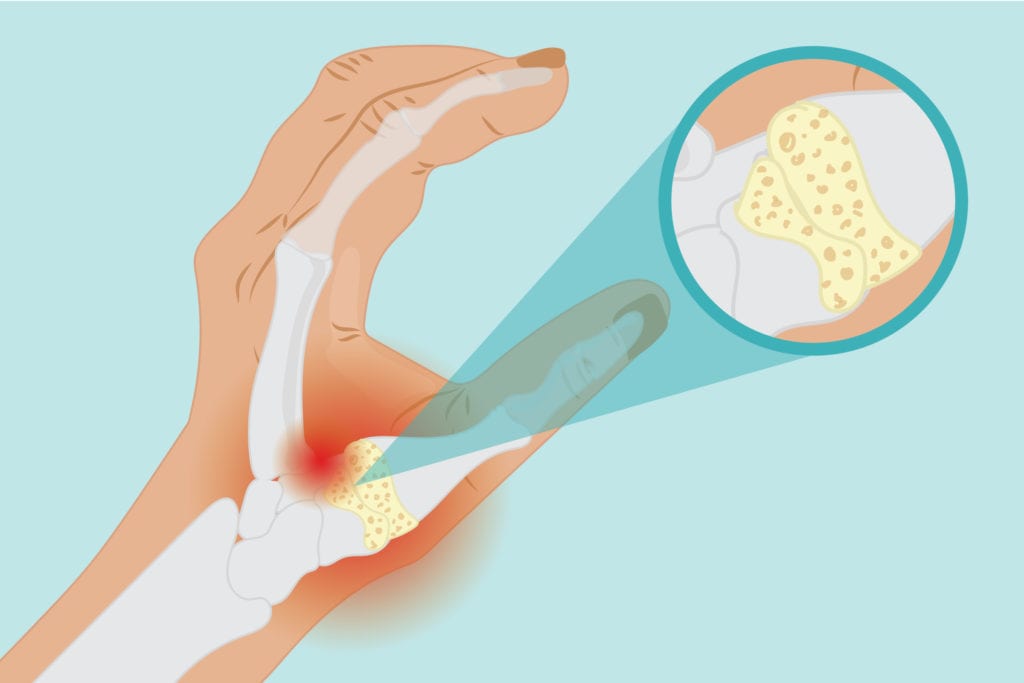
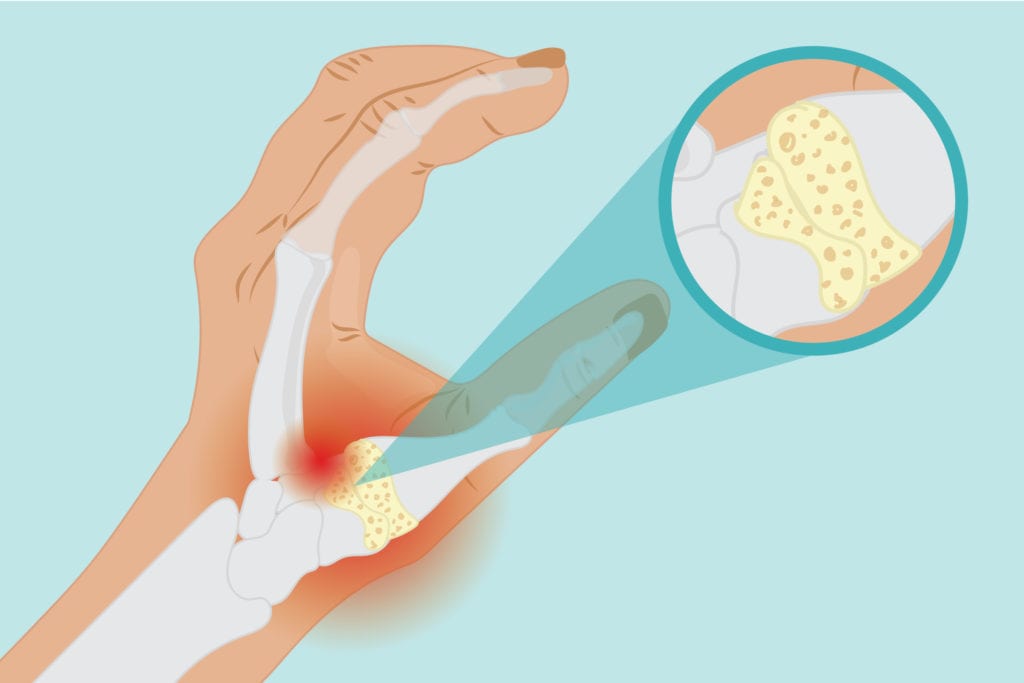
Just as wear and tear can occur in the joints in the knees and hips, cartilage in the hands can wear down over time. Over time, the cartilage at the base of the thumb could break down and become inflamed, starting to show signs of a condition called basal joint arthritis: arthritis of the thumb. The condition is painful and can make everyday activities harder. Recognizing and treating basal joint arthritis is the first step to helping ease the pain.
Basal Joint Arthritis Symptoms
Pain at the thumb is often the first basal joint arthritis symptom. The pain can occur in different forms. For some people, it will be a dull, constant ache; in others it might be a sharp pain that only hits when you use the thumb, says Saakshi Khattri, MD, assistant professor of rheumatology and dermatology at the Icahn School of Medicine in New York City. The pain is most likely to hit when you pinch or strain the basal joint, like when zipping a jacket or opening a jar, she says.
There could be swelling at the base of the thumb too, and people with basal joint arthritis might also notice their thumb loses mobility and gets weaker the longer they’ve been dealing with the pain. “People try to avoid doing certain motions that stress that joint,” says Dr. Khattri. “With time, what you see is wasting of the muscle at the base of the thumb.”
Arthritis of the thumb can feel similar to other hand conditions. Doctors will need to rule out carpal tunnel syndrome (which is caused by pinched nerves in the wrist and can affect the thumb and first three fingers) and de Quervain’s tenosynovitis (a thumb condition also caused by repetitive movements, but it affects the tendons rather than the joints) before settling on basal joint arthritis.
Basal Joint Arthritis Causes and Risk Factors
Wear and tear cause basal joint arthritis, so it’s most common among adults over the age of 40, according to the American Academy of Orthopaedic Surgeons. It’s a common condition, but certain people are more at risk of developing basal joint arthritis. Jobs and activities that require repetitive hand movement, such as factory work and sewing, wear the thumb cartilage down quicker. Women are more prone to thumb arthritis than men, partially because women historically do more work around the house that requires those small joints, says Folashade Alade, MD, a rheumatologist for Piedmont Physicians Group in Georgia.
Injuries to the area can also make the hand more vulnerable to thumb arthritis later in life. “When you have any trauma, it changes the actual architecture of the joint,” says Dr. Khattri. Over time, that could contribute to the cartilage wearing down.
How Doctors Diagnose Basal Joint Arthritis
Primary care doctors can diagnose basal joint arthritis, but they might also refer patients to a specialist such as a rheumatologist or orthopedic surgeon. The doctor will do a clinical exam, asking about a patient’s history and examining the thumb. Swelling at the base is “a dead giveaway,” says Dr. Khattri. Your doctor will also press the area. Tenderness suggests inflammation.
The physical exam could also include a “grind test,” says Dr. Alade. “You pull and then push at the base of the thumb, and you can almost hear the grind,” she says.
Those physical tests can usually clinch a diagnosis of basal joint arthritis, though doctors might also order an X-ray to check for cartilage damage or bumps of bone.
Treatment for Basal Joint Arthritis
OTC pain medications are the first-line treatment for easing the pain of basal joint arthritis, but there are other options too. During activities that involve a lot of thumb movement, patients can wear a spica splint, which goes around the wrist and thumb to keep the joint stable. A physical therapist can also teach people with basal joint arthritis how to do thumb exercises to avoid aggravating the condition.
When OTC meds aren’t enough, a doctor might recommend getting corticosteroid injections every few months, which ease the pain by reducing inflammation of the joint.
Some physicians might also consider injecting hyaluronic acid, a fluid that those with osteoarthritis lose, which is thought to contribute to joint pain. The injections are FDA-approved for large joints but not the thumb, though the off-label use could provide relief for basal joint arthritis too.
If all else fails and excruciating pain from basal joint arthritis still gets in the way of everyday life, surgery is an option. Fusing, repositioning, or removing the joint could help provide more lasting relief.
For those looking for extra pain relief in addition to what the medicine cabinet can offer, massage, acupuncture, and wax therapy (a soothing bath of heated wax) can be helpful too, says Dr. Alade. “All of those things make a difference,” she says.





