Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
Meeting up virtually right now is the safest way to connect with family and friends outside of your household without the risk of contracting COVID-19. Depending on where you live, you may even be currently ordered to stay at home except for permitted work or essential errands.
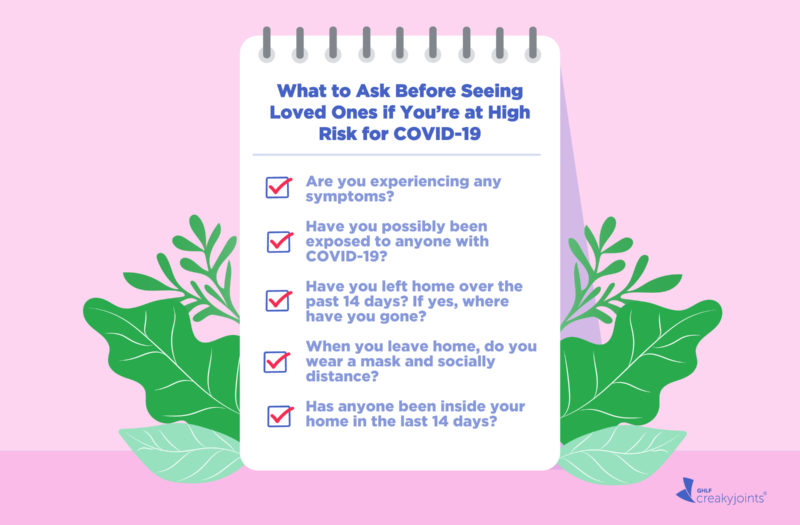
However, if you truly feel like you can’t go without seeing a loved one any longer and local regulations permit it, there are certain questions that are important to ask that person before meeting up — especially if you’re immunocompromised or have a chronic illness that increases your risk for COVID-19 complications.
The next-safest option may be seeing people outside while wearing masks and staying socially distant (at least six feet apart) the whole time.
“Any time you get together with someone, it’s really important to understand if they’ve been quarantining the same way you have so you can gauge your level of risk,” says Alaina Brinley Rajagopal, MD, an emergency medicine physician in Southern California who has treated COVID-19 patients.
It may feel unusual at first to run through a list of questions, but keep in mind that these are highly unusual times that call for extra steps to ensure your safety.
“If you’re in a position to genuinely measure somebody else’s safety protocols, you have to be really explicit about what they’re doing and what they’re not doing,” says Kim Gorgens, PhD, Clinical Professor and Director of Continuing Education at the Graduate School of Professional Psychology at the University of Denver. “What I’ve found is that we’re not all speaking the same language, and the word ‘safe’ has no universal definition.”
In this scenario, it’s best not to beat around the bush: Be kind but straightforward with your loved one. Tell them that you have a few questions to ask them to ensure you’re managing your own risk in the best way. Shifting the focus to your own concerns and away from your loved one’s habits may help them understand that you’re not judging them, but rather looking out for your own safety as an immunocompromised or high-risk individual, says Dr. Gorgens.
For example, you might say something like: “I’ve talked to my doctor about being at high risk for COVID-19 complications, and it’s really important that I avoid any possible exposure. Do you mind if I ask you a few questions before we meet up, for my own peace of mind?”
Avoid focusing the conversation on the other person with statements like “I don’t think you’re being careful enough” or “Well, we can’t meet up if you haven’t been wearing a mask.”
Dr. Brinley Rajagopal suggests starting with a friendly phrase such as: “I love you and I really want to see you, but it’s very important to me to make sure we’re on the same page as far as following guidelines.”
There are five important questions you can ask your loved one to determine how they’ve been managing their exposure to COVID-19, and if it’s safe for you to be around them, says Dr. Brinley Rajagopal.
“I would definitely recommend going through these questions with every person you choose to get together with, every time you get together,” she says. “And even when you do get together, still wear a mask, stay six feet apart as much as you can, and continue to adhere to CDC [U.S. Centers for Disease Control and Prevention] guidelines.”
If that person answers in short or vague sentences, think about what that may tell you about how closely they’re following COVID-19 mitigation efforts.
“It’s really important to trust your gut, so if something doesn’t seem right to you, then I wouldn’t get together with that person,” says Dr. Brinley Rajagopal.
1. Are you experiencing any symptoms?
Kindly ask your loved one if they have any of the following symptoms: fever or chills, cough, shortness of breath, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, or diarrhea.
We’ve all heard this laundry list of symptoms throughout the pandemic, but it’s important to ask your loved one anyhow. After all, one 13-year-old girl spread COVID-19 to 11 other people at a family gathering after having only nasal congestion as a symptom, per the U.S. Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
In other words, a symptom that your loved one might brush off as something minor may be a warning sign for you.
“Especially if someone is immunocompromised, it’s really important to avoid getting this virus, because there’s no way to predict who’s going to get really sick and who’s going to get mild symptoms,” says Dr. Brinley Rajagopal.
If they answer yes to any of these symptoms, do not get together. If the answer is no, continue to the next question.
2. Have you possibly been exposed to anyone with COVID-19?
If your loved one says something like “I don’t think so” or “I don’t know,” it may be most prudent to interpret that as a “yes” — especially if they’ve been other friends or family or people they work with.
“I’ve seen patients upon follow-up who contracted COVID-19, and surprisingly a lot of people knew they got it from a family member or friend gathering,” says Magdalena Cadet, MD, a clinical rheumatologist and Associate Attending Physician at NYU Langone Health in New York City.
The reason “I don’t know” may not be a good enough answer is because it’s estimated that 40 percent of COVID-19 infections are asymptomatic, meaning those infected never show symptoms of the disease, per the CDC.
If they answer yes to this question, do not get together. If the answer is no, continue to the next question.
Of course, someone will not know if they’ve been around someone who themselves is asymptomatic and doesn’t know if they have COVID-19, which is why the next few questions are so important.
3. Have you left the house in the last 14 days? If yes, where have you gone?
Some places are considered riskier than others, so take note of where your loved one has been.
For instance, researchers reviewed anonymized data from nearly 100 million Americans living in New York City, Chicago, and Washington, D.C., plus seven other metro areas in a November 2020 report published in the journal Nature.
They tracked visits to more than 550,000 cafes, hotels, and other points of interest in those regions, and found that certain venues like full-service restaurants, gyms, hotels, cafes, religious organizations, and limited-service restaurants produced the largest predicted increases in infections when reopened.
“Every time you leave your house, there’s a greater risk of getting the virus,” says Dr. Brinley Rajagopal. “So it makes sense to reduce that risk as much as possible to accomplish the tasks you need to do and see the family members or friends you need to see.”
If your loved one quickly went to the grocery store to pick up food, they were most likely in a lower-risk environment than if they met up with friends for dinner or at a bar.
“Also take into account the occupation of that person,” says Dr. Cadet. “If someone is an essential worker — such as a health care worker or bus driver — their risk of exposure is very different from someone who is working from home right now.”
If you feel comfortable with your loved one’s answer and it aligns with your own careful quarantine habits, move on to the next question.
4. When you leave home, do you wear a mask and stay at least 6 feet away from others?
Strong evidence shows the efficacy of masks, and the CDC recently updated its guidelines to note that masks protect both the wearer and those around that individual from spreading the virus.
In fact, widespread use of masks could prevent nearly 130,000 of 500,000 COVID-related deaths estimated to occur by March 2021 in the United States, per an October 2020 study published in the journal Nature Medicine.
If your loved one groans about wearing their mask or makes comments that hint that they may be cutting corners, take that as a red flag. For instance, look out for phrases like, “Oh sure, I wear a mask when I’m right next to people” — remember, masks are meant to be used in addition to social distancing.
If they answer no, do not get together. If the answer is yes, continue to the next question.
5. Has anyone been inside your home in the last 14 days?
If your loved one has had guests over, ask if they both wore masks and remained six feet apart. Remember: Just because it’s someone they trust doesn’t mean that individual isn’t carrying the virus.
“Also ask if it was one person or multiple people who came over,” says Dr. Brinley Rajagopal.
There’s a difference between having a repair person come to fix a broken faucet for 20 minutes and a group of friends eating and drinking together for a few hours.
“I’m more concerned with large group gatherings, even with ‘people they trust.’ We’ve heard over and over from people ‘This is someone I trust, this is someone who’s being careful,’ but then that careful person ends up getting COVID-19 and infecting who they’re talking to,” says Dr. Brinley Rajagopal.
If they haven’t had any contact with other people or left the house in the last 14 days, it may be safe to get together, she says.
“However, it’s still important for everyone to stay distanced and wear masks,” she says. “Also, be sure to follow the regulations in your area. If there’s a stay-at-home order, stay at home.”
If you’ve reached this point and feel comfortable meeting up with your loved one, you may be able to do so carefully if local regulations allow. However, still follow standard mitigation efforts like social distancing and mask wearing. Also note that it’s better to spend time with others outdoors than indoors.
When you do need to let your loved one know that you can’t meet up, they may manage their emotions in different ways — they might be very understanding, or they could respond defensively or by trying to guilt-trip you. However, try not to dwell on negative responses, and remember that they may be going through very different experiences if they are not a high-risk or immunocompromised individual.
“It says everything about them not walking in your shoes,” says Dr. Gorgens. “They don’t see the realities of exposing yourself to any kind of risk with underlying health issues or a compromised immune system.”
In any scenario, keep in mind that the safest way to connect with your loved ones without the added risk is via a phone call or video chat. “Given the current surge, I think the best thing right now is to do virtual meetings,” says Dr. Cadet.
Get Free Coronavirus Support for Chronic Illness Patients
Join the Global Healthy Living Foundation’s free COVID-19 Support Program for chronic illness patients and their families. We will be providing updated information, community support, and other resources tailored specifically to your health and safety. Join now.
Chang S, et al. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. November 10, 2020. doi: https://doi.org/10.1038/s41586-020-2923-3.
COVID-19 Pandemic Planning. COVID-19 (Coronavirus Disease). U.S. Centers for Disease Control and Prevention. September 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html.
Interview with Alaina Brinley Rajagopal, MD, an emergency medicine physician in Southern California
Interview with Kim Gorgens, PhD, Clinical Professor and Director of Continuing Education at the Graduate School of Professional Psychology at the University of Denver
Interview with Magdalena Cadet, MD, a clinical rheumatologist and associate attending physician at NYU Langone Health in New York City
Lee S, et al. Clinical Course and Molecular Viral Shedding Among Asymptomatic and Symptomatic Patients With SARS-CoV-2 Infection in a Community Treatment Center in the Republic of Korea. JAMA Internal Medicine. August 6, 2020. doi: https://www.doi.org/10.1001/jamainternmed.2020.3862.
Reiner RC, et al. Modeling COVID-19 scenarios for the United States. Nature Medicine. October 23, 2020. doi: https://doi.org/10.1038/s41591-020-1132-9.
Schwartz NG, et al. Adolescent with COVID-19 as the Source of an Outbreak at a 3-Week Family Gathering — Four States, June–July 2020. MMWR Morbidity and Mortality Weekly Report (MMWR). doi: http://dx.doi.org/10.15585/mmwr.mm6940e2.