By now you know that rheumatoid arthritis (RA) is an autoimmune or inflammatory condition — your immune system has gone haywire and mistakenly attacked your joints. But like many inflammatory arthritis conditions, RA is considered a systemic disease. That means your hyped-up immune system can damage other parts of the body, including your skin.
Jiha Lee, MD, a rheumatologist and Assistant Professor of rheumatology at the University of Michigan Medical School, Ann Arbor, MI, urges patients to be aware of skin changes. “So if they notice nodules [for instance], bring it to [my] attention and pay attention to changes over time, so that we can appropriately manage them.”
Some skin problems are more serious than others and can be caused by the disease itself or from the medications you take to manage RA. You may not have any issues with your skin at all. One 2015 study found that only 26 percent of RA patients have some kind of skin change. But even if it affects a minority of RA patients, those who have skin problems tend to have more severe cases of RA, researchers from Dartmouth found.
Skin Problems Related to RA
Here are some common skin problems to watch for and address with your health care provider if they happen to you.
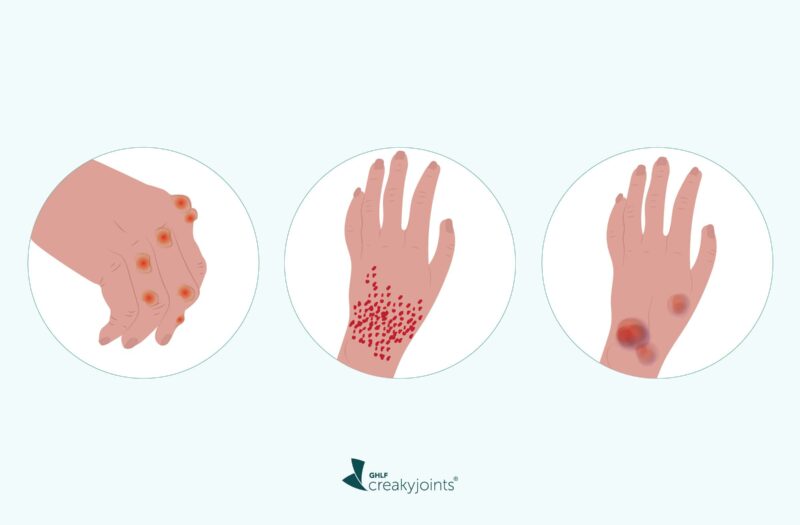
Rheumatoid nodules
This is the most common skin change in RA patients, says Dr. Lee, affecting roughly one in four patients. Nodules tend to occur in patients with seropositive RA, meaning they have either rheumatoid factor (RF) or anti-CCPs, the antibodies that inflame your joints.
What they look like: Nodules are flesh-colored lumps just under the skin. They can be soft or firm, and can get fairly large (lemon-sized). “They occur in more of the pressure point areas,” says Dr. Lee, including the fingers, elbows, and forearms. Nodules can also grow on the feet and even in your lungs.
Are they serious? Most of the time nodules are painless and fairly small — but they can interfere with how well you move your hands or fingers. In some case, they can damage a nerve. If nodules become infected, form ulcers (a round open sore on the skin), or are very painful, a rheumatologist will send you to a dermatologist to get a biopsy, says Dr. Lee. You should also speak up if your nodules are large and making you self-conscious.
How they’re treated: Doctors will leave rheumatoid nodules alone if they’re small or growing slowly. But if they’re painful or affecting your mobility or growing very fast, then rheumatologists may take you off of the RA drug methotrexate, which can boost their growth. “About 70 percent of the time if patients stop taking the methotrexate, the nodules will regress over months,” says Dr. Lee.
Your rheumatologist will probably collaborate with a dermatologist on other treatments for nodules, including steroid injections into the nodule itself, which can decrease its size, or surgical removal, especially if they’re infected or have ulcers.
While rheumatoid nodules are common, “we’re trying to discover them early and getting more aggressive with early treatment,” says Dr. Lee, “so we haven’t seen to the degree of development or burden of rheumatoid nodules that’s previously been reported.”
Rheumatoid vasculitis
When you have RA, your blood vessels (especially the smaller ones) can become inflamed too. This is called rheumatoid vasculitis (RV), and it’s thankfully rare, affecting one percent or one in 100 RA patients, says Dr. Lee.
What it looks like: Usually, you’ll have a red or purplish rash on your legs. In more serious cases, you’ll have sores or purple lesions on your legs and fingers or large ulcers on your legs, says Betsy Furukawa, MD, a dermatologist at Loma Linda University Health, in Loma Linda, CA.
Is it serious? RV can affect other parts of the body — like the kidneys, lungs, or brain — resulting in muscle weakness, chest pains, or tingling or numbness in the fingers or toes, says Dr. Lee. In more advanced cases, RV can cause life-threatening complications like strokes or heart attacks.
How it’s treated: As soon as you see any kind of rash, but especially purple bumps or sores, let your doctor know, suggests Dr. Furukawa. You’ll be sent to a dermatologist who will biopsy the tissue to determine if it’s RV.
How it’s treated depends on whether the disease is widespread. If it’s confined to a small area (like the fingers), doctors will give you steroids. If you have more severe symptoms (like leg ulcers and chest pains), doctors will give you an immunosuppressant, either methotrexate or IV infusions of rituximab, says Dr. Lee.
Neutrophilic dermatosis
“Neutrophilic dermatosis is quite rare; found in patients who have very severe disease,” Dr. Lee notes. While it affects women more than men, slightly less than one percent of patients get these types of skin conditions. There are several different types, but what they have in common is that the rashes have dense concentrations of white blood cells (known as neutrophils), but without any sign of infection.
What it looks like: Sometimes you have plaques — raised patches of skin — on your legs, chest, or face. Other times you may have a large, inflamed wound on your lower leg or a persistent rash that doesn’t go away, says Dr. Furukawa. You may have pus on these wounds or they can just look like purplish raised bumps.
Is it serious? Neutrophilic dermatosis can go away on its own, surprisingly, but it can also become aggressive, affecting other parts of your body like your eyes. They can also cause tissue death at the edges of these angry, inflamed wounds.
How it’s treated: First, you’ll need a diagnosis. “Any new rash, especially one that’s persistent or doesn’t go away quickly, would need expert evaluation,” says Dr. Furukawa, noting that a biopsy from a dermatologist is often required for diagnosis and to guide treatment.
“There’s a long list of therapies because there aren’t great studies on what works for these conditions, and that’s in part because they’re thankfully pretty rare,” says Dr. Furukawa. Treatment may include the following:
- High doses of oral steroids
- Topical steroids creams
- Hydroxychloroquine
Skin Problems Related to Medications
Non-specific skin conditions are actually more common for rheumatoid arthritis, says Dr. Furukawa, and it’s good to know about them so you can contact your doctor if you notice these changes.
Fragile skin and easy bruising
“A lot of times patients will mention they have easy bruising — and a lot of times that’s related to medications that can increase the risk of bleeding as well as lead to thrombocytopenia [a disease that causes platelets to drop],” explains Dr. Lee. Steroids can weaken your blood vessels, especially if you’re older and have been on them for a while, but methotrexate and some biologics can also cause a drop in platelets.
What it looks like: Your skin will be thinner, bruise easily, and be more prone to cuts and scratches, says Dr. Furukawa. “The skin also tends to be very dry. If your fingers swell, you might notice that the skin there is especially tight and thin and bruises easily,” she says, adding that some patients also notice ridges in their nails.
Is it serious? It’s mostly annoying, but your doctor will probably check your platelet count to make sure it doesn’t get dangerously low.
How it’s treated: Protection is key, says Dr. Furukawa. “For example, if you go out and do yard work, you need to put gloves on because you wouldn’t want to get excessive cuts or bruising,” she says. Also important, Dr. Furukawa notes, moisturizing. Apply lotion on the hands every time they get wet.
Sun sensitivity
This is another medication-related skin issue, says Dr. Lee, especially if you take Plaquenil and minocycline. Methotrexate can also cause sun sensitivity, but usually only on areas where you’ve already had a bad sunburn.
What it looks like: Your skin gets burned or darker in areas, or you can get a rash.
Is it serious? It can be painful.
How it’s treated: Prevention is key: Stay in the shade, wear long sleeves and hats, and use sunscreen, say experts.
Skin cancer
“TNF inhibitors like Humira increase your risk of skin cancer over time, even though they don’t make patients photosensitive,” says Dr. Furukawa, who often sees RA patients with squamous and basal cell carcinomas, the most common forms of skin cancer.
What it looks like: Basal cell carcinomas can look like pink or dark bumps, and sometimes ooze if they get big. Squamous cell carcinomas look like sores.
Is it serious? Both kinds grow slowly, but left untreated, they can grow into the layers of the skin and even the bone.
How it’s treated: Again, prevention is your best bet, which is why it’s important to have a dermatologist you trust if you’re taking TNF inhibitors. “We do recommend that patients on these medications get skin exams every year — and, of course, let their doctor know if they have any new or changing skin lesions,” says Dr. Furukawa. If the dermatologist does find either type of cancer, you’ll get it surgically removed.
Whenever you find a rash or bump, take a photo to show or send to your rheumatologist. “Oftentimes when you come to a doctor’s office, the rashes are gone or things have changed,” says Dr. Lee. Photographs provide a record and the doctor can see how things change over time. “My patients often send me a photo over the portal and that way we can consult with the dermatologist, if needed,” she adds.
The bottom line: Reach out to your rheumatologist if you notice any skin irregularities. “The good news is that most patients with RA don’t get things like large leg wounds,” says Dr. Furukawa, “but they do have the potential, so it’s important to be aware and [take steps] to protect their skin.”
American College of Rheumatology. Rheumatoid Arthritis. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Rheumatoid-Arthritis.
American Osteopathic College of Dermatology, “Rheumatoid Nodules.” https://www.aocd.org/page/RheumatoidNodules.
Daniel A, et al. Dermatologic manifestations of rheumatoid arthritis. Rheumatology. 2015. doi: https://doi.org/10.4172/2161-1149.1000168.
Interview with Betsy Furukawa, MD, dermatologist, Loma Linda University Health, Loma Linda, CA.
Interview with Jiha Lee, MD, rheumatologist, University of Michigan Health, Ann Arbor, MI.
Prakash B, et al. Cutaneous manifestations of rheumatoid arthritis. Internet Journal of Rheumatology and Clinical Immunology. 2015. doi: https://doi.org/10.15305/ijrci/v3i1/107.
Reumatologia Clinica (2019). “Rheumatoid neutrophilic dermatitis.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7091481/.
U.S. Food and Drug Administration. The Sun and Your Medicine. https://www.fda.gov/drugs/special-features/sun-and-your-medicine.
Vasculitis Foundation. Rheumatoid Vasculitis. https://www.vasculitisfoundation.org/education/forms/rheumatoid-vasculitis/#1545129433813-d79cdfcc-43bd.