Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
If you have an inflammatory or autoimmune type of arthritis or rheumatic disease — such as rheumatoid arthritis, psoriatic arthritis, axial spondyloarthritis, or lupus — you’ve likely had questions about the COVID-19 vaccine. Among the most common concerns from the CreakyJoints community:
- Do I need a third dose?
- Do immunosuppressant medications make the vaccine less effective?
- Should I temporarily stop medication when getting the vaccine to boost the immune response?
- Will the vaccine cause a disease flare?
- Is one type of vaccine better for autoimmune or inflammatory disease patients than another?
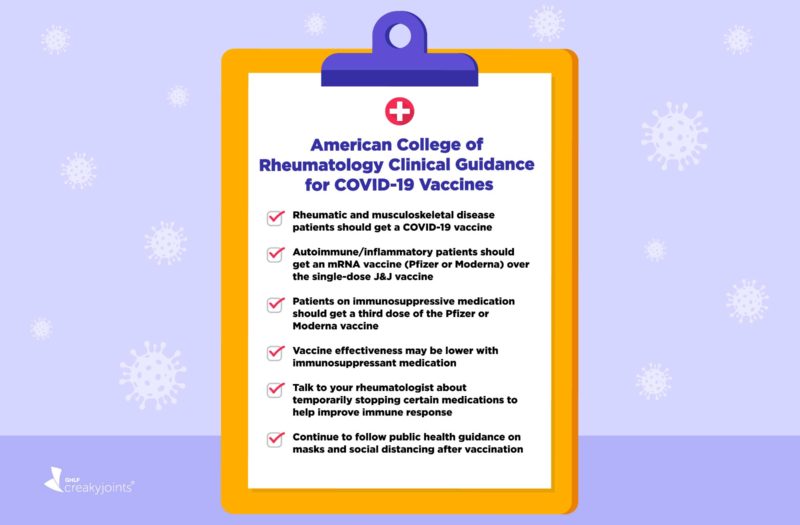
Updated guidance from the American College of Rheumatology continues to provide answers for patients and their providers.
First issued in February 2021 and updated regularly as new research emerges, the guidance advises health care providers on giving the COVID-19 vaccine to rheumatic disease patients to 1) encourage vaccine uptake; 2) improve vaccine effectiveness by adjusting medications that could affect immune response; and 3) ensure patients stay safe and protected from COVID-19 generally.
As a patient, being aware of the guidance can help you have informed conversations with your doctor. Remember that the guidance is not meant to be personalized for each individual, so discussing your situation with your doctor is key.
The two main COVID-19 vaccine message doctors want rheumatic disease patients to know now are:
Vaccinated? Get a third dose: “Almost all patients who are on immunosuppressant or immunomodulating drugs need an additional vaccine dose,” says rheumatologist Jeffrey Curtis, MD, MPH, Professor of Medicine at the University of Alabama at Birmingham, who led the task force that created the guidance. Dr. Curtis is also a Co-Principal Investigator of ArthitisPower, our patient-centered research registry.
Not vaccinated? Get the vaccine. “We have ample data that the vaccine is safe for people with inflammatory and autoimmune rheumatic disease,” says Rebecca Sadun, MD, MPH, Assistant Professor of Medicine at Duke University and a member of the ACR vaccine guidance task force. “There are no significant safety concerns and we have enough patients vaccinated to feel more than comfortable saying this.”
With that in mind, here are important highlights from the guidance.
1. People with rheumatic and musculoskeletal disease (including autoimmune and inflammatory disease) SHOULD GET a COVID-19 vaccine
“We want patients to get a COVID-19 vaccine — hard stop,” says Dr. Curtis. People with autoimmune and inflammatory rheumatic diseases can be at a higher risk for hospitalized COVID-19 and worse outcomes compared to the general population, which is why getting protection from the vaccine is so critical.
The vaccine is safe for autoimmune and inflammatory rheumatic diseases.
The ACR guidance says, “beyond known allergies to vaccine components, there are no known additional contraindications to COVID-19 vaccination.” This means that simply having an autoimmune or inflammatory rheumatic disease — or taking immunomodulating medication to treat it — is not a reason to not get a COVID-19 vaccine.
While vaccination should ideally occur in autoimmune and inflammatory patients with well-controlled disease, COVID-19 vaccination should occur as soon as possible, regardless of disease severity, except in people with life-threatening illness. In other words, most people who are having disease flares or other symptoms that are not life-threatening should likely still be vaccinated, per your doctor’s advice.
2. People with autoimmune or inflammatory arthritis who are not vaccinated should get an mRNA vaccine (Pfizer or Moderna) instead of a one-dose vaccine (Johnson & Johnson)
The reason for this is twofold. One is that the mRNA vaccines are slightly more protective against COVID-19 infections than the J&J vaccine. If someone is immunocompromised because they are taking immunosuppressant medication, it helps to start with a vaccine that offers slightly more protection in the first place, says Alfred Kim, MD, PhD, Assistant Professor of Medicine, Pathology, and Immunology at Washington University in St. Louis, Missouri.
The other is that right now, third doses for immunocompromised patients are available only to those who received the Pfizer or Moderna vaccine, and it’s clear that people who are on immunosuppressive or immunomodulating medications need this third dose, says Dr. Curtis.
This recommendation may change if an additional dose becomes authorized and recommended for the Johnson & Johnson vaccine. (Right now, there is not enough data to support recommending an additional dose.)
3. People on immunosuppressive or immunomodulating medication should get a third dose of the Pfizer or Moderna vaccine
An additional third dose is now routinely recommended for everyone on medication that affects immune system function, at least 28 days after completing the second dose of the Pfizer or Moderna vaccine.
This applies to most medications for inflammatory and autoimmune rheumatic diseases with one exception: hydroxychloroquine (Plaquenil). Because this medication does not suppress the immune system, those who take only hydroxychloroquine do not need a third vaccine dose. (However, they could get booster shots eight months after their second vaccine dose, in line with recommendations for the general population.)
You should get ideally get the same type of vaccine for your third dose as you did for your first two (if you got Moderna originally, get Moderna for your third dose). But switching to the other mRNA vaccine is okay if you can’t get the same as your original series.
Read more here about getting the third COVID-19 vaccine dose for immunocompromised people.
4. COVID-19 vaccine immune response is lower with many immunomodulating and immunosuppressant medications, but you still get protection
This is why the third dose is recommended — to help immunocompromised patients mount a more robust response to the vaccine.
Doctors and researchers are just beginning to get data on rheumatology patients’ response to the COVID-19 vaccine. Overall, the news is very positive: Most people with autoimmune and inflammatory conditions will have a good response to the COVID-19 vaccine.
In one notable study of nearly 700 autoimmune/inflammatory rheumatic disease patients, 86 percent developed antibodies after the second vaccine dose, compared to 100 percent of healthy controls.
However, vaccine response can vary considerably by medication type, which is why the ACR guidance makes recommendations for withholding certain medications or adjusting the timing of when you take medications relative to when you get the vaccine (more on this below).
Even if the vaccine is some degree less effective, it’s still critically important to get it, including the third dose — and to feel assured that you are more protected from serious COVID-19 complications as a result.
“Remember that any vaccine usually doesn’t work as well in people who take immunomodulating medication,” says Dr. Curtis. “But even if it doesn’t protect you at the same level as someone your age without your health condition, that does not mean the vaccine is worthless. We want patients to get the vaccine so they have as much protection as possible.”
Think of it this way: If you had a choice between being in a snowstorm wearing a winter coat, hat, gloves, and scarf (fully effective vaccine) versus a just a winter coat (less effective vaccine) versus just a T-shirt (no vaccine), of course you’d prefer having all the winter attire. But having the coat is way better than just the T-shirt.
5. Antibody testing is not recommended to check immunity after vaccination
There’s not enough data about what antibody test results mean to use them to make decisions about whether someone’s had a good response to the vaccine. The ACR guidance recommends that everyone with an autoimmune or inflammatory rheumatic disease get the vaccine in the first place, then get the third dose according to recommendations. Knowing your antibody levels shouldn’t change this.
6. There is a theoretical risk of a disease flare after getting a COVID-19 vaccine, but consider the big picture
The ACR guidance reminds us that, given the seriousness of a COVID-19 infection, the benefit of vaccination far outweighs the potential risk for a disease flare or worsening. So far, data suggests that side effects from the vaccine are similar in autoimmune and inflammatory rheumatic disease patients and the general population. What’s more, getting infected with COVID-19 can also cause disease flares — not to mention countless other health problems, including life-threatening ones.
Changes to Medication Timing Around the COVID-19 Vaccine
Should patients stop taking certain medications before or after getting the COVID-19 vaccine to help the body mount a stronger immune response? With data from preliminary studies, the ACR guidance highlights a few specific medications that have been linked to a lower immune response to the vaccine.
This advice is a jumping-off point for a conversation with you and your doctor and it doesn’t apply to every person across the board. Stopping a medication could increase the risk of having a disease flare, so it may not be the right choice for you. Some medications do not need to stopped because the data is not strong enough to suggest that doing so would considerably increase the response to the vaccine.
There’s a lot here that experts still do not know, and it’s best to discuss your personal situation with your provider.
Third Vaccine Dose
The ACR guidance recommends a slightly different approach for the third vaccine dose than for the original COVID-19 vaccine series (below).
In the original two-dose vaccine series, you’re getting two vaccines spaced relatively close together (three weeks apart for Pfizer and four for Moderna). If you hold medication for one to two weeks after each dose, you would be off your medication for a prolonged period of time and your risk of having a flare could increase, explains Dr. Sadun.
Most rheumatic disease patients will be getting their third dose many weeks or months after their second dose, so this timing consideration is less of an issue.
1. Hold immunomodulating or immunosuppressive medications (except for glucocorticoids and most biologics) for 1-2 weeks after the third dose, assuming disease activity allows
This applies to the following medications:
- Apremilast (Otzela)
- IVIG
- Sulfasalazine (Azulfidine)
- Leflunomide (Arava)
- Azathioprine (Imuran)
- Cyclophosphamide (Cytoxan)
- Belimumab (Benlysta)
- Mycophenolate (CellCept)
- Oral calcineurin inhibitors (cyclosporine or tacrolimus)
- Methotrexate
- JAK inhibitors (Xeljanz, Olumiant, Rinvoq)
- Abatecept (Orencia)
The reason for holding these medications after the third dose is to try to help your body mount as robust a response to the vaccine as possible, says Dr. Sadun. “For most patients, holding their medication for a week or two does not put them at risk of a serious flare. With the third dose, we’re trying to bring the blunted vaccine response to a full response.”
2. There isn’t a clear answer about holding most biologics, including TNF inhibitors and interleukin inhibitors
Many people have questions about whether to stop taking biologics that are not included in the above list, and unfortunately, there are no definite rules. The ACR guidance notes that its task force was mixed about whether to advise for or against holding the following biologics at the time of the third dose:
- TNF biologics (ex: Cimzia, Enbrel, Humira, Remicade, Simponi and Simponi Aria)
- IL-6 biologics (ex: Actemra and Kevzara)
- IL-1 biologics (ex: Kineret, Ilaris)
- IL-17 biologics (ex: Cosentyx, Taltz)
- IL-23 biologics (ex: Skyrizi, Tremfya)
- IL-12/23 biologics (ex: Stelara)
Data suggests that people on these medications do not have a dramatically reduced response to the COVID-19 vaccine. Some doctors may recommend you temporarily hold them out of an abundance of caution; maybe there’s a chance doing so could increase your response slightly. Others may recommend that you continue to take them because stopping them could impact your risk of a flare and there is unlikely to be a big impact on vaccine response.
It’s a personal decision that you and your doctor can discuss together.
3. Discuss timing around rituximab with your doctor before getting the third dose
Your doctor may recommend that you try to get your third vaccine dose two to four weeks before your next rituximab infusion. Here’s why:
This biologic, used to treat rheumatoid arthritis, lupus, and vasculitis, is an infusion typically administered every six months. It gets rid of B cells circulating in your blood and in your tissues, which helps reduce inflammation. However, these B cells are needed to generate an effective immune system response to vaccines.
More than any other rheumatic disease therapy, rituximab is linked with a poor response to the COVID-19 vaccine. Getting the COVID-19 vaccine close to your NEXT rituximab dose — when your levels of B cells would be higher — may allow your body to mount a better response to the vaccine.
Getting the third COVID-19 vaccine dose close to your LAST rituximab infusion likely means you will have a poor response to it. Determining optimal timing with your doctor is critical.
Original Vaccine Series
No Change in Medication Timing for
In the case of many immunomodulating medications for rheumatic diseases, the guidance suggests that patients do not stop taking medications before or after getting the vaccine. This is because there is no reason to think, based on available data, that stopping these medications would markedly increase your body’s immune system response to the vaccine.
This applies to:
- Hydroxychloroquine (Plaquenil)
- Apremilast (Otezla)
- IVIG
- Low-dose glucocorticoids (ex: prednisone, daily dose < 20 mg)
- Sulfasalazine (Azulfidine)
- Leflunomide (Arava)
- Azathioprine (Imuran)
- Cyclophosphamide (Cytoxan) (oral)
- TNF biologics (ex: Cimzia, Enbrel, Humira, Remicade, Simponi and Simponi Aria)
- IL-6 biologics (ex: Actemra and Kevzara)
- IL-1 biologics (ex: Kineret, Ilaris)
- IL-17 biologics (ex: Cosentyx, Taltz)
- IL-23 biologics (ex: Skyrizi, Tremfya)
- IL-12/23 biologics (ex: Stelara)
- Belimumab (Benlysta)
There were differing views about high-dose steroids (daily doses ≥ 20 mg.) Some doctors agree that no changes in medication timing are needed, while others may recommend that patients taper steroids to a lower dose before receiving a COVID-19 vaccine. This would be done to make sure the vaccine protects you as much as possible.
Consider Changes in Medication Timing for
The guidance highlights a few types of medications where there was moderate consensus among the task force about temporarily skipping doses before or after receiving vaccine OR trying to time when you get the vaccine so it occurs at a certain point during the course of your treatment.
This means some evidence suggests this may be helpful at increasing the body’s immune response, but it’s not a hard-and-fast rule. Your doctor may have a different recommendation based on your personal situation.
Acetaminophen, Non-steroidal Anti-Inflammatory Drugs (NSAIDs): Skip for 24 hours prior to vaccination
The CDC has recommended that people not take acetaminophen (such as Tylenol) and NSAIDs (such ibuprofen/Advil or naproxen/Aleve) before getting the vaccine for the purpose of trying to prevent vaccine side effects. The ACR guidance recommends that people with stable disease avoid taking these medications, which are frequently used to manage pain and other symptoms, for 24 hours before the vaccine for those with stable disease. Both the CDC and the ACR guidance say it is okay to use these medications after the vaccine to treat symptoms.
Methotrexate: Skip for 1 week after each vaccine dose; skip for 2 weeks after a single-dose vaccine
The guidance recommends that patients with well-controlled disease can skip methotrexate for one week after getting each dose of the COVID-19 vaccine. If your disease is not well-controlled — and skipping MTX is likely to make you prone to flare — your doctor may advise against this. If you get a single-dose vaccine (Johnson & Johnson), the guidance recommends holding MTX for two weeks after. Methotrexate is typically taken orally or injected once a week for rheumatic diseases.
Read more here about methotrexate and the COVID-19 vaccine.
Oral calcineurin inhibitors (ex: cyclosporine or tacrolimus): Skip for 1 week following each vaccine dose
The guidance recommends that patients with stable disease stop taking this medication for one week after each COVID-19 vaccine dose.
JAK inhibitors (ex: Xeljanz, Olumiant, Rinvoq): Skip for 1 week after each vaccine dose
The guidance recommends that patients can stop taking these medications, which are oral pills taken daily, for one week after each COVID-19 vaccine dose.
JAK inhibitors work in part by reducing the activity of immune system proteins called interferon, which play an important role in how your immune system responds to invading viruses.
“Interferon is kind of like the captain in of the immune system army signaling all of the troops and telling them when and where to deploy. When you reduce interferon, you can throw your immune system’s response into chaos,” says Dr. Curtis. The thinking is that holding JAKs after getting the COVID-19 vaccine may improve how your body is able to recognize and fight viral infections like the coronavirus.
Mycophenolate (CellCept): Skip for 1 week after each vaccine dose
The guidance recommends that patients with stable disease stop taking this medication for one week after each COVID-19 vaccine dose.
Abatacept (Orencia), injectable form: Skip one week before and after the first vaccine dose only
The injectable form of this medication is taken weekly. This applies only to the first vaccine dose. The guidance suggests that there’s no need to skip abatacept before or after the second vaccine dose.
Abatacept affects the function of T cells, which Dr. Curtis describes as the immune system’s matchmaker — they ensure all the different components are communicating and working together. Since the coronavirus is brand-new (or novel) and most of our immune systems have never encountered it before, it may be important to not affect the work of T cells right before or after getting the vaccine.
Abatacept (Orencia), IV form: Get COVID-19 vaccine 4 weeks after your last infusion, then skip a week and get next infusion
For the IV form of the medication, which is typically given every four weeks, the guidelines suggest timing when you get the COVID-19 vaccine so it’s four weeks after your last infusion (as in, right before you’re due for your next one), then getting the vaccine, then waiting a week to get the next infusion. The schedule would look like this:
- Get abatacept infusion
- 4 weeks later: Get COVID-19 vaccine
- 1 week later: Get next abatacept infusion
Rituximab (Rituxan): Get COVID-19 vaccine approximately 4 weeks before next infusion, then delay next infusion by 2-4 weeks after second vaccine dose — if possible
As described above, rituximab is linked with a poor response to the COVID-19 vaccine because it depletes the immune system’s B cells, which are needed to produce antibodies. The further away you are from your last rituximab infusion, the better off you may be in terms of having a stronger vaccine response. The schedule would look like this:
- Get rituximab infusion
- Wait 4 weeks before next dose (about 5 months later) and get COVID-19 vaccine
- 3-4 weeks later: Get second COVID-19 vaccine (depending on Moderna or Pfizer)
- 2-4 weeks later: Get next rituximab infusion
This kind of schedule is recommended for patients whose disease activity will allow them to be off medication for an extended period, so it may not be advised for all patients.
Read more here about rituximab and the COVID-19 vaccine.
Cyclophosphamide infusion: Time administration so it’s one week after each COVID-19 vaccine dose
Other Recommendations for Before and After Getting a COVID-19 Vaccine
The guidance also includes these additional pointers to keep in mind for before and after getting the vaccine:
- If you have a non-serious side effect to an earlier dose of a COVID-19 vaccine, you should still get subsequent dose. Serious side effects include a severe (anaphylactic) allergic reaction. Non-serious side effects include symptoms like pain and swelling at the injection site, fever, chills, fatigue, and headache. They should go away within a few days.
- After you get vaccinated, continue to follow the same public health rules (such as wearing a mask, social distancing, washing your hands, avoiding gatherings and crowds). You shouldn’t change your prevention behaviors just because you’re vaccinated, including after the third dose.
- People in your household and close contacts should get vaccinated to create a “cocooning” effect, which may help keep you even safer.
- Autoimmune and inflammatory arthritis patients on immunosuppressant or immunomodulatory medication who have a known exposure to COVID-19 should consider monoclonal antibody treatment preventively to reduce their risk of severe COVID-19. This treatment is newly approved for preventing COVID-19 in people who are immunocompromised once they know they’ve been exposed. It applies whether you’re vaccinated or not.
How the Guidance Was Created
The guidance was developed by a task force of nine rheumatologists, two infectious disease specialists, and two public health experts who currently or previously worked at the U.S. Centers for Disease Control and Prevention (CDC). The group meets regularly to review what new data is available and build consensus to issue recommendations that have either a “strong” or “moderate” level of agreement.
However, the guidance acknowledges that there’s a lot of variability among patients because of differences in underlying health conditions, disease severity, medications, and co-occurring medical issues, which makes it critical to individualize decisions.
Note that the guidance is:
- Based on current knowledge and will be updated as more information comes out
- Meant to be individualized for patients and used as part of shared decision-making with your own doctor.
In other words, the guidance provides considerations to help doctors and patients make decisions about the COVID-19 vaccine — and potential modifications to medications — but there’s not enough data to consider these recommendations gospel.
Get Free Coronavirus Support for Chronic Illness Patients
Join the Global Healthy Living Foundation’s free COVID-19 Support Program for chronic illness patients and their families. We will be providing updated information, community support, and other resources tailored specifically to your health and safety. Join now.
COVID-19 Vaccine Clinical Guidance Summary for Patients with Rheumatic and Musculoskeletal Disease. American College of Rheumatology. August 19, 2021. https://www.rheumatology.org/Portals/0/Files/COVID-19-Vaccine-Clinical-Guidance-Rheumatic-Diseases-Summary.pdf.
Furer V, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Annals of the Rheumatic Diseases. May 27, 2021. doi: https://doi.org/10.1136/annrheumdis-2021-220647.
Interview with Alfred Kim, MD, PhD, Assistant Professor of Medicine, Pathology, and Immunology at Washington University in St. Louis, Missouri
Interview with Jeffrey Curtis, MD, MPH, Professor of Medicine at the University of Alabama at Birmingham
Interview with Michael Putman, MD, Assistant Professor at the Medical College of Wisconsin.
Interview with Rebecca Sadun, MD, MPH, Assistant Professor of Medicine at Duke University