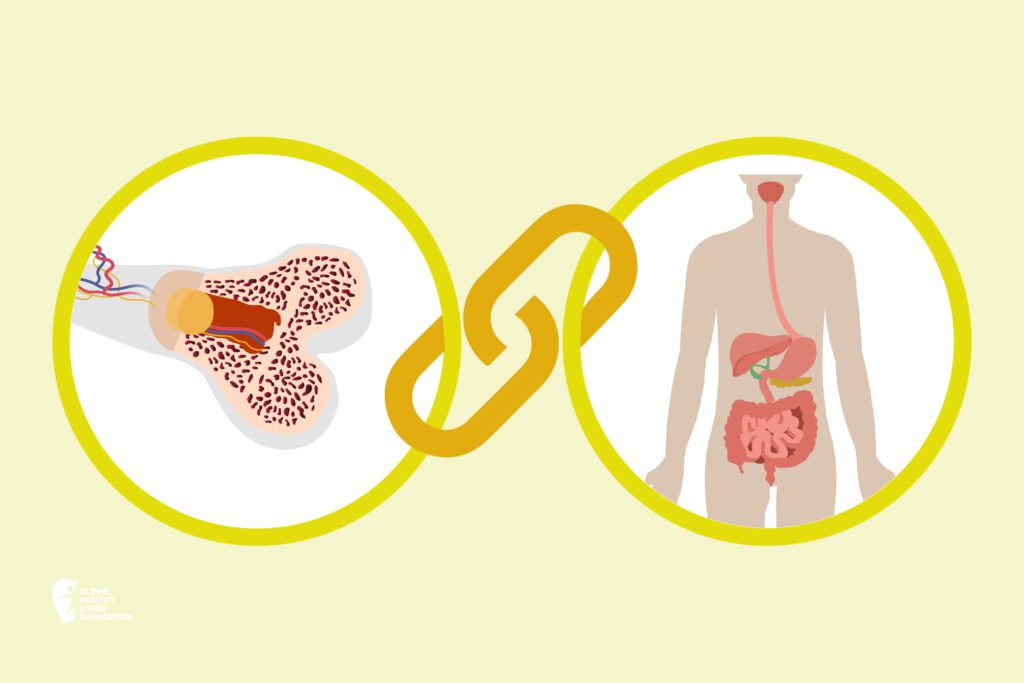
While inflammatory bowel disease (IBD) impacts your gastrointestinal (GI) tract, osteoporosis affects your bones. It causes bones to become weak, brittle, and break more easily. And it’s common: Osteoporosis is thought to affect more than 200 million people across the globe.
If you have IBD, bone health may not be top-of-mind — but it has been linked with osteoporosis. Here’s why you should also find ways to preserve your bone health.
The Link Between IBD and Osteoporosis
IBD in an umbrella term for chronic inflammatory conditions that affect your GI tract, such as Crohn’s disease and ulcerative colitis. It leads to a range of digestive symptoms that come and go, like abdominal pain and frequent bowel movements. And it’s common — IBD affects about 10 million people worldwide.
IBD also increases your risk of other health conditions — from migraine to heart disease to cancer. Research shows an association between IBD and bone loss, which can lead to osteoporosis and an increased risk of bone fracture. “Inflammatory bowel disease itself does not cause osteoporosis,” says Abhik Bhattacharya, MD, gastroenterologist and IBD specialist at The Susan and Leonard Feinstein IBD Center, Mount Sinai Health System in New York City. Instead, a few factors come into play.
IBD Medications
One of the most commonly used IBD treatments is prednisone, which is a very potent corticosteroid, says Bhattacharya. It acts very quickly and works to suppress the immune system, he adds.
But corticosteroids can also come with side effects like bone loss, particularly when used in high doses over time. According to the Crohn’s and Colitis Foundation, 30 to 50 percent of people who use corticosteroids long-term develop osteoporosis. Though that risk varies depending on the dosage and the length of corticosteroid use.
According to Bhattacharya, the largest risk comes from taking 20 or more milligrams (mg) of corticosteroids for a period of three months or more. “Over a lifetime of any patient, they can lead to a decrease in bone deposition,” he says. “This is synonymous with what we know as osteoporosis.”
What’s more, researchers have found that, even long-term use of lower doses (5 mg) of prednisone can lead to bone loss.
Underlying Inflammation
IBD is an inflammatory disease, meaning it involves inflammation in the GI tract. This inflammatory response can disrupt the natural pace at which old bone is removed and new bone is formed. And when IBD is active, it increases the risk to your bone health.
Research shows that taking anti-inflammatory medications to control IBD may help reduce negative effects of inflammation on bone health. However, studies show that when you combine anti-inflammatory medications with steroids, the steroids still pose a risk to your bone health.
Vitamin D Deficiency
Studies have found that IBD can lead to malabsorption, resulting in vitamin D deficiency. However, vitamin D helps your body absorb calcium—and both of these essential nutrients help promote strong, healthy bones.
Osteoporosis Risk Factors
“The other risk factors [for osteoporosis] would be whatever risk factors are present in general population,” says Bhattacharya. These can be broken into two groups: uncontrollable and controllable risk factors.
Uncontrollable risk factors for osteoporosis include:
- Gender: Osteoporosis is more common in women, especially in perimenopausal women.
- Ethnicity: Osteoporosis is more common in Caucasian and Asian women.
- Age: The older you get, the higher your risk of developing osteoporosis.
- Family history: If an immediate family member, like a parent, has osteoporosis, your risk of developing it increases.
Controllable risk factors, or those you can modify, include:
- Medications: Long-term use of steroids or anticonvulsants can contribute to osteoporosis.
- Diet: Low calcium and vitamin D intake may contribute to osteoporosis risk.
- Inactivity: Not exercising regularly, or being inactive, can weaken your bones.
- Weight: Being underweight (or having a small body frame) can impact bone health.
- Smoking: Smoking cigarettes makes you more prone to osteoporosis and bone fractures.
- Alcohol: Excessive alcohol consumption impacts how the body absorbs calcium and vitamin D, both of which are critical for healthy bone development.
By familiarizing yourself with the many risk factors tied to osteoporosis, you can have an informed conversation with your health care provider about your personal risk and what you can do to protect your bones.
Osteoporosis Symptoms
Osteoporosis is sometimes referred to as a “silent” condition. That’s because it often has no symptoms.
As it progresses, it can lead to symptoms like:
- Back pain
- Sudden back pain
- Joint pain
- Changes in posture
- Stooping or loss of height
But most people aren’t aware they have osteoporosis until they fracture or break a bone. That’s why it’s so important to be aware of osteoporosis and take steps to protect your bone health.
Tips to Manage IBD and Protect Your Bones
“The number one thing is to make sure that your disease is always in remission,” says Bhattacharya. “Follow up with your doctors regularly. Take your immunosuppressant medication. Make sure your disease is in remission so that you never request steroids.”
Aside from that, “just maintain a regular healthy lifestyle,” he adds.
Eat a Healthy, Nutritious Diet
Proper nutrition can help you manage IBD, prevent nutritional deficiencies or malnutrition, and maintain a healthy weight.
While there’s no one diet to ease IBD and promote bone health, plan to eat a well-balanced diet full of foods you can tolerate, such as low-fiber fruits and vegetables and lean protein. Aim to also get plenty of calcium and vitamin D to help preserve bone strength.
Women ages 50 and under and men ages 70 and under should aim to get 1,000 mg of calcium each day and increase intake to 1,200 mg each day once women reach age 51 and men reach age 71. The recommended vitamin D intake is 400-800 IU a day for most adults under age 50, and 800-1,000 IU a day for those 50 and up.
Stay Active
When you’re dealing with IBD symptoms, exercise may be the last thing on your mind. But evidence suggests that staying active can help you manage your condition.
Research has also found that resistance exercises in particular — such as weightlifting — can help preserve bone health and muscle mass. However, low-impact exercises — like walking or riding a bike — are best for people who have osteoporosis, as they don’t overtax the joints. Read more about exercises to avoid for osteoporosis.
Maintain a Healthy Weight
IBD symptoms like persistent diarrhea can lead to weight loss. And being underweight can weaken bone health and increase your risk of osteoporosis.
Be sure to eat a healthful diet to help you avoid malnutrition. Try to reach and maintain a healthy weight to promote optimal bone health.
Quit Smoking
Smoking is bad for your health in many ways. It can harm your digestive tract as well as weaken bones and increase fracture risk.
If you smoke, quitting can help decrease IBD activity and reduce the risk of bone loss and fractures. One study shows that quitting may help increase bone mass previously lost due to smoking.
Ask your doctor if you need help with quitting. You may benefit from the use of a smoking cessation aid.
Avoid Alcohol
Evidence suggests that alcohol may contribute to inflammation when you have IBD. Research has also found that chronic, excessive alcohol consumption increases osteoporosis risk.
Many people who have IBD tend to avoid alcohol altogether, as it tends to worsen IBD symptoms. Though mild consumption may have a negligible impact. If you do drink, be sure to so in moderation: That means one drink a day (or less) for women, and two (or less) for men.
When to Talk to Your Doctor About Bone Health
“If you have IBD and you’ve been on steroids, ask your doctor about osteoporosis immediately, and let the doctor decide based on the risk factors whether they need to be screened,” says Bhattacharya.
Because there are often no symptoms of osteoporosis until a bone breaks, routine screening can help prevent osteoporosis. Screening is easy and only takes five to 10 minutes. Early detection can help you take proper steps to prevent fractures and promote bone health.
Routine screening for osteoporosis is typically done:
- After age 65 for women, 70 for men, or sooner depending on your personal risk factors
- Every one or two years, or more often depending on your health
- After a bone fracture in those over age 50
- When taking new medication associated with low bone mass or bone loss
Talk to your doctor at your next health exam about getting screened for osteoporosis.
This article was made possible with support from Amgen.
American Bone Health. How Often Should I Get Tested?
https://americanbonehealth.org/bone-density/how-often-should-i-have-a-bone-density-test/.
Berkowitz L, et al. Impact of Cigarette Smoking on the Gastrointestinal Tract Inflammation: Opposing Effects in Crohn’s Disease and Ulcerative Colitis. Frontiers in Immunology. January 2018. https://www.frontiersin.org/articles/10.3389/fimmu.2018.00074/full
Bone Health & Osteoporosis Foundation. Evaluation of Bone Health/Bone Density Testing. https://www.bonehealthandosteoporosis.org/patients/diagnosis-information/bone-density-examtesting/.
Bone Health & Osteoporosis Foundation. Food and Your Bones — Osteoporosis Nutrition Guidelines. https://www.bonehealthandosteoporosis.org/patients/treatment/nutrition/.
Bone Health & Osteoporosis Foundation. Get the Facts on Calcium and Vitamin D. https://www.bonehealthandosteoporosis.org/patients/treatment/calciumvitamin-d/get-the-facts-on-calcium-and-vitamin-d/
Bone Health & Osteoporosis Foundation. Osteoporosis Exercise for Strong Bones. https://www.bonehealthandosteoporosis.org/patients/treatment/exercisesafe-movement/osteoporosis-exercise-for-strong-bones/.
Centers for Disease Control and Prevention. Inflammatory bowel disease (IBD). Complications. https://www.cdc.gov/ibd/data-and-statistics/comorbidities.html.
Cleveland Clinic. When (and Why) Should I Start Screening for Osteoporosis? https://health.clevelandclinic.org/when-and-why-should-i-start-screening-for-osteoporosis/.
Crohn’s and Colitis Foundation. Bone Loss. https://www.crohnscolitisfoundation.org/sites/default/files/2020-03/boneloss.pdf.
Crohn’s and Colitis Foundation. What is IBD? https://www.crohnscolitisfoundation.org/what-is-ibd.
Crohn’s and Colitis Foundation. What Should I Eat? https://www.crohnscolitisfoundation.org/diet-and-nutrition/what-should-i-eat.
Crohn’s and Colitis Foundation. When to Take Stomach Pain and other GI Issues Seriously. https://www.crohnscolitisfoundation.org/what-is-ibd/symptoms.
Engels M, et al. Exercise in patients with inflammatory bowel diseases: current perspectives. Clinical and Experimental Gastroenterology. June 2017. https://www.dovepress.com/exercise-in-patients-with-inflammatory-bowel-diseases-current-perspect-peer-reviewed-fulltext-article-CEG.
Epsley S, et al. The Effect of Inflammation on Bone. Frontiers in Physiology. January 2021. https://www.frontiersin.org/articles/10.3389/fphys.2020.511799/full.
Hodgens A, et al. Corticosteroids. July 2022. https://www.ncbi.nlm.nih.gov/books/NBK554612/.
Hoffman P, et al. Prevalence, Risk Factors and Course of Osteoporosis in Patients with Crohn’s Disease at a Tertiary Referral Center. Journal of Clinical Medicine. November 2019. https://www.mdpi.com/2077-0383/8/12/2178.
Hong AR, et al. Effects of Resistance Exercise on Bone Health. Endocrinology and Metabolism (Seoul). December 2018. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6279907/.
Kiyota Y, et al. Smoking cessation increases levels of osteocalcin and uncarboxylated osteocalcin in human sera. Nature. October 2020. https://www.nature.com/articles/s41598-020-73789-4.
Lima CA, et al. “Risk factors for osteoporosis in inflammatory bowel disease patients.” World Journal of Gastrointestinal Pathophysiology. November 2015. https://www.wjgnet.com/2150-5330/full/v6/i4/210.htm.
Lo B, et al. Incidence, Risk Factors and Evaluation of Osteoporosis in Patients With Inflammatory Bowel Disease: A Danish Population-Based Inception Cohort With 10 Years of Follow-Up. Journal of Crohn’s and Colitis. https://academic.oup.com/ecco-jcc/article/14/7/904/5722012.
Mayo Clinic. Bone health: Tips to keep your bones healthy. https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/bone-health/art-20045060.
Mayo Clinic. Osteoporosis. https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968.
National Institute on Aging. Osteoporosis. https://www.nia.nih.gov/health/osteoporosis.
National Institute of Arthritis and Musculoskeletal and Skin Diseases. Osteoporosis. https://www.niams.nih.gov/health-topics/osteoporosis
NIH Osteoporosis and Related Bone Diseases National Resource Center. Smoking and Bone Health. https://www.bones.nih.gov/health-info/bone/osteoporosis/conditions-behaviors/bone-smoking.
Personal interview with Abhik Bhattacharya, MD, gastroenterologist and IBD specialist at The Susan and Leonard Feinstein IBD Center, Mount Sinai Health System in New York City.
Ramos GP, et al. Alcohol Use in Patients With Inflammatory Bowel Disease. Gastroenterology & Hepatology. May 2021. https://www.gastroenterologyandhepatology.net/archives/may-2021/alcohol-use-in-patients-with-inflammatory-bowel-disease/.
Wang X, et al. Alcoholism and Osteoimmunology. Current Medicinal Chemistry. 2021. https://www.eurekaselect.com/article/106118.
West Virginia Department of Health & Human Resources. Osteoporosis Risk Factors. https://dhhr.wv.gov/hpcd/FocusAreas/osteoporosis/Pages/Osteo-Risk-Factors.aspx.
World IBD Day. About us. https://worldibdday.org/about-us.
Xu C, et al. Dietary Patterns and Progression of Knee Osteoarthritis: Data from the Osteoarthritis Initiative. The American Journal of Clinical Nutrition. January 2020. https://academic.oup.com/ajcn/article/111/3/667/5698103.