Listen to Your Gut: A Webinar on Inflammatory Bowel Disease (IBD)
Inflammatory bowel diseases (IBD) are chronic, remitting and relapsing inflammatory conditions of the gastrointestinal tract. It includes Crohn’s disease and ulcerative colitis. While Crohn’s disease is inflammation that affects any part of the gastrointestinal tract from the mouth to the anus, ulcerative colitis affects only the colon in a continuous manner from the rectum up. This educational webinar addresses current knowledge on IBD, including what it is, how it is diagnosed and who it affects. The webinar also provides an overview of the currently available therapeutic options and highlights current research of immunosuppressive treatment of IBD.
Bharati Kochar, MD, MSCR, Department of Medicine, Division of Gastroenterology and Hepatology, University of North Carolina at Chapel Hill (UNC), was joined by CreakyJoints patients and staff for a one-hour webinar to discuss this topic. The presentation concludes with a Q&A session.
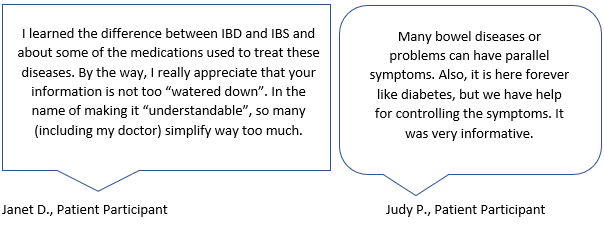
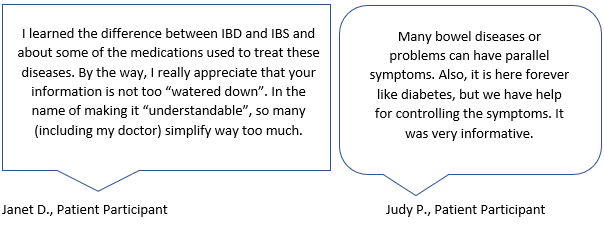
Here’s what patient participants said they learned from this webinar:
Here are a few key learnings from CreakyJoints staff:
1.Inflammatory bowel disease (IBD) is different from irritable bowel syndrome (IBS) although the two conditions are commonly confused. IBD is an autoimmune and chronic condition that causes inflammation of the gastrointestinal tract. IBS is not an autoimmune condition and does not cause inflammation of the gastrointestinal tract.
2. There is no single cause of IBD. IBD is caused by many factors, such as immune system disturbances (overactive immune response), gut microbiome disturbances and environmental triggers. The “hygiene hypothesis for autoimmune and allergic diseases” provides one common explanation. It postulates that limited exposure to microbes changes the balance of the immune system and leads to IBD. There is also a genetic component to IBD, but more research is needed to understand what causes IBD.
3. There are different kinds of IBD remission: symptomatic remission, endoscopic remission and histological remission.
a) Symptomatic remission means that a patient may not be experiencing any symptoms from their IBD any longer. Just because someone is not experiencing symptoms does not mean they do not have the disease and, therefore, should not stop treatment. Although a patient is not experiencing symptoms, lab tests and imaging results may still show persistent inflammation in the GI tract requiring continued treatment.
b) Endoscopic remission means that during a scope, such as a colonoscopy or a sigmoidoscopy, no inflammation is seen.
c) Histological remission means that when a biopsy is repeated there is no evidence of inflammation seen in the intestines. This would be accompanied by endoscopic remission.
4. A colonoscopy can indicate inflammation in the colon. If this is the case, a biopsy may be recommended to determine whether the cause of inflammation is indeed inflammatory bowel disease. A biopsy can help determine if you have Crohn’s disease or ulcerative colitis (UC).
5. There are a number of medication available to treat IBD, both Crohn’s disease and ulcerative colitis; many of these medications change the way the immune system works.
The above are just a few takeaways from the one-hour event. Check out the embedded video below to view the webinar in its entirety, or head on over to youtube.com/CreakyJoints.





