Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
When the COVID-19 pandemic struck earlier this year, it disrupted everyday life for everyone. Schools shut down, grocery shopping felt risky, and our usual ways of working, socializing, and traveling came to a grinding halt.
Health care, too, changed overnight. One day it was normal to go to the doctor, get bloodwork done, and take your medications as prescribed; the next, well, maybe it wasn’t.
In the early days of the pandemic — and as it continues — people with rheumatic and musculoskeletal (RMD) conditions have had unique concerns and experiences due to their chronic diseases, the comorbidities that occur with them, the medications used to treat them (which often include immunosuppressive therapies), and the fact that they typically see health care specialists more regularly than the general population.
In order to understand the concerns and behaviors of people living with rheumatic and musculoskeletal disease (both autoimmune and non-autoimmune kinds) during the pandemic, the research team of the Global Healthy Living Foundation quickly sprang into action.
By the end of March 2020, we launched the Arthritis & Rheumatic Disease COVID-19 Project, a study for patients with all types of arthritis, to track the evolving impact of COVID-19 on people living with these conditions. (This study is actually part of a bigger group we created called the Autoimmune COVID-19 Project, in which we collaborate with research registries for people living with multiple sclerosis (MS), Crohn’s disease and ulcerative colitis, and vasculitis.)
In a series of research abstracts presented during ACR Convergence 2020, the annual meeting of the American College of Rheumatology, we have insights from more than 10,000 people with rheumatic diseases who participated in initial surveys (conducted between March 28 and May 26, 2020).
The findings reveal important insights about the concerns that rheumatic disease patients had about COVID-19, how their access to health care was disrupted, and the ways in which they responded to these disruptions, including behavior related to immunosuppressive medications.
Here are some key learnings from our research.
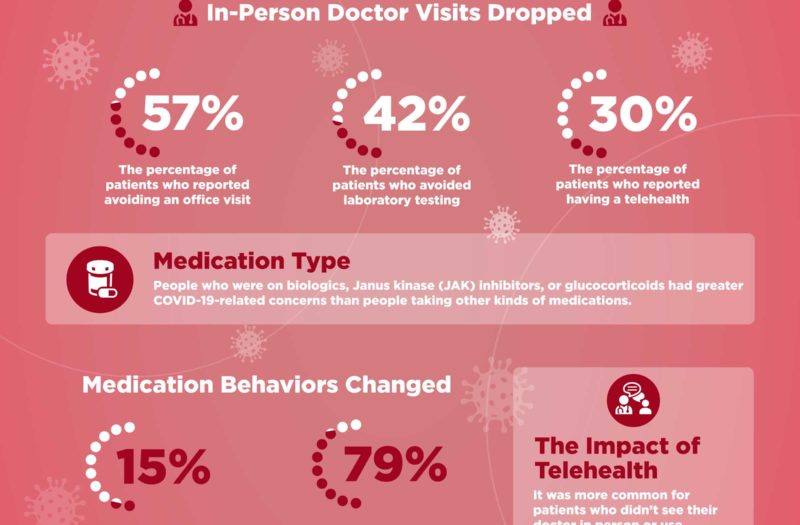
1. There was an immediate and substantial decrease in in-person health care
In one study, led by rheumatologist Michael George, MD, an assistant professor of medicine at the Hospital of the University of Pennsylvania along with a team of other researchers, survey responses from 1,517 patients across the U.S. with autoimmune rheumatic diseases from the ArthritisPower registry (diagnoses included rheumatoid arthritis, psoriatic arthritis, axial spondyloarthritis, and systemic lupus erythematosus) were analyzed. We found that:
- 57 percent of patients reported avoiding a doctor’s office visit
- 42 percent of patients avoided laboratory testing
- 30 percent of patients reported having a telehealth visit
2. But it was LESS common among patients with autoimmune disease to skip doctor’s visits and MORE common for them to have telehealth visits than people with non-autoimmune rheumatic and conditions
In a related study, researchers looked data from 9,004 patients who were part of a multi-state rheumatology provider network called American Arthritis and Rheumatology Associates (AARA).
They wanted to examine whether there were differences in people’s concerns and behaviors depending on whether they had an autoimmune condition (such as rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, or systemic lupus erythematosus) or a non-autoimmune rheumatic disease (such as osteoarthritis or osteoporosis).
They found that it was less common among patients with autoimmune disease to avoid a doctor’s visit or laboratory tests and more common for them to have had a telehealth visit compared to those with non-autoimmune disease.
A possible explanation is that autoimmune patients generally need to see their providers more often, so it may be more convenient for patients with conditions like osteoarthritis or osteoporosis (who may only go to the doctor once or twice a year) to delay a visit than it is for someone who is used to seeing the doctor every few weeks or months.
3. The type of medications that patients took were related to their concerns about COVID-19
Our data showed that people who were on biologics, Janus kinase (JAK) inhibitors, or glucocorticoids had greater COVID-19-related concerns than people taking other kinds of medications.
While there are still many unknowns, what research has generally shown so far is that higher doses of glucocorticoids have been linked with worse COVID-19 complications, but other disease-modifying drugs (DMARDs), including biologics and JAK inhibitors, have not.
In fact, many inflammation-fighting DMARDs are currently being studied as a treatment for COVID-19 complications.
“It is understandable that people would be concerned about their medication, but patients should not stop taking medication without discussing it with their doctor, since uncontrolled autoimmune disease might actually make you more susceptible to an infection like COVID-19,” says Dr. George.
Yet unfortunately …
4. Many patients stopped taking their medications without talking to their doctors
Data from both studies showed that patients stopped taking disease-modifying medication. In one study, 15 percent of patients — who did not have respiratory illness symptoms — reported stopping one of their DMARDs because of concerns about COVID-19.
Of these, 79 percent of therapy interruptions were not recommended by a doctor.
In the other study, among the 5,543 patients receiving a DMARD, 10 percent stopped a medication because of concerns about COVID-19.
At the very beginning of the pandemic, there was no clear direction about medication for patients. But within a few weeks, the American College of Rheumatology issued guidance that still stands today.
The main takeaway: People who are otherwise healthy (no COVID-19 symptoms or known exposure or no other infections) should not stop taking any of their rheumatic disease medications without consulting their doctor. It may be advisable to try to reduce the dosage of glucocorticoids with guidance from a clinician. For patients with a COVID-19 infection, doctors may suggest they take a break from certain medications while they are sick. Read more here about the guidance.
5. Telemedicine may have helped patients stick with their treatment
Interestingly, our research showed that it was more common for patients who avoided an office visit and reported that telehealth was not available to stop a DMARD than for those who were able to keep seeing their providers (either in person or virtually).
“Rheumatologists continue to play a critical role in answering patients’ questions about their medications during the pandemic,” says Dr. George. “This data seems to show that patients who were able to discuss their concerns with their doctors may have got the information they needed to follow treatment recommendations. We know that stopping disease-modifying medication can cause patients to have disease flares and may actually make them more susceptible to infection, so it’s important to always talk to your doctor about your treatment and not stop taking your medication on your own.”
6. Telemedicine usage had less to do with geography than you might think
You might think that patients in rural areas would use telehealth more than patients in urban areas, who likely live closer to their providers, but our data showed the opposite.
Patients in urban areas used telehealth more often during this study period than those in rural areas.
This may have to do with the distribution of COVID-19 “hot spots,” which were more concentrated in cities in the first few months of the pandemic and have since spread to more suburban and rural areas throughout the South, West, and Midwest. Compared to rural areas, there seemed to be more anxiety in urban areas about leaving home at all, including to go to their doctor’s office, so providers and patients interacted via telehealth instead.
7. Patients with and without autoimmune disease expressed similar concerns about COVID-19
Our study found that patients with and without autoimmune disease expressed similar concerns about COVID-19, as well as similar social distancing behaviors. For example, 49 percent of both groups said they had “extreme concern about COVID-19.”
Both groups avoided seeing family and friends (around 84 percent), avoided restaurants (around 94 percent), and avoided leaving the house (around 52 percent) at a similar frequency.
One notable difference, though, was that almost 40 percent of people with autoimmune conditions said that their health condition “extremely affected their concern” about COVID-19, compared to only 16 percent of people without autoimmune disease.
Non-autoimmune patients were older (average age 69) than those with autoimmune conditions (average age 58), so it’s possible that people with non-autoimmune rheumatic conditions were concerned about COVID because of their age or other comorbidities, but not necessarily because of their rheumatic condition (osteoarthritis or osteoporosis).
Found This Study Interesting? Get Involved
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
George M, et al. Concerns and Behaviors of Patients with Common Autoimmune Rheumatic Diseases in the United States Early in the COVID-19 Pandemic. [abstract]. Arthritis & Rheumatology. November 2020. https://acrabstracts.org/abstract/concerns-and-behaviors-of-patients-with-common-autoimmune-rheumatic-diseases-in-the-united-states-early-in-the-covid-19-pandemic.
George M, et al. Concerns and Health-Related Behaviors During the COVID-19 Pandemic in Patients with or Without Autoimmune Rheumatic Disease in a Large Physician Network. [abstract]. Arthritis & Rheumatology. November 2020. https://acrabstracts.org/abstract/concerns-and-health-related-behaviors-during-the-covid-19-pandemic-in-patients-with-or-without-autoimmune-rheumatic-disease-in-a-large-physician-network.