia: A Meta-Analysis. Pain. November 2010. doi: http://dx.doi.org/10.1016/j.pain.2010.06.011.
Hewlett S, et al. Reducing arthritis fatigue impact: two-year randomised controlled trial of cognitive behavioural approaches by rheumatology teams (RAFT). Annals of the Rheumatic Diseases. February 2019. doi: http://dx.doi.org/10.1136/annrheumdis-2018-214469.
History of Cognitive Behavior Therapy. Beck Cognitive Behavior Therapy. https://beckinstitute.org/about-beck/team/our-history/history-of-cognitive-therapy.
Hofman SG, et al. The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognitive Research & Therapy. July 2012. doi: https://doi.org/10.1007/s10608-012-9476-1.
Interview with Liana Fraenkel, MD, MPH, a rheumatologist and adjunct professor at Yale School of Medicine in New Haven, Connecticut
Interview with Shilagh A. Mirgain, PhD, a psychologist in the department of Orthopedics and Rehabilitation at the University of Wisconsin Research Park Clinic in Madison, Wisconsin
Interview with Tamara J. Somers, PhD, an associate professor in the Department of Psychiatry and Behavioral Sciences at Duke University Medical Center in Durham, North Carolina
Lumley MA, et al. The effects of written emotional disclosure and coping skills training in rheumatoid arthritis: A randomized clinical trial. Journal of Consulting & Clinical Psychology. August 2014. doi: https://doi.org/10.1037/a0036958.
Sharpe L. Psychosocial management of chronic pain in patients with rheumatoid arthritis: challenges and solutions. Journal of Pain Research. March 2016. doi: https://doi.org/10.2147/JPR.S83653.
Shedler J, et al. Where Is the Evidence for “Evidence-Based” Therapy? Psychiatric Clinics of North America. June 2018. doi: https://doi.org/10.1016/j.psc.2018.02.001.